Sun, Feb 22, 2026
[Archive]
Volume 18, Issue 3 (2025)
J Med Edu Dev 2025, 18(3): 155-163 |
Back to browse issues page
Ethics code: IR.ZAUMS.REC.1401.241
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nosratzehi M, Arbabisarjou A, Shahbazi F, Nosratzehi S, Nosratzehi M. Relationship between academic self-efficacy and academic burnout in medical students. J Med Edu Dev 2025; 18 (3) :155-163
URL: http://edujournal.zums.ac.ir/article-1-2445-en.html
URL: http://edujournal.zums.ac.ir/article-1-2445-en.html
Mahin Nosratzehi1  , Azizollah Arbabisarjou2
, Azizollah Arbabisarjou2  , Fatemeh Shahbazi3
, Fatemeh Shahbazi3  , Shahin Nosratzehi *4
, Shahin Nosratzehi *4  , Mohammad Nosratzehi5
, Mohammad Nosratzehi5 
 , Azizollah Arbabisarjou2
, Azizollah Arbabisarjou2  , Fatemeh Shahbazi3
, Fatemeh Shahbazi3  , Shahin Nosratzehi *4
, Shahin Nosratzehi *4  , Mohammad Nosratzehi5
, Mohammad Nosratzehi5 
1- Department of Internal Medicine, Zahedan University of Medical Science, Zahedan, Iran
2- Department of Nursing, Zahedan University of Medical Sciences, Zahedan, Iran
3- Department of Community Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
4- Department of Internal Medicine, Genetics of Non-communicable Disease Research Center, Ali Ibne Abitaleb Hospital, School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran ,shnosratzehi123@gmail.com
5- School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
2- Department of Nursing, Zahedan University of Medical Sciences, Zahedan, Iran
3- Department of Community Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
4- Department of Internal Medicine, Genetics of Non-communicable Disease Research Center, Ali Ibne Abitaleb Hospital, School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran ,
5- School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
Keywords: students, self-efficacy, burnout, professional, residence characteristics, motivation, psychological adaptation
Full-Text [PDF 506 kb]
(886 Downloads)
| Abstract (HTML) (1857 Views)
Full-Text: (44 Views)
Abstract
Background & Objective: Academic self-efficacy is widely known as an important factor in student success, affecting not only academic performance but also emotional strength. In the stressful world of medical education, lower self-efficacy may make students more likely to experience academic burnout. The goal of this study is to look into the relationship between academic self-efficacy and academic burnout in medical students.
Materials & Methods: A correlational study was carried out on 110 clinical medical students during the academic year 2022-2023. Data were gathered using the Academic Self-Efficacy Scale and the Maslach Burnout Inventory for Students. Statistical studies included Pearson's correlation coefficient, independent t-tests, and ANOVA done using SPSS version 22.
Results: The average age of the students was 23.9 ± 1.6 years. Of those taking part, 45.5% were male and 54.5% female. 91.8% were single. 60% were in the clerkship, and 40% in the internship courses. A strong negative relationship was found between academic self-efficacy and academic burnout (r = -0.284, p < 0.01). Female students and those living with their families showed higher academic self-efficacy and lower burnout levels. Also, clerkship students reported higher self-efficacy scores than interns.
Conclusion: Higher academic self-efficacy goes with lower academic burnout, showing a protective effect. Enhancing self-efficacy may improve students' well-being and academic performance. Evidence-based methods such as goal-setting workshops, cognitive-behavior training, self-reflection exercises, and organized mentorship programs have been shown to effectively help academic self-efficacy in medical students, helping to improve academic performance and well-being.
At the same time, it is important to think about the factors that can make self-efficacy lower, especially academic burnout. Academic burnout is an important psychological factor that can make students' motivation, focus, and confidence in their academic abilities lower [9]. Burnout is marked by emotional tiredness, negative feelings (depersonalization), and a feeling of low personal success, and it has become a growing anxiety among medical students [10]. Studies show very high rates of burnout in this group — in some cases up to 88% — often because of heavy academic pressure, high workloads, and limited emotional help [11,12]. Burnout not only affects students' academic results but also harms their mental health, making the risk of anxiety, depression, and even dropping out of university higher [12, 13].
Recent research shows that academic self-efficacy is a key psychological factor that can help medical students deal with academic burnout [14-16]. Based on Bandura's social thinking theory, self-efficacy is about students' beliefs in their ability to do tasks and face challenges, which directly shapes their motivation, emotional control, and academic performance [17]. Studies such as Hayat et al. [18] and Wu et al. [19] show that self-efficacy plays a role in the relationship between academic stress and learning results, where higher self-efficacy leads to lower burnout and higher involvement. Zhang et al. [20] further showed that self-efficacy helps connect burnout and professional behaviors like empathy, pointing out its broader importance in medical education. However, some studies, including Wu et al. [19], report that the direct effect of self-efficacy on academic performance may change depending on factors like gender, school support, or cultural rules. Although there is growing interest worldwide, few studies have looked into these issues in Middle Eastern countries such as Iran, where educational pressures, social support systems, and money challenges may shape students' psychological responses in special ways [18, 21, 22]. This shows a need for local research to understand how academic self-efficacy and burnout are connected in the cultural and school context of Iranian medical schools.
Also, despite the importance of these issues, few studies have looked closely at the relationship between academic self-efficacy and burnout at different stages of medical education. Recent changes in Iran — such as lowering academic motivation, growing money and educational stress, and the psychological effect of the COVID-19 pandemic — may have changed how students experience self-efficacy and academic burnout. So, it is important to do local studies to capture these contextual factors and help create relevant educational and psychological programs.
Based on these points, the current study aims to find out the relationship between academic self-efficacy and academic burnout among medical students.
Materials & Methods
Design and setting(s)
We conducted this correlational study over the 2022–2023 academic year, running from 23 October 2022 to 22 July 2023. The work involved clinical-phase medical students at Zahedan University of Medical Sciences
(ZAUMS), Iran. For some background, within the Iranian medical education system, this clinical phase usually has two main parts: the clerkship (also called Stager or externship), which is a period of watched clinical training in the final undergraduate years, and the internship (Intern). That final internship year comes with full-time clinical duties, still under watch. About who we left out, we did not include students who did not wish to take part or who left key sections of the questionnaire incomplete. We also left out those who reported a past history of major mental health problems—such as depression or anxiety—as these conditions could affect academic self-efficacy or burnout scores. Lastly, to make potential bias less, we left out students who had taken part in similar educational or psychological help during the same semester.
Participants and sampling
Based on earlier studies [23], we know the relation between academic self-efficacy and academic burnout is usually a moderate one, with correlation most often falling between 0.3 and 0.4. To make sure our study was the same as this existing evidence, we went with a correlation measure of 0.3 for our sample size calculation. Using that number, and setting α at 0.05 with a power of 90%, our calculation pointed us toward a target sample size of 110 people taking part.
To get these people taking part, we used a balanced quota sampling way. This meant we randomly picked students from each clinical group to make sure our sample was properly representative.
Tools/Instruments
To start things off, everyone involved was first asked to fill out an informed consent form. This was to make absolutely sure their taking part was voluntary. After that, they completed a basic demographic information form. We gathered simple personal and educational details—stuff like their age, gender, whether they were single or married, if they were in the clerkship or intern stage, and where they were living (like a student dorm, private housing, or with family). We gathered these details to later check if any of these background factors might have an effect on academic self-efficacy or burnout. To measure the students' belief in their own academic abilities, we used the Academic Self-Efficacy Questionnaire, originally developed by Owen and Froman back in 1988 [24]. It is a 33-item tool that checks areas including note-taking, question-asking, class taking part, and computer use. People taking part rated each item on a standard 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The questionnaire shows well-established reliability in international studies, with reported Cronbach's alpha measures generally ranging from 0.86 to 0.93, and test-retest reliability of 0.90 across an 8-week interval [24-26]. For our study, we used the Persian version of the questionnaire, which has 32 items. The reason for one less item is that item 28 is about laboratory courses, which aren't relevant to all programs, so it was taken out. This version has also proven to be reliable; for example, a study by Jamali et al. reported a great Cronbach's alpha of 0.93 for it [27]. In our own study, the reliability was confirmed with a Cronbach's alpha of 0.77. The total score from all 32 items can range from 32 to 160. Based on the scoring used by Jamali et al., we grouped the scores into three groups: low (32–79), moderate (80–119), and high (120–160) academic self-efficacy [27] . To check academic burnout, the Maslach Burnout Inventory for Students, created by Schaufeli et al. in 2002 [28], was given. This 15-item tool needs people taking part to rate statements on a 5-point Likert scale ranging from 1 ("strongly disagree") to 5 ("strongly agree"). It checks three main areas: academic tiredness (5 items), academic not working well (6 items), and academic staying the same (4 items). Total scores were put into groups as low (15–30), moderate (31–50), or high (51–75) burnout. The inventory is widely known internationally and shows strong reliability, with Cronbach's alpha values typically ranging from 0.70 to 0.88 [28-30]. For our Persian-speaking people taking
part, we turned to the version changed and checked by Rostami et al. in 2014, specifically for Iranian students [31]. Their work confirmed the questionnaire's structure and content through exploratory factor study, and they also reported good coming together and different validity. In our sample, we found a Cronbach's alpha of 0.73, which supports the internal consistency of the scale for this study [31].
Data analysis
Statistical study was done using SPSS software (version 22). First data putting together was done through descriptive statistics, including frequencies, percentages, means, and standard deviations. The normalness of data spread was checked using the Kolmogorov-Smirnov test, which showed that the data followed a normal spread. Then, Pearson's correlation coefficient was used to look at the relationship between academic self-efficacy and academic burnout. To compare average scores between two different groups (like clerkship vs. intern), we used independent t-tests. When we needed to compare scores across more than two groups, we turned to Analysis of Variance (ANOVA). For all these tests, we set a meaning level of 0.05.
Results
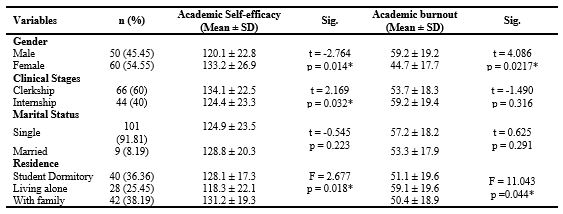
The average age of the students was 23.9 ± 1.6 years. Of those taking part, 45.5% were male and 54.5% female. 91.8% were single. 60% were in the clerkship, and 40% in the internship courses. Figure 1 shows the frequency spread of students based on their academic self-efficacy and academic burnout scores, which were put into low, moderate, and high groups. Table 1 shows the average score of academic self-efficacy and the average score of academic burnout among medical students put into groups by demographic features. Female students showed higher self-efficacy (133.2 ± 26.9) and moderate burnout (44.7 ± 17.7), while students who lived with their family reported better results than those who lived in dorms or alone.
A big difference in academic self-efficacy scores was seen between students in different clinical stages, with clerkship students reporting higher scores than interns (P = 0.032). There was a negative and significant relationship between academic burnout and academic self-efficacy in college students (r = -0.284, p < 0.01). More specifically, academic self-efficacy got lower as academic burnout scores got higher.
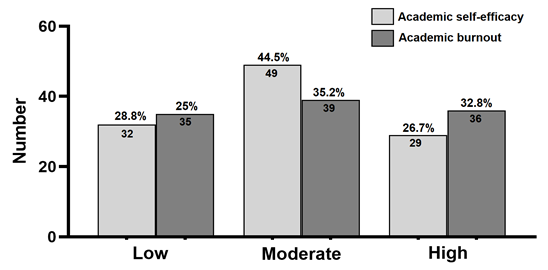
Figure 1. The frequency distribution of students in terms of academic self-efficacy and academic burnout in the low, moderate-, and high-score groups.
Table 1. Academic self-efficacy and academic burnout scores in medical students according to demographic characteristics
Discussion
This study looked at the relation between academic self-efficacy and burnout in medical students. What we found was a clear, negative relationship between the two—meaning students with higher academic self-efficacy tended to report lower levels of academic burnout. This adds to a growing body of research pointing to self-efficacy as a buffer against the psychological and academic pressures common in medical training [4, 23, 32, 33]. In particular, students who felt more confident in their abilities reported less emotional tiredness and academic tiredness [34]. These results are the same as earlier work, such as a 2013 study by Ugwu et al. in Nigeria, which also pointed out self-efficacy as a key factor in strength against burnout [35]. Interestingly, however, they are different from findings by Karami et al. in Iran, where students showed relatively lower burnout levels—possibly because of stronger motivational support systems at the time [36].
Recent research shows that drops in students' self-confidence and internal drive may help explain the rising rates of academic burnout seen in today's medical students [3]. Recent modeling studies suggest that self-efficacy not only affects academic performance, but also plays a key role in how emotional and environmental stressors add to academic tiredness [37]. Also, lower self-efficacy has been linked to lower learning involvement and poor academic adjustment, which can make burnout stronger over time [3]. These insights strengthen that when it comes to helping student well-being in medical training, we can't ignore motivation and mental health factors. Of note, we saw interesting differences in self-efficacy and burnout between genders. In our sample, female students showed higher confidence in their academic abilities and lower burnout levels than male students. This finding is the same as previous research suggesting that female medical students often show greater emotional awareness and benefit from stronger social support systems. These factors appear to help them create more effective ways to cope and greater strength during their studies [38]. Also, Wu et al. found that although female students reported slightly lower internal motivation than males, they tended to do better academically and took part more actively in learning—results that may be partly affected by their stronger self-belief and better management of emotions. These patterns point out that support strategies in medical education should think about how male and female students may have different experiences and use different coping resources [39]. The results show a notable difference in academic self-efficacy between clerkship students and interns. This finding supports earlier work suggesting that confidence in one's academic abilities can change considerably across the stages of medical training, especially as tasks become more demanding and responsibilities get bigger [40, 41]. Clerkship students, who are earlier in their clinical education, typically benefit from closer watching, more guided learning opportunities, and clearer performance expectations—all of which may add to higher confidence in their academic skills [40]. On the other hand, interns work with greater independence and carry more clinical responsibility, which might lead to more pressure and a matching dip in self-efficacy. It is also possible that the more supportive, organized environment during clerkship helps students feel more capable, while the transition to intern-level independence can bring stress that negatively affects how they view their own academic ability [41, 42]. The study also points to the role of environmental factors—especially where students live—in shaping their self-efficacy and burnout levels. Students who lived with their families showed higher self-efficacy and reported only moderate burnout, compared to those living alone or in university housing. This finding makes stronger the idea that family support can help protect against academic stress and emotional tiredness [42]. Similar results were reported by Zhang et al. who noted that external factors—such as money independence, family duties, and social support—play an important role in how vulnerable students are to burnout [43]. These insights remind us that psychological well-being [44] and academic adjustment aren't just about individual features; they're also deeply affected by social, cultural, and living conditions. So, it's important for universities and educators to think about these factors when creating mental health and academic support strategies. Effective ways to help improve academic self-efficacy include organized educational support, personalized mentoring, goal-setting activities, and easy-to-get mental health services [39]. For example, flipped classroom ways have been shown to help more active taking part and give students a greater sense of control over their learning—key ingredients for building self-efficacy [45]. Also, Zhang et al. stressed that self-efficacy doesn't just make burnout less and improve academic habits—it also makes stronger qualities like empathy, which are vital in shaping caring and skilled doctors [20]. Along the same lines, Erschens et al. found that even students with previous work experience struggled to cope with academic burnout when they lacked self-efficacy, pointing out its basic role in adjusting to the demands of medical training [33]. Together, these findings suggest that helping self-efficacy through well-rounded strategies can play a central role in making academic burnout less and helping long-term success—both during medical school and throughout a physician's career. This study has several strengths, including its comparison of medical students at different training stages, the use of balanced sampling, and the use of culturally adjusted and psychometrically sound tools—all of which strengthen its methodological quality and relevance. That said, some limitations should be thought about. First, the cross-sectional nature of the design means we cannot find out cause and effect between academic self-efficacy and burnout. Longer-term studies are needed to understand how these variables affect each other over time. Second, because the sample came from a single university, the results may not apply to other medical schools with different cultural, educational, or school environments. Third, since all measures were based on self-report, responses may have been affected by social desirability or personal interpretation. Also, the study did not account for possible confounding variables—such as academic workload, money pressure, or past academic success—that could affect both self-efficacy and burnout. Future studies would benefit from using multi-center and mixed-way approaches to confirm and build on these results. Comparing students across different fields and training levels—such as preclinical versus clinical phases, or medical versus nursing students—could offer useful insights into how self-efficacy functions in different educational settings. It would also be valuable to look into the factors that shape self-efficacy from the perspective of both students and faculty, which could help find factors that can be changed to support strength and academic success. Further qualitative work is needed to better understand the root causes of academic burnout from students' own experiences, and to look at how mentors, advisors, and peer networks might help make its effects less.
Finally, there is a need for intervention studies that test the effectiveness of approaches such as flipped classrooms, mentoring programs, and emotional intelligence training. These could provide practical, evidence-based strategies for making self-efficacy stronger and making burnout less in medical education.
Conclusion
This study points out the critical importance of academic self-efficacy in making academic burnout less among medical students. Making students' belief in their own capabilities stronger should be a key goal within medical education, as it supports both academic success and psychological well-being. Given the complex relations between personal, social, and environmental influences, efforts to build self-efficacy must take a complete approach. Medical schools are asked to use preventive measures such as regular psychological counseling, early finding of vulnerable students through mental health screenings, and quick referral to specialized support when needed. Offering both emotional and real support—including academic recognition, peer support, and organized mentorship—can further make students' confidence and involvement stronger. In addition, including student input into curriculum design and tailoring educational content to learners' realities can help create a more aware and supportive academic atmosphere. By putting first initiatives centered on self-efficacy, medical educators can not only lower the risk of burnout but also help shape capable, motivated, and emotionally strong future healthcare providers.
Ethical considerations
The present study was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research set up by the Ministry of Health and Medical Education and the Ministry of Science, Research and Technology, Iran. We got the approval by the Ethics Review Committee of Zahedan University of Medical Sciences, Iran (Registration No. IR.ZAUMS.REC.1401.241).
Artificial intelligence utilization for article writing
We confirm that the conception, design, data gathering, statistical study, interpretation of results, and drafting of the manuscript were fully done by the authors. During the preparation of this work, AI tools such as ChatGPT, Instatext and Grammarly were only used to rewrite and improve clarity, style, and grammar. After this AI help, the authors carefully reviewed, revised, and finished all sections of the manuscript, taking full responsibility for the originality, accuracy, and integrity of its contents.
Acknowledgment
The authors would like to thank Zahedan University of Medical Sciences.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author contributions
MN and AAS helped to conceive and design the study. The data gathering was done by FSH and MN. SHN studied and interpreted the data. AAS and MN wrote the first draft of the manuscript and translated it. MN and SHN consulted and supervised the research process. All authors read, revised, and approved the final manuscript.
Funding
The current research was funded by a specific project grant from Zahedan University of Medical Sciences (Grant No: 3468).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
Background & Objective: Academic self-efficacy is widely known as an important factor in student success, affecting not only academic performance but also emotional strength. In the stressful world of medical education, lower self-efficacy may make students more likely to experience academic burnout. The goal of this study is to look into the relationship between academic self-efficacy and academic burnout in medical students.
Materials & Methods: A correlational study was carried out on 110 clinical medical students during the academic year 2022-2023. Data were gathered using the Academic Self-Efficacy Scale and the Maslach Burnout Inventory for Students. Statistical studies included Pearson's correlation coefficient, independent t-tests, and ANOVA done using SPSS version 22.
Results: The average age of the students was 23.9 ± 1.6 years. Of those taking part, 45.5% were male and 54.5% female. 91.8% were single. 60% were in the clerkship, and 40% in the internship courses. A strong negative relationship was found between academic self-efficacy and academic burnout (r = -0.284, p < 0.01). Female students and those living with their families showed higher academic self-efficacy and lower burnout levels. Also, clerkship students reported higher self-efficacy scores than interns.
Conclusion: Higher academic self-efficacy goes with lower academic burnout, showing a protective effect. Enhancing self-efficacy may improve students' well-being and academic performance. Evidence-based methods such as goal-setting workshops, cognitive-behavior training, self-reflection exercises, and organized mentorship programs have been shown to effectively help academic self-efficacy in medical students, helping to improve academic performance and well-being.
Introduction
Academic success is one of the main goals of education systems all over the world and is thought of as an important sign of students' success and progress [1]. In medical education, where academic demands are especially high, it is very important to understand the factors that help students succeed and do well [2]. Among these factors, academic self-efficacy — which is a student's belief in their ability to successfully handle, organize, do, and complete academic tasks — has been known as a basic factor in motivation, getting involved, and learning results [3]. Studies show that students with higher academic self-efficacy tend to have better academic performance, keep working even when facing challenges, and feel more satisfaction with their educational experience [4-6]. Academic self-efficacy also helps explain the correlation between psychological factors, such as anxiety, cognitive skills, and academic satisfaction [7]. These findings point out the complex ways that different factors affect academic success and burnout [8] .At the same time, it is important to think about the factors that can make self-efficacy lower, especially academic burnout. Academic burnout is an important psychological factor that can make students' motivation, focus, and confidence in their academic abilities lower [9]. Burnout is marked by emotional tiredness, negative feelings (depersonalization), and a feeling of low personal success, and it has become a growing anxiety among medical students [10]. Studies show very high rates of burnout in this group — in some cases up to 88% — often because of heavy academic pressure, high workloads, and limited emotional help [11,12]. Burnout not only affects students' academic results but also harms their mental health, making the risk of anxiety, depression, and even dropping out of university higher [12, 13].
Recent research shows that academic self-efficacy is a key psychological factor that can help medical students deal with academic burnout [14-16]. Based on Bandura's social thinking theory, self-efficacy is about students' beliefs in their ability to do tasks and face challenges, which directly shapes their motivation, emotional control, and academic performance [17]. Studies such as Hayat et al. [18] and Wu et al. [19] show that self-efficacy plays a role in the relationship between academic stress and learning results, where higher self-efficacy leads to lower burnout and higher involvement. Zhang et al. [20] further showed that self-efficacy helps connect burnout and professional behaviors like empathy, pointing out its broader importance in medical education. However, some studies, including Wu et al. [19], report that the direct effect of self-efficacy on academic performance may change depending on factors like gender, school support, or cultural rules. Although there is growing interest worldwide, few studies have looked into these issues in Middle Eastern countries such as Iran, where educational pressures, social support systems, and money challenges may shape students' psychological responses in special ways [18, 21, 22]. This shows a need for local research to understand how academic self-efficacy and burnout are connected in the cultural and school context of Iranian medical schools.
Also, despite the importance of these issues, few studies have looked closely at the relationship between academic self-efficacy and burnout at different stages of medical education. Recent changes in Iran — such as lowering academic motivation, growing money and educational stress, and the psychological effect of the COVID-19 pandemic — may have changed how students experience self-efficacy and academic burnout. So, it is important to do local studies to capture these contextual factors and help create relevant educational and psychological programs.
Based on these points, the current study aims to find out the relationship between academic self-efficacy and academic burnout among medical students.
Materials & Methods
Design and setting(s)
We conducted this correlational study over the 2022–2023 academic year, running from 23 October 2022 to 22 July 2023. The work involved clinical-phase medical students at Zahedan University of Medical Sciences
(ZAUMS), Iran. For some background, within the Iranian medical education system, this clinical phase usually has two main parts: the clerkship (also called Stager or externship), which is a period of watched clinical training in the final undergraduate years, and the internship (Intern). That final internship year comes with full-time clinical duties, still under watch. About who we left out, we did not include students who did not wish to take part or who left key sections of the questionnaire incomplete. We also left out those who reported a past history of major mental health problems—such as depression or anxiety—as these conditions could affect academic self-efficacy or burnout scores. Lastly, to make potential bias less, we left out students who had taken part in similar educational or psychological help during the same semester.
Participants and sampling
Based on earlier studies [23], we know the relation between academic self-efficacy and academic burnout is usually a moderate one, with correlation most often falling between 0.3 and 0.4. To make sure our study was the same as this existing evidence, we went with a correlation measure of 0.3 for our sample size calculation. Using that number, and setting α at 0.05 with a power of 90%, our calculation pointed us toward a target sample size of 110 people taking part.
To get these people taking part, we used a balanced quota sampling way. This meant we randomly picked students from each clinical group to make sure our sample was properly representative.
Tools/Instruments
To start things off, everyone involved was first asked to fill out an informed consent form. This was to make absolutely sure their taking part was voluntary. After that, they completed a basic demographic information form. We gathered simple personal and educational details—stuff like their age, gender, whether they were single or married, if they were in the clerkship or intern stage, and where they were living (like a student dorm, private housing, or with family). We gathered these details to later check if any of these background factors might have an effect on academic self-efficacy or burnout. To measure the students' belief in their own academic abilities, we used the Academic Self-Efficacy Questionnaire, originally developed by Owen and Froman back in 1988 [24]. It is a 33-item tool that checks areas including note-taking, question-asking, class taking part, and computer use. People taking part rated each item on a standard 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The questionnaire shows well-established reliability in international studies, with reported Cronbach's alpha measures generally ranging from 0.86 to 0.93, and test-retest reliability of 0.90 across an 8-week interval [24-26]. For our study, we used the Persian version of the questionnaire, which has 32 items. The reason for one less item is that item 28 is about laboratory courses, which aren't relevant to all programs, so it was taken out. This version has also proven to be reliable; for example, a study by Jamali et al. reported a great Cronbach's alpha of 0.93 for it [27]. In our own study, the reliability was confirmed with a Cronbach's alpha of 0.77. The total score from all 32 items can range from 32 to 160. Based on the scoring used by Jamali et al., we grouped the scores into three groups: low (32–79), moderate (80–119), and high (120–160) academic self-efficacy [27] . To check academic burnout, the Maslach Burnout Inventory for Students, created by Schaufeli et al. in 2002 [28], was given. This 15-item tool needs people taking part to rate statements on a 5-point Likert scale ranging from 1 ("strongly disagree") to 5 ("strongly agree"). It checks three main areas: academic tiredness (5 items), academic not working well (6 items), and academic staying the same (4 items). Total scores were put into groups as low (15–30), moderate (31–50), or high (51–75) burnout. The inventory is widely known internationally and shows strong reliability, with Cronbach's alpha values typically ranging from 0.70 to 0.88 [28-30]. For our Persian-speaking people taking
part, we turned to the version changed and checked by Rostami et al. in 2014, specifically for Iranian students [31]. Their work confirmed the questionnaire's structure and content through exploratory factor study, and they also reported good coming together and different validity. In our sample, we found a Cronbach's alpha of 0.73, which supports the internal consistency of the scale for this study [31].
Data analysis
Statistical study was done using SPSS software (version 22). First data putting together was done through descriptive statistics, including frequencies, percentages, means, and standard deviations. The normalness of data spread was checked using the Kolmogorov-Smirnov test, which showed that the data followed a normal spread. Then, Pearson's correlation coefficient was used to look at the relationship between academic self-efficacy and academic burnout. To compare average scores between two different groups (like clerkship vs. intern), we used independent t-tests. When we needed to compare scores across more than two groups, we turned to Analysis of Variance (ANOVA). For all these tests, we set a meaning level of 0.05.
Results
The average age of the students was 23.9 ± 1.6 years. Of those taking part, 45.5% were male and 54.5% female. 91.8% were single. 60% were in the clerkship, and 40% in the internship courses. Figure 1 shows the frequency spread of students based on their academic self-efficacy and academic burnout scores, which were put into low, moderate, and high groups. Table 1 shows the average score of academic self-efficacy and the average score of academic burnout among medical students put into groups by demographic features. Female students showed higher self-efficacy (133.2 ± 26.9) and moderate burnout (44.7 ± 17.7), while students who lived with their family reported better results than those who lived in dorms or alone.
A big difference in academic self-efficacy scores was seen between students in different clinical stages, with clerkship students reporting higher scores than interns (P = 0.032). There was a negative and significant relationship between academic burnout and academic self-efficacy in college students (r = -0.284, p < 0.01). More specifically, academic self-efficacy got lower as academic burnout scores got higher.
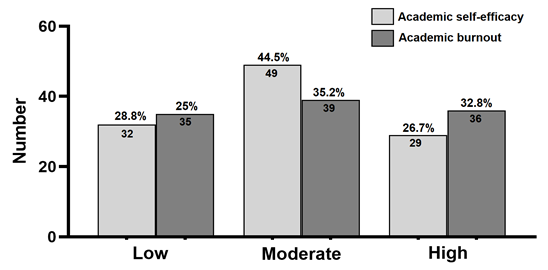
Figure 1. The frequency distribution of students in terms of academic self-efficacy and academic burnout in the low, moderate-, and high-score groups.
Table 1. Academic self-efficacy and academic burnout scores in medical students according to demographic characteristics
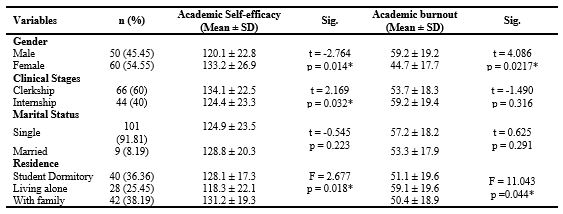
Note: Differences in academic self-efficacy and academic burnout scores were compared across demographic groups. Independent t-tests were used for dichotomous demographic variables, including Gender, Clinical Stages, and Marital Status, while one-way ANOVA was applied for variables with more than two groups, such as Residence. P-values less than 0.05 were considered statistically significant.
Abbreviations: n, number of participants; SD, standard deviation; Sig., statistical significance; p, probability value.
Abbreviations: n, number of participants; SD, standard deviation; Sig., statistical significance; p, probability value.
Discussion
This study looked at the relation between academic self-efficacy and burnout in medical students. What we found was a clear, negative relationship between the two—meaning students with higher academic self-efficacy tended to report lower levels of academic burnout. This adds to a growing body of research pointing to self-efficacy as a buffer against the psychological and academic pressures common in medical training [4, 23, 32, 33]. In particular, students who felt more confident in their abilities reported less emotional tiredness and academic tiredness [34]. These results are the same as earlier work, such as a 2013 study by Ugwu et al. in Nigeria, which also pointed out self-efficacy as a key factor in strength against burnout [35]. Interestingly, however, they are different from findings by Karami et al. in Iran, where students showed relatively lower burnout levels—possibly because of stronger motivational support systems at the time [36].
Recent research shows that drops in students' self-confidence and internal drive may help explain the rising rates of academic burnout seen in today's medical students [3]. Recent modeling studies suggest that self-efficacy not only affects academic performance, but also plays a key role in how emotional and environmental stressors add to academic tiredness [37]. Also, lower self-efficacy has been linked to lower learning involvement and poor academic adjustment, which can make burnout stronger over time [3]. These insights strengthen that when it comes to helping student well-being in medical training, we can't ignore motivation and mental health factors. Of note, we saw interesting differences in self-efficacy and burnout between genders. In our sample, female students showed higher confidence in their academic abilities and lower burnout levels than male students. This finding is the same as previous research suggesting that female medical students often show greater emotional awareness and benefit from stronger social support systems. These factors appear to help them create more effective ways to cope and greater strength during their studies [38]. Also, Wu et al. found that although female students reported slightly lower internal motivation than males, they tended to do better academically and took part more actively in learning—results that may be partly affected by their stronger self-belief and better management of emotions. These patterns point out that support strategies in medical education should think about how male and female students may have different experiences and use different coping resources [39]. The results show a notable difference in academic self-efficacy between clerkship students and interns. This finding supports earlier work suggesting that confidence in one's academic abilities can change considerably across the stages of medical training, especially as tasks become more demanding and responsibilities get bigger [40, 41]. Clerkship students, who are earlier in their clinical education, typically benefit from closer watching, more guided learning opportunities, and clearer performance expectations—all of which may add to higher confidence in their academic skills [40]. On the other hand, interns work with greater independence and carry more clinical responsibility, which might lead to more pressure and a matching dip in self-efficacy. It is also possible that the more supportive, organized environment during clerkship helps students feel more capable, while the transition to intern-level independence can bring stress that negatively affects how they view their own academic ability [41, 42]. The study also points to the role of environmental factors—especially where students live—in shaping their self-efficacy and burnout levels. Students who lived with their families showed higher self-efficacy and reported only moderate burnout, compared to those living alone or in university housing. This finding makes stronger the idea that family support can help protect against academic stress and emotional tiredness [42]. Similar results were reported by Zhang et al. who noted that external factors—such as money independence, family duties, and social support—play an important role in how vulnerable students are to burnout [43]. These insights remind us that psychological well-being [44] and academic adjustment aren't just about individual features; they're also deeply affected by social, cultural, and living conditions. So, it's important for universities and educators to think about these factors when creating mental health and academic support strategies. Effective ways to help improve academic self-efficacy include organized educational support, personalized mentoring, goal-setting activities, and easy-to-get mental health services [39]. For example, flipped classroom ways have been shown to help more active taking part and give students a greater sense of control over their learning—key ingredients for building self-efficacy [45]. Also, Zhang et al. stressed that self-efficacy doesn't just make burnout less and improve academic habits—it also makes stronger qualities like empathy, which are vital in shaping caring and skilled doctors [20]. Along the same lines, Erschens et al. found that even students with previous work experience struggled to cope with academic burnout when they lacked self-efficacy, pointing out its basic role in adjusting to the demands of medical training [33]. Together, these findings suggest that helping self-efficacy through well-rounded strategies can play a central role in making academic burnout less and helping long-term success—both during medical school and throughout a physician's career. This study has several strengths, including its comparison of medical students at different training stages, the use of balanced sampling, and the use of culturally adjusted and psychometrically sound tools—all of which strengthen its methodological quality and relevance. That said, some limitations should be thought about. First, the cross-sectional nature of the design means we cannot find out cause and effect between academic self-efficacy and burnout. Longer-term studies are needed to understand how these variables affect each other over time. Second, because the sample came from a single university, the results may not apply to other medical schools with different cultural, educational, or school environments. Third, since all measures were based on self-report, responses may have been affected by social desirability or personal interpretation. Also, the study did not account for possible confounding variables—such as academic workload, money pressure, or past academic success—that could affect both self-efficacy and burnout. Future studies would benefit from using multi-center and mixed-way approaches to confirm and build on these results. Comparing students across different fields and training levels—such as preclinical versus clinical phases, or medical versus nursing students—could offer useful insights into how self-efficacy functions in different educational settings. It would also be valuable to look into the factors that shape self-efficacy from the perspective of both students and faculty, which could help find factors that can be changed to support strength and academic success. Further qualitative work is needed to better understand the root causes of academic burnout from students' own experiences, and to look at how mentors, advisors, and peer networks might help make its effects less.
Finally, there is a need for intervention studies that test the effectiveness of approaches such as flipped classrooms, mentoring programs, and emotional intelligence training. These could provide practical, evidence-based strategies for making self-efficacy stronger and making burnout less in medical education.
Conclusion
This study points out the critical importance of academic self-efficacy in making academic burnout less among medical students. Making students' belief in their own capabilities stronger should be a key goal within medical education, as it supports both academic success and psychological well-being. Given the complex relations between personal, social, and environmental influences, efforts to build self-efficacy must take a complete approach. Medical schools are asked to use preventive measures such as regular psychological counseling, early finding of vulnerable students through mental health screenings, and quick referral to specialized support when needed. Offering both emotional and real support—including academic recognition, peer support, and organized mentorship—can further make students' confidence and involvement stronger. In addition, including student input into curriculum design and tailoring educational content to learners' realities can help create a more aware and supportive academic atmosphere. By putting first initiatives centered on self-efficacy, medical educators can not only lower the risk of burnout but also help shape capable, motivated, and emotionally strong future healthcare providers.
Ethical considerations
The present study was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research set up by the Ministry of Health and Medical Education and the Ministry of Science, Research and Technology, Iran. We got the approval by the Ethics Review Committee of Zahedan University of Medical Sciences, Iran (Registration No. IR.ZAUMS.REC.1401.241).
Artificial intelligence utilization for article writing
We confirm that the conception, design, data gathering, statistical study, interpretation of results, and drafting of the manuscript were fully done by the authors. During the preparation of this work, AI tools such as ChatGPT, Instatext and Grammarly were only used to rewrite and improve clarity, style, and grammar. After this AI help, the authors carefully reviewed, revised, and finished all sections of the manuscript, taking full responsibility for the originality, accuracy, and integrity of its contents.
Acknowledgment
The authors would like to thank Zahedan University of Medical Sciences.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author contributions
MN and AAS helped to conceive and design the study. The data gathering was done by FSH and MN. SHN studied and interpreted the data. AAS and MN wrote the first draft of the manuscript and translated it. MN and SHN consulted and supervised the research process. All authors read, revised, and approved the final manuscript.
Funding
The current research was funded by a specific project grant from Zahedan University of Medical Sciences (Grant No: 3468).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
Article Type : Brief Report |
Subject:
Medical Education
Received: 2025/03/12 | Accepted: 2025/09/28 | Published: 2025/10/1
Received: 2025/03/12 | Accepted: 2025/09/28 | Published: 2025/10/1
References
1. Sahlberg P. Trends in global education reform since the 1990s: looking for the right way. Int J Educ Dev. 2023;98:102748. [DOI:10.1016/j.ijedudev.2023.102748]
2. Lisnyj KT, Pearl DL, McWhirter JE, Papadopoulos A. Exploration of factors affecting post-secondary students' stress and academic success: application of the socio-ecological model for health promotion. Int J Environ Res Public Health. 2021;18(7):3779. [DOI:10.3390/ijerph18073779] [PMID] []
3. Wu H, Li S, Zheng J, Guo J. Medical students' motivation and academic performance: the mediating roles of self-efficacy and learning engagement. Med Educ Online. 2020;25(1):1742964. [DOI:10.1080/10872981.2020.1742964] [PMID] []
4. Meng Q, Zhang Q. The influence of academic self-efficacy on university students' academic performance: the mediating effect of academic engagement. Sustainability. 2023;15(7):5767. [DOI:10.3390/su15075767]
5. Bohee S. Effects of satisfaction with major and academic self-efficacy on academic persistence of students in health-related fields. Korean J Emerg Med Serv. 2022;26(3):93-104.
6. Al-Abyadh MA, Abdel Azeem HH. Academic achievement: influences of university students' self-management and perceived self-efficacy. J Intell. 2022;10(3):55. [DOI:10.3390/jintelligence10030055] [PMID] []
7. Huamán-Tapia E, Almanza-Cabe RB, Sairitupa-Sanchez LZ, Pinto Tapia B, Barja-Ore J, Flores-Mendoza A, et al. Critical thinking, generalized anxiety in satisfaction with studies: the mediating role of academic self-efficacy in medical students. Behav Sci. 2023;13(8):665. [DOI:10.3390/bs13080665] [PMID] []
8. Tong Q. Exploring the interplay between teachers' emotions, personal traits, environmental factors and psychological well-being. Eur J Educ. 2025;60(1):e12903. [DOI:10.1111/ejed.12903]
9. Özhan MB. Academic self-efficacy and school burnout in university students: assessment of the mediating role of grit. Curr Psychol. 2021;40(9):4235-4246. [DOI:10.1007/s12144-021-02023-9]
10. Cotobal Rodeles S, Martín Sánchez FJ, Martínez-Sellés M. Physician and medical student burnout, a narrative literature review: challenges, strategies, and a call to action. J Clin Med. 2025;14(7):2263. [DOI:10.3390/jcm14072263] [PMID] []
11. Di Vincenzo M, Arsenio E, Della Rocca B, Lax A, Sampogna G, Volpicelli A, et al. Is there a burnout epidemic among medical students? Results from a systematic review. Medicina. 2024;60(4):575. [DOI:10.3390/medicina60040575] [PMID] []
12. Nazari S, Ghazvini H, Seyedhosseini Tamijani SM, Rafaiee R. Increased suicide of Iranian resident physicians in the COVID-19 pandemic. Int J High Risk Behav Addict. 2022;11(1):e117651. [DOI:10.5812/ijhrba.117651]
13. Ashraf D. The hidden epidemic: burnout and mental health amongst medical students. Surgo. 2024;1(3):297. [DOI:10.36399/Surgo.1.297]
14. Liu W, Zhang R, Wang H, Zhang L, Li Z, Liu H, et al. Association between anxiety, depression symptoms, and academic burnout among Chinese students: the mediating role of resilience and self-efficacy. BMC Psychol. 024;12(1):335. [DOI:10.1186/s40359-024-01823-5] [PMID] []
15. Kong LN, Yang L, Pan YN, Chen SZ. Proactive personality, professional self-efficacy and academic burnout in undergraduate nursing students in China. J Prof Nurs.2021;37(4):690-695. [DOI:10.1016/j.profnurs.2021.04.003] [PMID]
16. Chen C, Shen Y, Zhu Y, Xiao F, Zhang J, Ni J. The effect of academic adaptability on learning burnout among college students: the mediating effect of self-esteem and the moderating effect of self-efficacy. Psychol Res Behav Manag. 2023;16:1615-1629. [DOI:10.2147/PRBM.S408591] [PMID] []
17. Woreta GT, Zewude GT, Józsa K. The mediating role of self-efficacy and outcome expectations in the relationship between peer context and academic engagement: a social cognitive theory perspective. Behav Sci. 2025;15(5):681. [DOI:10.3390/bs15050681] [PMID] []
18. Hayat AA, Shateri K, Amini M, Shokrpour N. Relationships between academic self-efficacy, learning-related emotions, and metacognitive learning strategies with academic performance in medical students: a structural equation model. BMC Med Educ. 2020;20(1):76. [DOI:10.1186/s12909-020-01995-9] [PMID] []
19. Wu Y, Xie F, Jiang R. Academic anxiety, self-regulated learning ability, and self-esteem in Chinese candidates for college entrance examination during the COVID-19 outbreak: a survey study. Psychol Res Behav Manag. 2022;15:2383-2390. [DOI:10.2147/PRBM.S360127] [PMID] []
20. Zhang X, Han G, Feng C, Xu Y, Gao L, Tan Z. The relationship between self-efficacy, learning burnout, willingness to fulfill the contract and empathy of rural-oriented tuition-waived medical students of China: a cross-sectional study. BMC Med Educ. 2025;25(1):53. [DOI:10.1186/s12909-025-06637-6] [PMID] []
21. Mohsen AS. The impact of self-esteem, academic self-efficacy and perceived stress on academic performance: a cross-sectional study of Saudi psychology students. Eur J Educ Sci. 2017;4(3):51-63.
22. Turan S, Demirel Ö, Sayek İ. Metacognitive awareness and self-regulated learning skills of medical students in different medical curricula. Med Teach. 2009;31(10):e477-e483. [DOI:10.3109/01421590903193521] [PMID]
23. Fooladvand K. Role of social support, academic stress and academic self-efficacy on mental and physical health. Contemp Psychol. 2010;4(2):81-94.
24. Owen SV, Froman RD. Development of a college academic self-efficacy scale. Paper presented at: Annual Meeting of the National Council on Measurement in Education; 1988 Apr 5-7; New Orleans, LA.
25. Kula S, Taşdemir M. Evaluation of pre-service teachers' academic self-efficacy levels in terms of some certain variables. Procedia Soc Behav Sci. 2014;141:686-690. [DOI:10.1016/j.sbspro.2014.05.120]
26. Ifdil I, Bariyyah K, Dewi A, Rangka I. The college academic self-efficacy scale (CASES); An Indonesian validation to measure the self-efficacy of students. J Kajian Bimbingan Konseling. 2019;4(4):115-121. [DOI:10.17977/um001v4i42019p115]
27. Jamali M, Noroozi A, Tahmasebi R. Factors affecting academic self-efficacy and its association with academic achievement among students of Bushehr University of Medical Sciences 2012-13. Iran J Med Educ. 2013;13(8):629-641.
28. Schaufeli WB, Martínez IM, Pinto AM, Salanova M, Bakker AB. Burnout and engagement in university students: a cross-national study. J Cross Cult Psychol. 2002;33(5):464-481. [DOI:10.1177/0022022102033005003]
29. Hu Q, Schaufeli WB. The factorial validity of the Maslach burnout inventory-student survey in China. Psychol Rep. 2009;105(2):394-408. [DOI:10.2466/PR0.105.2.394-408] [PMID]
30. Campos JADB, Maroco J. Maslach burnout inventory-student survey: portugal-Brazil cross-cultural adaptation. Rev Saude Publica. 2012;46(5):816-824. [DOI:10.1590/S0034-89102012000500008] [PMID]
31. Rostami Z, Abedi M, Schaufeli W, Ahmadi S. The psychometric characteristics of Maslach burnout inventory student survey: a study students of Isfahan University. Zahedan J Res Med Sci. 2013;16(9):55-58.
32. Amnie A. An investigation of predictors of self-efficacy to cope with stress and implications for health education practice. Am J Health Educ. 2018;49(3):1-11. [DOI:10.1080/19325037.2018.1431165]
33. Erschens R, Schröpel C, Herrmann-Werner A, Loda T, Jerg-Bretzke L, Keifenheim KE, et al. The mediating role of self-efficacy in the relationship between past professional training and burnout resilience in medical education: a multicentre cross-sectional study. BMC Med Educ. 2024;24(1):875. [DOI:10.1186/s12909-024-05854-9] [PMID] []
34. Wang Q, Sun W, Wu H. Associations between academic burnout, resilience and life satisfaction among medical students: a three-wave longitudinal study. BMC Med Educ. 2022;22(1):248. [DOI:10.1186/s12909-022-03326-6] [PMID] []
35. Ugwu FO, Onyishi IE, Tyoyima WA. Exploring the relationships between academic burnout, self-efficacy and academic engagement among Nigerian college students. Afr Symp. 2013;13(2):37-45.
36. Karami J, Hatamian P. The relationship between self-efficacy and perfectionism with academic burnout students. Pajoohande. 2016;21(4):186-191.
37. Cong Y, Yang L, Ergün ALP. Exploring the relationship between burnout, learning engagement and academic self-efficacy among EFL learners: a structural equation modeling analysis. Acta Psychol. 2024;248:104394. [DOI:10.1016/j.actpsy.2024.104394] [PMID]
38. Theis S, Bryan E, Ringler C. Addressing gender and social dynamics to strengthen resilience for all. In: 2019 Annual trends and outlook report: gender equality in rural Africa: From commitments to outcomes. Washington (DC): International Food Policy Research Institute; 2019. p. 126-139. [DOI:10.2499/9780896293649_09]
39. Valverde-Janer M, Ortega-Caballero M, Ortega-Caballero I, Ortega-Caballero A, Segura-Robles A. Study of factors associated with the development of emotional intelligence and resilience in university students. Educ Sci. 2023;13(3):255. [DOI:10.3390/educsci13030255]
40. Cevik AA, Cakal ED, Alao D, Elzubeir M, Shaban S, Abu-Zidan F. Self-efficacy beliefs and expectations during an emergency medicine clerkship. Int J Emerg Med. 2022;15(1):4. [DOI:10.1186/s12245-021-00406-0] [PMID] []
41. Durduran Y, Hacılar E, Yücel M. Evaluation of professional self-efficacy perceptions of medical school intern students. J Basic Clin Health Sci. 2024;8(1):110-118. [DOI:10.30621/jbachs.1297758]
42. Wilks SE. Resilience amid academic stress: the moderating impact of social support among social work students. Adv Soc Work. 2008;9(2):106-125. [DOI:10.18060/51]
43. Zhang JY, Shu T, Xiang M, Feng ZC. Learning burnout: evaluating the role of social support in medical students. Front Psychol. 2021;12:625506. [DOI:10.3389/fpsyg.2021.625506] [PMID] []
44. Niroumand Sarvandani M, Garmabi B, Asadi M, Ghazvini H, Rafaiee R, Kalalian Moghaddam H. Impact of circadian rhythm disturbance and chronotype on medical students' mental state. Basic Clin Neurosci. 2025;16(2):219-232. [DOI:10.32598/bcn.2022.1425.6] [PMID] []
45. Langer AL, Parnes AD, Kumar NL, Kesselheim JC, Osman NY. The "flipped visit": an innovative method to improve medical student self-efficacy through a structured approach in clinic. BMC Med Educ. 2024;24(1):1118. [DOI:10.1186/s12909-024-06122-6] [PMID] []
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |