Tue, Feb 24, 2026
[Archive]
Volume 18, Issue 1 (2025)
J Med Edu Dev 2025, 18(1): 23-31 |
Back to browse issues page
Ethics code: 980543
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Daryazadeh S, Amouzeshi Z. Impact of interprofessional education on the attitudes and clinical skills of medical and nursing students: A quasi-experimental study. J Med Edu Dev 2025; 18 (1) :23-31
URL: http://edujournal.zums.ac.ir/article-1-2296-en.html
URL: http://edujournal.zums.ac.ir/article-1-2296-en.html
1- Department of Medical Education, Medical Education Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
2- Department of Nursing, School of Nursing and Midwifery, Birjand University of Medical Sciences, Birjand, Iran ,amouzeshiz9039@gmail.com
2- Department of Nursing, School of Nursing and Midwifery, Birjand University of Medical Sciences, Birjand, Iran ,
Full-Text [PDF 868 kb]
(893 Downloads)
| Abstract (HTML) (1754 Views)
Full-Text: (345 Views)
Abstract
Background & Objective: Interprofessional education is widely recognized as a fundamental approach for fostering collaborative teamwork and enhancing healthcare delivery. This study examined the impact of an interprofessional education program on the attitudes and clinical skills of medical and nursing students in surgery wards.
Materials & Methods: This quasi-experimental study used a single group, pre- and post-test design. Ten 3-hour Interprofessional education sessions were held in the surgery ward for 10 small groups of medical and nursing students (n = 42). Pretests and posttests were administered using a checklist to evaluate the students' clinical skills in dressing replacement. Furthermore, the attitudes of both groups of students toward interprofessional education were assessed with a valid and reliable questionnaire following the educational intervention. Data were analyzed in SPSS software using chi-square, t-test, and Mann-Whitney U tests.
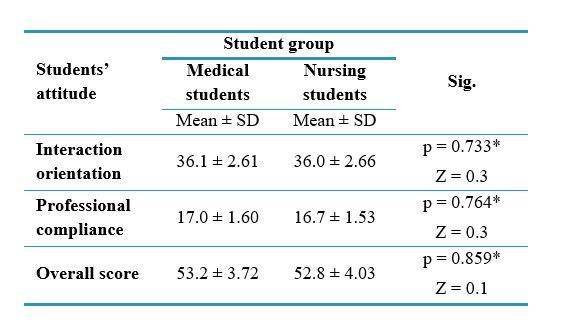
Results: A significant difference was observed in the mean scores for dressing replacement skills between medical and nursing students before and after the intervention (p < 0.001). The Mann-Whitney U test indicated that there was no significant difference in the mean scores for attitudes in the two domains of interaction-orientedness (p = 0.733) and professional compliance (p = 0.764).
Conclusion: The findings of this study suggest that interprofessional education can effectively enhance the clinical skills of both medical and nursing students, thereby promoting better patient care. It is crucial to foster a positive attitude among learners and educators through training programs to maximize the effectiveness of interprofessional education.
Introduction
Every member of the healthcare team brings their unique expertise to patient care. Collaboration and communication within the team are essential for providing effective care [1]. That said, the World Health Organization has identified Interprofessional Education (IPE) as an effective approach for promoting collaborative teamwork and improving healthcare delivery [2, 3]. IPE refers to a collaborative learning process where students from diverse healthcare disciplines engage in shared educational experiences. Such learning is enacted collaboratively within the context of patient care [4] and should be a crucial element of education in disciplines such as medicine and nursing [1]. An IPE intervention occurs when professionals from various health or social care fields participate in interactive learning activities together. The main goal is to enhance interprofessional collaboration and improve the health and well-being of patients or clients. This type of learning involves active participation and exchanges among learners from various professions [5].
IPE encourages students to cultivate a positive attitude toward collaborating with various healthcare professionals. It helps them understand and respect the unique roles and responsibilities of their colleagues, leading to better service delivery and fewer medical errors [5]. IPE serves as a fundamental element in building a strong and flexible healthcare workforce. It creates a positive environment and boosts motivation for collaboration among health professionals, thereby playing a crucial role in developing human resources that can provide efficient and responsive care [6]. Moreover, medical educators are increasingly recognizing the significance of integrating IPE into their curricula [2]. This emphasis arises from the understanding that solitary professional identity formation, devoid of IPE exposure, can hinder effective collaboration within the complex dynamics of the patient care team and pose challenges for future professional trajectories [1].
Ineffective collaboration between physicians and nurses can result in lower-quality patient care, reduced job satisfaction, and increased treatment costs. Therefore, IPE is a vital part of healthcare education, especially for nursing and medical students [7]. Hence, effective IPE implementation is expected to reduce medical errors, boost patient satisfaction, and ultimately culminate in improved patient care outcomes [3].
Integrating IPE into medical science curricula is essential for ensuring patient safety [8]. Research highlights IPE's effectiveness in promoting interprofessional thinking, patient-centered care, shared knowledge, and improved mutual understanding [1]. Research on the effectiveness of IPE shows that it positively affects teamwork and communication skills among participants [1, 9, 10]. Studies on IPE in clinical settings underscore its critical role in improving communication, teamwork, and, ultimately, patient care and safety [4, 11]. A Best Evidence Medical Education (BEME) guide supports these findings, highlighting IPE's impact on learner attitudes and learning [8]. Although there is ample evidence supporting IPE, it remains underrecognized and is not effectively utilized in educational institutions within the country [12]. IPE can improve attitudes toward teamwork and collaboration, potentially leading to better patient care post-graduation. However, the optimal timing for introducing medical students to IPE remains a matter of debate [13]. This investigation was motivated by a perceived lack of IPE in our university's surgery ward. Given the documented benefits of IPE and the paucity of research examining its efficacy in clinical settings, this investigation aimed to assess the impact of IPE on the clinical skills and attitudes of medical and nursing students.
Materials & Methods
Design and setting(s)
This quasi-experimental study used a single group, pre- and post-test design at Birjand University of Medical Sciences in Iran from 21 April 2022 to 22 July 2022. It is important to note that random selection of students was not possible, as they had already been assigned to apprenticeship groups by the faculty.
Participants and sampling
The study population comprised all medical and nursing students in the clinical phase of their respective programs who were willing to participate. It is important to note that students who were absent for more than one day were excluded from the study. Additionally, eight nursing students opted not to participate. A total of 42 students were recruited using the census method (Figure 1).
Tools/Instruments
The demographic information form collected data on participants' age, gender, field of study, and GPA.
A dressing replacement skill checklist was created based on a standard nursing textbook to evaluate student skills before and after the IPE intervention. This checklist consisted of 16 dichotomous items (yes/no, 1/0), corresponding to the procedural steps of dressing replacement. Each item was scored as either correct or left blank. The total score for each student ranged from 0 to 20 to facilitate easier interpretation and analysis.
Content validity was established through expert review by ten clinical nursing and medical faculty members from the surgery ward. To confirm the face validity of the checklist, it was administered to 20 nursing students. Test-retest reliability for the dressing replacement skill checklist was assessed using Pearson’s correlation coefficient over a two-week interval (r = 0.55, p = 0.011, n = 20), indicating a moderate level of temporal stability for the tool.
Medical and nursing students completed a questionnaire to assess their attitudes toward IPE following the educational intervention. We utilized the Attitudes to IPE Questionnaire, which had been previously translated into Persian in Sohrabi et al.'s study, where its validity and reliability were confirmed [14]. We referenced this study in our article. In the Sohrabi et al. study, the original 15-item instrument was translated into Persian and underwent a psychometric evaluation to confirm its content, structure, and construct validity, as well as its internal consistency and test-retest reliability. Ten participants and 10 experts assessed content validity and content validity index; construct validity was evaluated using exploratory factor analysis. According to the impact item score above 1.5, the index of content validity of 0.62, and the content validity index of 0.7, 12 questions were preserved. Based on exploratory factor analysis, 12 items were kept in scale. The final questionnaire consisted of 12 items that participants responded to using a 5-point Likert scale, ranging from "completely agree" to "completely disagree." The questionnaire items focused on two primary constructs: interaction-orientedness (8 items) and professional compliance (4 items). The reliability of the attitude scale was established by computing the stability coefficient (Spearman’s ρ = 0.92) and internal consistency (Cronbach’s ά = 0.866) [14].
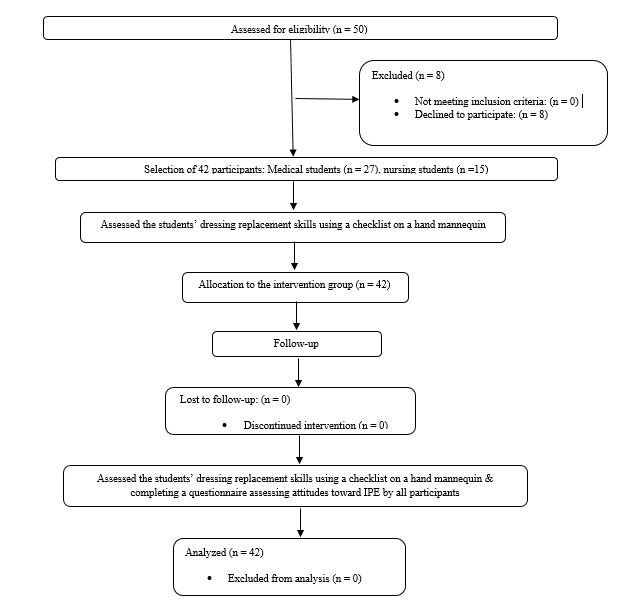
Figure 1. Flow chart of the study
Data collection methods
The educational intervention was delivered through an IPE program integrated into the formal coursework.
Clinical faculty members from both medicine and nursing, who are responsible for the undergraduate curricula in the surgical ward, were brought together to discuss the rationale for implementing IPE. A comprehensive analysis of common essential competencies/skills within the surgical context was conducted, drawing upon both medical and nursing curricula. Participants were asked to identify a fundamental skill that is essential for all students. Due to a preference for skills that are readily attainable, the dressing replacement skill was chosen as the selected competency.
Prior to the intervention, a briefing session was conducted to familiarize students with the concept of IPE. Before the start of the IPE training sessions, a pretest was administered to evaluate students’ dressing replacement skills using a manikin. The assessor was a senior nursing graduate who had experience working in the surgical department. Ten small groups were formed, each comprising four to five nursing (consisting of eighth semester nursing students) and medical students (consisting of fourth and sixth year medical students) in clinical phases who were willing to participate in the study. A master's degree in nursing with surgical ward experience and a surgical chief resident served as mentors for these learning cohorts. Before the intervention, to ensure proper skill transfer by students in both groups, medical students underwent targeted training in history-taking under the mentorship of the surgical chief resident. Nursing students training in dressing replacement began with an instructional video, followed by guided practice under the supervision of a mentor. Each group of medical and nursing students was then assigned two patients, for whom they were responsible during their clinical training, with oversight from a supervisor.
Efforts were made to ensure that nursing students were present while medical students took the patients' histories. Similarly, medical students were present when nursing students changed the dressings. The program spanned two weeks, encompassing ten three-hour sessions conducted in the surgery ward between 8:00 AM and 11:00 AM. This timeframe allowed for concurrent skill training and patient care. After the intervention, the students’ dressing replacement skills were reevaluated using the same checklist on the
manikin. One by one, students entered the testing room and were asked to dress a wound on a hand mannequin. The observer, who was a senior nurse with clinical experience, assessed their skills using a checklist. Additionally, students completed the attitude questionnaire upon program conclusion.
Data analysis
Because the data did not follow a normal distribution, non-parametric tests were used for data analysis. The Wilcoxon test was employed to compare the mean scores of dressing replacement skills before and after the intervention, while the Mann-Whitney test was used to compare the interprofessional attitude mean scores between medical and nursing students. Data analysis was conducted using SPSS version 23.
Results
The study sample consisted of 42 students (54.8% female, n = 23; 45.2% male, n = 19), with a mean age of 23.9 ± 3.03 years (Table 1). The results of the statistical tests indicated no significant differences between medical and nursing students regarding the variables analyzed (age, gender, and GPA), demonstrating that the groups were homogeneous (p > 0.05).
Table 1. Demographic characteristics of the students (n = 42)
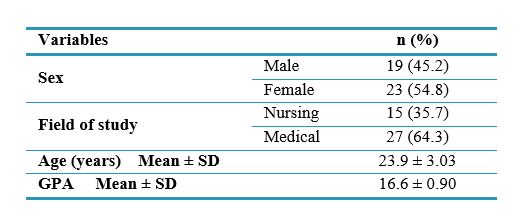
Abbreviations: n, number of participants; SD, standard deviation; GPA, grade point average.
A significant difference was observed in the mean scores for dressing replacement skills (out of 20) before and after the intervention (p < 0.001) (Table 2, Figure 2).
Table 2. Comparison of mean scores for dressing replacement skill before and after the intervention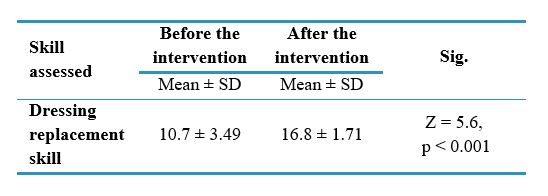
Notes: Wilcoxon was used to compare mean scores of the dressing replacement skill before and after the intervention
Abbreviations: SD, standard deviation; Sig., statistical significance.
