Mon, Feb 2, 2026
[Archive]
Volume 16, Issue 49 (2023)
J Med Edu Dev 2023, 16(49): 50-56 |
Back to browse issues page
Ethics code: A-12-1918-1
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Thacker J, Shinde M, Ganjiwale J, Nimbalkar S. A survey to assess the understanding of healthcare research among the Indian undergraduate medical students. J Med Edu Dev 2023; 16 (49) :50-56
URL: http://edujournal.zums.ac.ir/article-1-1768-en.html
URL: http://edujournal.zums.ac.ir/article-1-1768-en.html
1- Department of Pediatrics, Pramukhswami Medical College, Bhaikaka University, Karamsad, Gujarat, India , thackerjigar@yahoo.co.in
2- Central Research Service, Charutar Arogya Mandal, Bhaikaka University, Karamsad, Gujarat, India
3- Department of Neonatology, Pramukhswami Medical College, Bhaikaka University, Karamsad, Gujarat, India
2- Central Research Service, Charutar Arogya Mandal, Bhaikaka University, Karamsad, Gujarat, India
3- Department of Neonatology, Pramukhswami Medical College, Bhaikaka University, Karamsad, Gujarat, India
Keywords: Evidence-based medicine, Critical appraisal, Research methodology, Medical Education, Undergraduate medical curriculum
Full-Text [PDF 410 kb]
(1169 Downloads)
| Abstract (HTML) (2511 Views)
Full-Text: (1171 Views)
Abstract
Background & Objective: The concept of Evidence-Based Medicine (EBM) and critical appraisal should be taught to undergraduate (UG) medical students so that future doctors can confidently assess the trustworthiness of the literature they read. In the current study, the understanding of biomedical research among Indian UG medical students was assessed.
Material & Methods: The Cross-sectional survey questionnaire as a Google form was circulated via online mode (WhatsApp, e-mail) in December 2020. Any UG medical students including interns from India could voluntarily participate. We aspired to get more than 601 responses as this was the minimum sample size calculated for our study, but we analyzed 715 responses. The questions of this self-made questionnaire were framed for assessing participants' attitudes and knowledge about healthcare research, EBM, and critical appraisal. The data were descriptively analyzed in frequency percentage. Chi2 tests were used to compare the association between categorical variables.
Results: Almost equal participation from all grades of the MBBS study, with almost equal gender distribution, and the mean (SD) age of the participants was 21.09(2.06) years. 22% wanted to do their post-graduation (PG) abroad. 59% surfed the internet for new subject knowledge. Teachers have never asked to refer to any journal for 66%. 14% have read journal articles at least once, with half of the understanding. No difference in biostatistics knowledge before and after its curricular teaching in Third MBBS part 1. Foreign PG aspirants were taking part in research activities more. 46% wanted to do training in critical appraisal, and 43% believed not having critical appraisal skills will affect their patient care.
Material & Methods: The Cross-sectional survey questionnaire as a Google form was circulated via online mode (WhatsApp, e-mail) in December 2020. Any UG medical students including interns from India could voluntarily participate. We aspired to get more than 601 responses as this was the minimum sample size calculated for our study, but we analyzed 715 responses. The questions of this self-made questionnaire were framed for assessing participants' attitudes and knowledge about healthcare research, EBM, and critical appraisal. The data were descriptively analyzed in frequency percentage. Chi2 tests were used to compare the association between categorical variables.
Results: Almost equal participation from all grades of the MBBS study, with almost equal gender distribution, and the mean (SD) age of the participants was 21.09(2.06) years. 22% wanted to do their post-graduation (PG) abroad. 59% surfed the internet for new subject knowledge. Teachers have never asked to refer to any journal for 66%. 14% have read journal articles at least once, with half of the understanding. No difference in biostatistics knowledge before and after its curricular teaching in Third MBBS part 1. Foreign PG aspirants were taking part in research activities more. 46% wanted to do training in critical appraisal, and 43% believed not having critical appraisal skills will affect their patient care.
Introduction
Practicing Evidence-Based Medicine (EBM) depends upon careful clinical decision-making based on high-quality evidence from Randomized Control Trials (RCT) and observational studies (1,2). In the recent era, the exponential output of medical literature each year makes it harder to find reliable evidence (3). The results and conclusions of any of the studies cannot be directly applied to the practice. One needs to analyze the study objective, soundness of the study design, and research methodology. Then to assess the internal and external validity of the study results within the context of own patient profile (4). To do so, the clinician needs to have the ability to critically appraise the scientific material presented to them. Critical appraisal is the process of carefully and systematically examining the research article to judge its trustworthiness, value, and relevance in a particular context (5). The skills of searching, reading, and critically appraising the medical literature have to be seeded right from undergraduate (UG) medical education for enabling a future clinician to utilize information independently and appropriately for better healthcare outcomes (2,6). Traditionally, formal teaching on critical appraisal was far way apart in a packed medical curriculum. But, a lack of formal instruction on critical appraisal compromises junior doctors' ability to interpret clinical research adequately (6,7).
We have limited data from India demonstrating medical undergraduate or postgraduate (PG) students' interest or ability toward biomedical research or critical appraisal (8). Epidemiology and biostatistics are being taught in the Third MBBS Part 1 under the subject of Preventive and Social Medicine (P&SM). Though, no formal teaching exists for research methodology or critical appraisal skills. With the drastic change, a new undergraduate medical curriculum, Competency-Based Medical Education was introduced in India in 2019. The new curriculum focuses more on the integration of subjects and skill development rather than mere subject knowledge. Due importance is given to Self-directed learning (9). Unfortunately, it appears, even new curricula do not focus enough on critical appraisal ability among undergraduates to make them practice Evidence Based Medicine self-confidently. In our institute, two days workshop on research methodology is being conducted annually for the last many years, primarily focusing on newly entered postgraduates for their thesis preparedness. Increasingly, interested undergraduates are also taking part. Being an aspirant for the United States Medical Licensing Exam (USMLE), some undergraduates take part in research activities to get this reflected in their resumes. In a welcome move, the Basic Course in Biomedical Research is now mandatory for postgraduate and medical faculty in any stream. This is a uniform research methodology course across the nation offered by the Indian Council of Medical Research - National Institute of Epidemiology (ICMR-NIE), Chennai in an online mode. However, the course is not meant for undergraduate medical students (10).
In this survey, we aim to assess the current level of understanding of healthcare research among Indian undergraduate medical students. This may lead to a path forward in imparting knowledge and skill of critical appraisal among undergraduates with required system changes.
Material & Methods
Design and setting (s)
This cross-sectional survey was conducted on undergraduate medical students doing their Bachelor of Medicine, Bachelor of Surgery (MBBS) course in India during the month of December 2020.
Participants and sampling
Any undergraduate student who is currently pursuing his MBBS course in India, in any year of their study including interns could take part in the survey, with no exclusion criteria. They were asked for their voluntary participation. The preface to the form described the purpose of the study and how would be their responses evaluated. The proposed benefit of the study to medical science and medical education was mentioned. Sample size calculation was based on the assumption of 50% of students knowing critical appraisal of research articles, taking 4% as our acceptable difference for the estimation at a 95% confidence level, the minimum estimated sample size calculated was 601. This being an estimation problem, we went beyond 601 for collecting responses.
Tools and Data collection methods
The survey questionnaire had a total of 31 questions, out of which the first was the participants’ e-mail asking for identification, and the second question was their agreement to participate which was considered as their implied consent. Apart from an e-mail, no other identifier was asked, neither the name nor the college they are studying in. The remaining 29 core survey questions were asked sequentially but divided under different headings during analysis. The participants did not need to attempt all the survey questions. They may attempt a question or not based on their understanding. Questions no. 6, 16, 28, and 31 were not analyzed as later on found to have low contribution toward the study objectives. Most of the questions were the closed-answered type with choosing the best possible or all applicable options. Four questions required a brief description included, 1) Name any four journals, 2) Name any four components of the original article, 3) Describe the difference between original and review articles briefly in two lines, and 4) Importance of p-value. The answers to these questions were not tough to evaluate. Two of the authors evaluated the answers with prior consensus between them. The number-percentage of correctly described answers was taken into consideration. Eight questions (questions no. 15-22) were meant for the participants who had read the journal article/s at least once to check their understanding. While analyzing three questions (questions no. 25, 26, 27), the existing participants of this cross-sectional survey were divided into two groups, before and after receiving the formal classroom education of biostatistics in the Third MBBS part 1. These questions were from the standard curriculum, and we wanted to know whether the understanding of the two groups is different, or whether the after group had a better understanding. Participants having any sort of research experience (question no. 23) were compared based upon their PG preferences – India or abroad (question no. 8). Authors, with their vast experience in the field of medical education and healthcare research, developed the survey questionnaire after a thorough literature review (3,6,11). To check for any ambiguity in understanding of the questions, a pilot survey had been conducted with ten departmental post-graduate students, and two questions were re-framed to bring more clarity to the respondents before the final version was circulated. The content validity index of the final questionnaire so developed was calculated with 4 experts’ opinions on the content. The four experts agreed on including all the questions put in the questionnaire. Apart from basic details and demographics questions, the minimum content validity index (CVI) calculated was 0.75 for 4 questions (3 out of 4 experts said the questions to be very relevant while none said not relevant) whereas all the rest of the 16 questions scored 1 for CVI. The overall CVI for the questionnaire was 0.95 meaning a good content validity for the tool.
Data analysis
Descriptive statistics [Frequency (%), mean (SD)] were used to portray the baseline characteristics of the participants and to assess their understanding of healthcare research. Chi2 tests were used to compare the association between categorical variables.
Results
We got a total of 784 responses. 10 participants had not given their agreement and after removing the duplicates, finally, we analyzed 715 responses. Table 1 depicts the basic demographic profiles of the participants with their post-graduate preferences (India or abroad).
Table 2 is dealing with the questions about participants' basic awareness, exposure, and incline toward journals and healthcare research. We got interesting findings here. 59% of participants surfed the internet for seeking any new information on the medical subject, and the least, only 7% asked their teachers. For 66% of the participants, teachers or mentors have never asked to read any journals. 103 (14.40%) students agreed to have read any journal article at least once, and only 24 (3.36%) named any four journals correctly.
For the 103 participants who have read journal articles at least once, a different set of questions were asked to assess their understanding, as mentioned in Table 3. It contains questions for assessing their knowledge objectively apart from self-proclaimed abilities. 57 participants believed they understand the difference between original and review articles, while 45 could describe it correctly.
Table 4 includes the curricular questions related to biostatistics and study design, what is supposed to be taught in the Third MBBS part 1, under the Preventive and community medicine subject. We compared the students before this formal teaching (I, II, and III/I MBBS) and after (III/II MBBS and interns). No difference was found between the before and after groups on the biostatistics questions related to the p-value and 95% confidence interval. Though, a significant number of the students from the after group could answer two out of three correct options for a question on study design.
77 (10.77%) participants agreed to have some research experience, either participating as a co-investigator or doing data collection (Table 2). Participants having research experience were compared based on their PG preferences – India or abroad. 18.79% of abroad PG aspirants had research experience compared to 9.39% of Indian PG aspirants, and this difference is statistically significant. (P-value = 0.015) (Figure 1).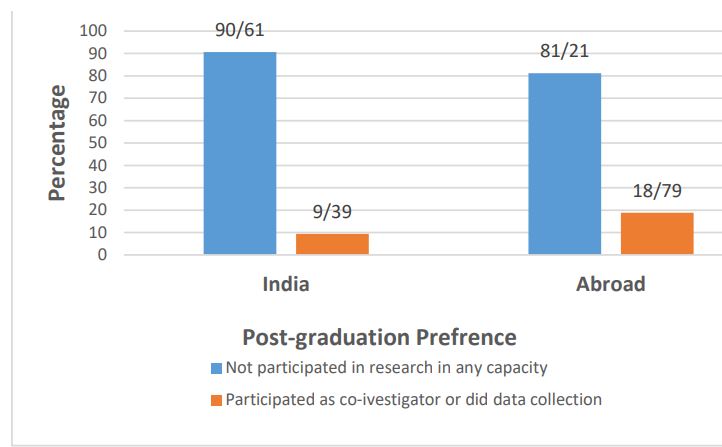
Figure 1. Bar diagram showing participation in research activities as per their post-graduation preferences
Discussion
To the best of our knowledge, this would be the first of its kind of study assessing the understanding of healthcare research among undergraduate medical students from India. Students from an early phase of their studies have also participated equally. A considerable proportion of participants wanted to do their post-graduation abroad. This can have an implication and can influence the study results, because an aspirant for Westernized countries may need to show some sort of research experience. Most students depend on the internet for new information, and the internet is a full mix of information with varied authenticity and diverse content and context. Thus, it is imperative for students to have the good critical appraising ability. Here, it also suggests the 'distance' between the medical teachers and the students, as only 7% were comfortable asking their teachers for seeking new information. 30% of participants reported that they do not have access to the journal (electronic or print) in their institute. We can understand, these participants were unaware of the journal access their library may have. Disturbingly, only 3% of participants know the name of any four journals correctly, and only for 34% of the participants their teachers or mentors have ever asked to refer to a journal. This is a clear lack of motivation.
It seems that participating students were not informed convincingly about the importance of EBM and the necessity to remain updated with the emerging evidence and critically appraising this new information. This is because despite poor performance only 46% were eager to have some training in critical appraisal of medical literature, and only 43% believed that not understanding critical appraisal will affect their patient care. A similar result was found from an Indian experience where 27% of the students were not convinced of the relevance of the EBM to UG studies (12), while in the Swiss survey importance of teaching and knowledge of EBM was rated high (13). Lack of good understanding of basic research methodology, poor interpretation of method and result, as well poor confidence in critically appraising an article was reported among medical students (11,14). Some of the impediments to EBM practice as identified by the students were time constraints, ignorance, missing practical relevance, and lack of training among others (13).
Improvement was demonstrated in medical students' self-reported confidence in critical appraisal skills after a half-day journal club session (3). Two-day mixed method interactive workshop not only augmented subjective confidence but quiz answers for 15 questions were also improved significantly (6). In this cross-sectional study, students were divided into the before and after receiving the formal education of biostatistics and study designs in Third MBBS part 1 on the questions from the curriculum. Surprisingly, no difference was found for the statistical questions on describing p-value and 95% confidence interval range. Though, significant numbers of the students from the after group could answer that causation can be inferred from cohort study or cohort and RCT both. In another study, third-year undergraduates after a short course on EBM were compared on their critical appraisal ability of RCTs with the experts. There was poor agreement and significant non-systemic over and under-estimation was found (15). This suggests, there cannot be a short-term solution and efforts should be placed on the systemic inclusion of biomedical research education and critical appraisal in the medical curriculum (11). Recently, several academic investigators have attempted so. A 5-weeks EBM module including lectures, workshops, and online search sessions was conducted over 52 fourth-year UG medical students and found effective in improving their knowledge and skills in EBM (16). In India, simulated RCT was designed and delivered to medical students for improving their EBM and critical appraisal skills (17). Team-based learning and group discussion methods were compared for teaching critical appraisal to a large class of UG medical students (18).
There are limitations of this survey. The sample may not be representative of the entire country, and over-representation from our region or home institute is likely. Obviously, we could have multiple social online penetration opportunities regionally to propagate the survey links than in the out far regions. As the survey did not ask for participants' college names for maintaining anonymity, we were unable to draw regional representation. It is possible in any online survey that some of the answers might have been googled. In strength, this survey got a large number of participants, averaging the unnoticed biases. We did not find any standard questionnaire suitable for our objective. So, we developed the questionnaire taking into account the regional trends in undergraduate medical education. Other researchers across the globe can validate our questionnaire with the necessary modification. This study fairly represents the temperament of Indian medical UG students toward biomedical research, critical appraisal, and EBM. In the future, we are planning to undertake a similar survey on the medical teachers to understand their attitude and readiness to inoculate EBM in the medical curricula. Further interventional studies are necessary for assessing the suitable options for fulfilling this lacuna in medical education.
Conclusion
Indian UG student lacks an understanding of healthcare research and even the importance of EBM is not well perceived. There is also insufficient motivation from medical teachers and a non-inclusive curriculum. Systematic curricular changes are warranted to impart an understanding of EBM, healthcare research, and critical appraisal among UG students in India.
Ethical consideration
The Institutional Ethics Committee approved the study with reference no. IEC/ HMPCMCE/ 125/ Faculty/ 7/ Date: 24/10/2020. A survey questionnaire was created as a Google form. The link to the form was circulated via various online modes, including WhatsApp, and e-mail across the MBBS students of different regions.
Disclosure
None of the authors has to declare any financial or other conflicts of interest.
Author contributions
Jigar P. Thacker, Jaishree Ganjiwale, and Somashekhar Nimbalkar have conceptualized the study and developed the study protocol and survey questionnaire. Jaishree Ganjiwale analyzed the initial responses; Jigar Thacker and Mayur Shinde evaluated the response. Mayur Shinde has done the statistical analysis.
Jigar Thacker has drafted the manuscript, with Mayur K. Shinde helping in manuscript editing and revision.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Data availability statement
The raw data-sheet can be available from the corresponding author upon reasonable request.
Practicing Evidence-Based Medicine (EBM) depends upon careful clinical decision-making based on high-quality evidence from Randomized Control Trials (RCT) and observational studies (1,2). In the recent era, the exponential output of medical literature each year makes it harder to find reliable evidence (3). The results and conclusions of any of the studies cannot be directly applied to the practice. One needs to analyze the study objective, soundness of the study design, and research methodology. Then to assess the internal and external validity of the study results within the context of own patient profile (4). To do so, the clinician needs to have the ability to critically appraise the scientific material presented to them. Critical appraisal is the process of carefully and systematically examining the research article to judge its trustworthiness, value, and relevance in a particular context (5). The skills of searching, reading, and critically appraising the medical literature have to be seeded right from undergraduate (UG) medical education for enabling a future clinician to utilize information independently and appropriately for better healthcare outcomes (2,6). Traditionally, formal teaching on critical appraisal was far way apart in a packed medical curriculum. But, a lack of formal instruction on critical appraisal compromises junior doctors' ability to interpret clinical research adequately (6,7).
We have limited data from India demonstrating medical undergraduate or postgraduate (PG) students' interest or ability toward biomedical research or critical appraisal (8). Epidemiology and biostatistics are being taught in the Third MBBS Part 1 under the subject of Preventive and Social Medicine (P&SM). Though, no formal teaching exists for research methodology or critical appraisal skills. With the drastic change, a new undergraduate medical curriculum, Competency-Based Medical Education was introduced in India in 2019. The new curriculum focuses more on the integration of subjects and skill development rather than mere subject knowledge. Due importance is given to Self-directed learning (9). Unfortunately, it appears, even new curricula do not focus enough on critical appraisal ability among undergraduates to make them practice Evidence Based Medicine self-confidently. In our institute, two days workshop on research methodology is being conducted annually for the last many years, primarily focusing on newly entered postgraduates for their thesis preparedness. Increasingly, interested undergraduates are also taking part. Being an aspirant for the United States Medical Licensing Exam (USMLE), some undergraduates take part in research activities to get this reflected in their resumes. In a welcome move, the Basic Course in Biomedical Research is now mandatory for postgraduate and medical faculty in any stream. This is a uniform research methodology course across the nation offered by the Indian Council of Medical Research - National Institute of Epidemiology (ICMR-NIE), Chennai in an online mode. However, the course is not meant for undergraduate medical students (10).
In this survey, we aim to assess the current level of understanding of healthcare research among Indian undergraduate medical students. This may lead to a path forward in imparting knowledge and skill of critical appraisal among undergraduates with required system changes.
Material & Methods
Design and setting (s)
This cross-sectional survey was conducted on undergraduate medical students doing their Bachelor of Medicine, Bachelor of Surgery (MBBS) course in India during the month of December 2020.
Participants and sampling
Any undergraduate student who is currently pursuing his MBBS course in India, in any year of their study including interns could take part in the survey, with no exclusion criteria. They were asked for their voluntary participation. The preface to the form described the purpose of the study and how would be their responses evaluated. The proposed benefit of the study to medical science and medical education was mentioned. Sample size calculation was based on the assumption of 50% of students knowing critical appraisal of research articles, taking 4% as our acceptable difference for the estimation at a 95% confidence level, the minimum estimated sample size calculated was 601. This being an estimation problem, we went beyond 601 for collecting responses.
Tools and Data collection methods
The survey questionnaire had a total of 31 questions, out of which the first was the participants’ e-mail asking for identification, and the second question was their agreement to participate which was considered as their implied consent. Apart from an e-mail, no other identifier was asked, neither the name nor the college they are studying in. The remaining 29 core survey questions were asked sequentially but divided under different headings during analysis. The participants did not need to attempt all the survey questions. They may attempt a question or not based on their understanding. Questions no. 6, 16, 28, and 31 were not analyzed as later on found to have low contribution toward the study objectives. Most of the questions were the closed-answered type with choosing the best possible or all applicable options. Four questions required a brief description included, 1) Name any four journals, 2) Name any four components of the original article, 3) Describe the difference between original and review articles briefly in two lines, and 4) Importance of p-value. The answers to these questions were not tough to evaluate. Two of the authors evaluated the answers with prior consensus between them. The number-percentage of correctly described answers was taken into consideration. Eight questions (questions no. 15-22) were meant for the participants who had read the journal article/s at least once to check their understanding. While analyzing three questions (questions no. 25, 26, 27), the existing participants of this cross-sectional survey were divided into two groups, before and after receiving the formal classroom education of biostatistics in the Third MBBS part 1. These questions were from the standard curriculum, and we wanted to know whether the understanding of the two groups is different, or whether the after group had a better understanding. Participants having any sort of research experience (question no. 23) were compared based upon their PG preferences – India or abroad (question no. 8). Authors, with their vast experience in the field of medical education and healthcare research, developed the survey questionnaire after a thorough literature review (3,6,11). To check for any ambiguity in understanding of the questions, a pilot survey had been conducted with ten departmental post-graduate students, and two questions were re-framed to bring more clarity to the respondents before the final version was circulated. The content validity index of the final questionnaire so developed was calculated with 4 experts’ opinions on the content. The four experts agreed on including all the questions put in the questionnaire. Apart from basic details and demographics questions, the minimum content validity index (CVI) calculated was 0.75 for 4 questions (3 out of 4 experts said the questions to be very relevant while none said not relevant) whereas all the rest of the 16 questions scored 1 for CVI. The overall CVI for the questionnaire was 0.95 meaning a good content validity for the tool.
Data analysis
Descriptive statistics [Frequency (%), mean (SD)] were used to portray the baseline characteristics of the participants and to assess their understanding of healthcare research. Chi2 tests were used to compare the association between categorical variables.
Results
We got a total of 784 responses. 10 participants had not given their agreement and after removing the duplicates, finally, we analyzed 715 responses. Table 1 depicts the basic demographic profiles of the participants with their post-graduate preferences (India or abroad).
Table 1. Basic demographics of the participants
| Sr. No. | Variable | No. of responses (Total N=715) |
Categories | Frequency (%) |
| 1. | Age (in years) | 701 | Median (Range) | 21(18,28) |
| 2. | Sex | 707 | Female | 370(52.33) |
| Male | 337(47.67) | |||
| 3. | Year of studying | 705 | First MBBS | 131(18.58) |
| Second MBBS | 184(26.10) | |||
| Third MBBS Part 1 | 136(19.29) | |||
| Third MBBS Part 2 | 204(28.94) | |||
| Intern | 50(7.09) | |||
| 4. | Medium of education in higher secondary school | 703 | English | 503(71.55) |
| Vernacular | 200(28.45) | |||
| 5. | Where will you prefer to do your Post Graduation? | 703 | Abroad | 152(21.62) |
| India | 540(76.81) | |||
| Does not want to do post-graduation | 11(1.56) |
Table 2 is dealing with the questions about participants' basic awareness, exposure, and incline toward journals and healthcare research. We got interesting findings here. 59% of participants surfed the internet for seeking any new information on the medical subject, and the least, only 7% asked their teachers. For 66% of the participants, teachers or mentors have never asked to read any journals. 103 (14.40%) students agreed to have read any journal article at least once, and only 24 (3.36%) named any four journals correctly.
Table 2. Participants’ basic awareness, exposure, and inclination towards healthcare research
| Sr. No. | Variable | Categories | Frequency(%) N=715 |
| 1. | What would be your primary approach to seek new information about your medical subject? | Ask peer or senior | 111(15.52) |
| Ask your Teacher | 53(7.41) | ||
| Refer Book from Library | 117(16.36) | ||
| Surf the internet | 421(58.88) | ||
| No Response | 13(1.81) | ||
| 2. | Have you ever browsed Google Scholar or PUBMED? | Yes | 264(36.92) |
| 3. | Do you have access to journals in any form in your college library? | Electronic Form | 22(3.07) |
| Text form | 228(31.89) | ||
| Both | 219(30.63) | ||
| None | 216(30.21) | ||
| No Response | 30(4.19) | ||
| 4. | Has your Teacher or Mentor ever asked you to refer any journal? | Yes | 241(33.71) |
| 5. | Have you ever read any journal article/s? | Yes | 103(14.40) |
| 6. | Name upto Four Journals you Know | Described four names correctly | 24(3.36) |
| 7. | Have you ever helped a faculty or postgraduate student conducting a research study by any of the following means? | Not Participated | 607(84.89) |
| Only Data Collection | 42(5.87) | ||
| Participated as a co-investigator | 35(4.89) | ||
| No Response | 31(4.33) | ||
| 8. | If answer to above question is "No", are you interested to participate? | Yes | 411(67.71) *N-607 |
| 9. | Are you interested to do some training regarding healthcare research of critical appraisal of the literature? | Yes | 331(46.29) |
| 10. | Do you believe if you don’t have an ability to critically appraise a medical article, will it affect your patient's care? | Yes | 311(43.50) |
For the 103 participants who have read journal articles at least once, a different set of questions were asked to assess their understanding, as mentioned in Table 3. It contains questions for assessing their knowledge objectively apart from self-proclaimed abilities. 57 participants believed they understand the difference between original and review articles, while 45 could describe it correctly.
Table 3. Participants’ understanding about the journal article/s read (103 participants agreed for reading journal article at least once.)
| Sr. No. | Variable | Categories | Frequency (%) |
| 1. | Do you understand the difference between original article and review article? | Yes | 57(55.34) |
| 2. | If Answer to above question is Yes, Describe it briefly in two lines. | Described correctly | 45(78.95) |
| 3. | Name any four component of an original article. | Correctly known | 53(51.45) |
| 4. | For those who have read an article, were you able to evaluate the internal and external validity of the findings presented in the article? | Yes | 21(20.38) |
| 5. | For the study you have read, which is the most important factor for study evaluation or interpretation? | Interpretation of Results | 47(45.63) |
| Sample size | 34(33) | ||
| Journal in which it is published. | 5(4.85) | ||
| Duration of the Study. | 5(4.85) | ||
| Missing | 12(11.65) | ||
| 6. | Were you able to make sense of the statistical analysis done and the interpretations drawn? | Yes | 59(57.28) |
| 7. | About the article(s) you have read, what % you think you could understand it properly. | 0%-50% | 35(33.98) |
| 51%-70% | 25(24.27) | ||
| 71%-90% | 21(20.38) | ||
| >90% | 2(1.94) | ||
| Missing | 20(19.41) |
Table 4 includes the curricular questions related to biostatistics and study design, what is supposed to be taught in the Third MBBS part 1, under the Preventive and community medicine subject. We compared the students before this formal teaching (I, II, and III/I MBBS) and after (III/II MBBS and interns). No difference was found between the before and after groups on the biostatistics questions related to the p-value and 95% confidence interval. Though, a significant number of the students from the after group could answer two out of three correct options for a question on study design.
Table 4. Comparison of knowledge on biostatistics and study design before and after receiving formal education in Third MBBS part 1
| Sr. No. | Variable | Categories | (Before group) Participants from I, II, and III/I MBBS Frequency (%) |
(After group) Participants from III/II MBBS and interns Frequency (%) |
p-value |
| 1. | What is importance of knowing p value? | Correctly Described |
45(48.91) | 42(51.22) | 0.761 |
| Wrongly Described | 47(51.09) | 40(48.78) | |||
| 2. | Causation can be inferred from which of the following study types: Can choose more than one option if applicable. | Cohort | 88(42.51) | 107(62.21) | <0.001 |
| RCT | 75(36.23) | 66(38.37) | 0.668 | ||
| BOTH | 30(14.49) | 40(23.26) | 0.02 | ||
| 3. | In statistical analysis, what range of 95% Confidence Interval is better? | Narrow | 117(62.57 ) | 104(65.41) | 0.583 |
*p-value assessed by chi2 test
77 (10.77%) participants agreed to have some research experience, either participating as a co-investigator or doing data collection (Table 2). Participants having research experience were compared based on their PG preferences – India or abroad. 18.79% of abroad PG aspirants had research experience compared to 9.39% of Indian PG aspirants, and this difference is statistically significant. (P-value = 0.015) (Figure 1).
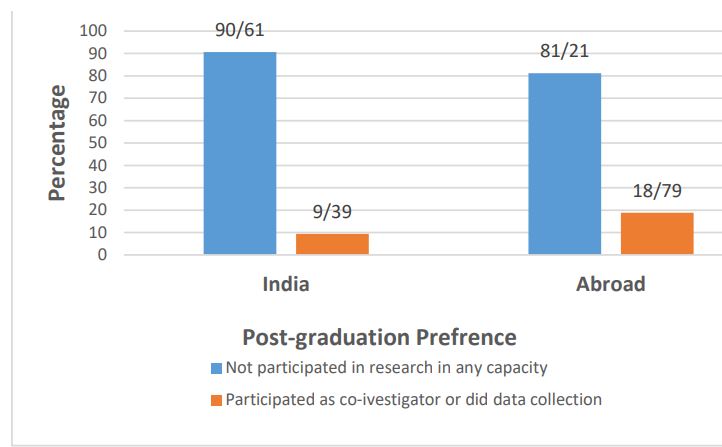
Figure 1. Bar diagram showing participation in research activities as per their post-graduation preferences
Discussion
To the best of our knowledge, this would be the first of its kind of study assessing the understanding of healthcare research among undergraduate medical students from India. Students from an early phase of their studies have also participated equally. A considerable proportion of participants wanted to do their post-graduation abroad. This can have an implication and can influence the study results, because an aspirant for Westernized countries may need to show some sort of research experience. Most students depend on the internet for new information, and the internet is a full mix of information with varied authenticity and diverse content and context. Thus, it is imperative for students to have the good critical appraising ability. Here, it also suggests the 'distance' between the medical teachers and the students, as only 7% were comfortable asking their teachers for seeking new information. 30% of participants reported that they do not have access to the journal (electronic or print) in their institute. We can understand, these participants were unaware of the journal access their library may have. Disturbingly, only 3% of participants know the name of any four journals correctly, and only for 34% of the participants their teachers or mentors have ever asked to refer to a journal. This is a clear lack of motivation.
It seems that participating students were not informed convincingly about the importance of EBM and the necessity to remain updated with the emerging evidence and critically appraising this new information. This is because despite poor performance only 46% were eager to have some training in critical appraisal of medical literature, and only 43% believed that not understanding critical appraisal will affect their patient care. A similar result was found from an Indian experience where 27% of the students were not convinced of the relevance of the EBM to UG studies (12), while in the Swiss survey importance of teaching and knowledge of EBM was rated high (13). Lack of good understanding of basic research methodology, poor interpretation of method and result, as well poor confidence in critically appraising an article was reported among medical students (11,14). Some of the impediments to EBM practice as identified by the students were time constraints, ignorance, missing practical relevance, and lack of training among others (13).
Improvement was demonstrated in medical students' self-reported confidence in critical appraisal skills after a half-day journal club session (3). Two-day mixed method interactive workshop not only augmented subjective confidence but quiz answers for 15 questions were also improved significantly (6). In this cross-sectional study, students were divided into the before and after receiving the formal education of biostatistics and study designs in Third MBBS part 1 on the questions from the curriculum. Surprisingly, no difference was found for the statistical questions on describing p-value and 95% confidence interval range. Though, significant numbers of the students from the after group could answer that causation can be inferred from cohort study or cohort and RCT both. In another study, third-year undergraduates after a short course on EBM were compared on their critical appraisal ability of RCTs with the experts. There was poor agreement and significant non-systemic over and under-estimation was found (15). This suggests, there cannot be a short-term solution and efforts should be placed on the systemic inclusion of biomedical research education and critical appraisal in the medical curriculum (11). Recently, several academic investigators have attempted so. A 5-weeks EBM module including lectures, workshops, and online search sessions was conducted over 52 fourth-year UG medical students and found effective in improving their knowledge and skills in EBM (16). In India, simulated RCT was designed and delivered to medical students for improving their EBM and critical appraisal skills (17). Team-based learning and group discussion methods were compared for teaching critical appraisal to a large class of UG medical students (18).
There are limitations of this survey. The sample may not be representative of the entire country, and over-representation from our region or home institute is likely. Obviously, we could have multiple social online penetration opportunities regionally to propagate the survey links than in the out far regions. As the survey did not ask for participants' college names for maintaining anonymity, we were unable to draw regional representation. It is possible in any online survey that some of the answers might have been googled. In strength, this survey got a large number of participants, averaging the unnoticed biases. We did not find any standard questionnaire suitable for our objective. So, we developed the questionnaire taking into account the regional trends in undergraduate medical education. Other researchers across the globe can validate our questionnaire with the necessary modification. This study fairly represents the temperament of Indian medical UG students toward biomedical research, critical appraisal, and EBM. In the future, we are planning to undertake a similar survey on the medical teachers to understand their attitude and readiness to inoculate EBM in the medical curricula. Further interventional studies are necessary for assessing the suitable options for fulfilling this lacuna in medical education.
Conclusion
Indian UG student lacks an understanding of healthcare research and even the importance of EBM is not well perceived. There is also insufficient motivation from medical teachers and a non-inclusive curriculum. Systematic curricular changes are warranted to impart an understanding of EBM, healthcare research, and critical appraisal among UG students in India.
Ethical consideration
The Institutional Ethics Committee approved the study with reference no. IEC/ HMPCMCE/ 125/ Faculty/ 7/ Date: 24/10/2020. A survey questionnaire was created as a Google form. The link to the form was circulated via various online modes, including WhatsApp, and e-mail across the MBBS students of different regions.
Disclosure
None of the authors has to declare any financial or other conflicts of interest.
Author contributions
Jigar P. Thacker, Jaishree Ganjiwale, and Somashekhar Nimbalkar have conceptualized the study and developed the study protocol and survey questionnaire. Jaishree Ganjiwale analyzed the initial responses; Jigar Thacker and Mayur Shinde evaluated the response. Mayur Shinde has done the statistical analysis.
Jigar Thacker has drafted the manuscript, with Mayur K. Shinde helping in manuscript editing and revision.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Data availability statement
The raw data-sheet can be available from the corresponding author upon reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2022/11/10 | Accepted: 2023/03/5 | Published: 2023/03/27
Received: 2022/11/10 | Accepted: 2023/03/5 | Published: 2023/03/27
References
1. Greenhalgh T, Howick J, Maskrey N; Evidence Based Medicine Renaissance Group. Evidence based medicine: a movement in crisis? BMJ. 2014;13;348- 3725. [DOI]
2. Möller R, Shoshan M. Does reality meet expectations? An analysis of medical students' expectations and perceived learning during mandatory research projects. BMC Medical Eduation. 2019;19(1):93. [DOI]
3. Gokani SA, Sharma E, Sharma T, et. al. Impact of a National Journal Club and Letter Writing Session on Improving Medical Students' Confidence with Critical Appraisal. Advances in Medical Education Practice. 2019;24;10:1081-1087. [DOI]
4. Manjali, Jifmi Jose; Gupta, Tejpal. Critical appraisal of a clinical research paper: What one needs to know. Cancer Research, Statistics, and Treatment. 2020;3(3): 545-551. [DOI]
5. Al-Jundi A, Sakka S. Critical Appraisal f Clinical Research. Journal of Clinical and Diagnostic Research. 2017;11(5): 1-5. [DOI]
6. Lee AE, Ardissino M, Bednarczuk NF, et. al. Prospective assessment of a critical appraisal teaching programme on medical students' confidence and performance in appraising medical literature. Journal of Royal College of Physicians Edinburg. 2020;50(1):60-66. [DOI]
7. Windish DM, Huot SJ, Green ML. Medicine residents' understanding of the biostatistics and results in the medical literature. JAMA. 2007;5;298(9):1010-22. [DOI]
8. Garg R, Goyal S, Singh K. Lack of Research Amongst Undergraduate Medical Students in India: It's time to Act and Act Now. Indian Pediatrics. 2017;15;54(5):357-360. [DOI]
9. Mahajan R, Virk A, Saiyad S, et. al. Stages of Concern of Medical Faculty toward Adoption of Competency-based Medical Education in India: A Multicentric Survey. International Journal of Applied and Basic Medical Research. 2022;12(2):87-94. [DOI]
10. Ponnaiah M, Bhatnagar T, Ganeshkumar P, et. al. Design and implementation challenges of massive open online course on research methods for Indian medical postgraduates and teachers -descriptive analysis of inaugural cycle. BMC Medical Education. 2022;22(1):369. [DOI]
11. Jaunoo S, Adams HL. A Survey Showing the Need to Incorporate the Teaching of Critical Appraisal Skills in the Undergraduate Medical Curriculum. British Journal of Medicine and Medical Research. 2016. [DOI]
12. Basheer A, Iqbal N, Alexander T et al. Introducing a course on Evidence Based Medicine for undergraduate medical students – experience from an Indian medical school. MedEdPublish. 2016; 5:153. [DOI]
13. Kaderli R, Burghardt L, Hansali C, et. al. A Students’ View of Evidence-Based Medicine: A Survey in Switzerland. Archives of Clinical and Experimental Surgery. 2012;1(1):1-7.
14. Hamdan A. Medical students still lack skills needed to practise evidence-based medicine. Journal of Royal Society of Medicine. 2012;105(8):324. [DOI]
15. Buchberger B, Mattivi JT, Schwenke C,et. al. Critical appraisal of RCTs by 3rd year undergraduates after short courses in EBM compared to expert appraisal. GMS Journal of Medical Education. 2018;35(2): 24. [DOI]
16. Al Shahrani AS. Development and evaluation of an evidence-based medicine module in the undergraduate medical curriculum. BMC Medical Education. 2020; 20(1):256. [DOI]
17. Basheer A, Iqbal N, Prabakaran S, et. al. Simulated Randomized Controlled Trial to Learn Critical Appraisal (SiRCA): A Randomized Controlled Study of Effectiveness Among Undergraduate Medical Students. Cureus. 2021; 1113(11):e19946. [DOI]
18. Daou D, Chakhtoura M, El-Yazbi A, et. al. Teaching critical appraisal to large classes of undergraduate medical students using team-based learning versus group discussions: a randomized controlled trial. BMC Medical Education. 2022;22(1):77. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |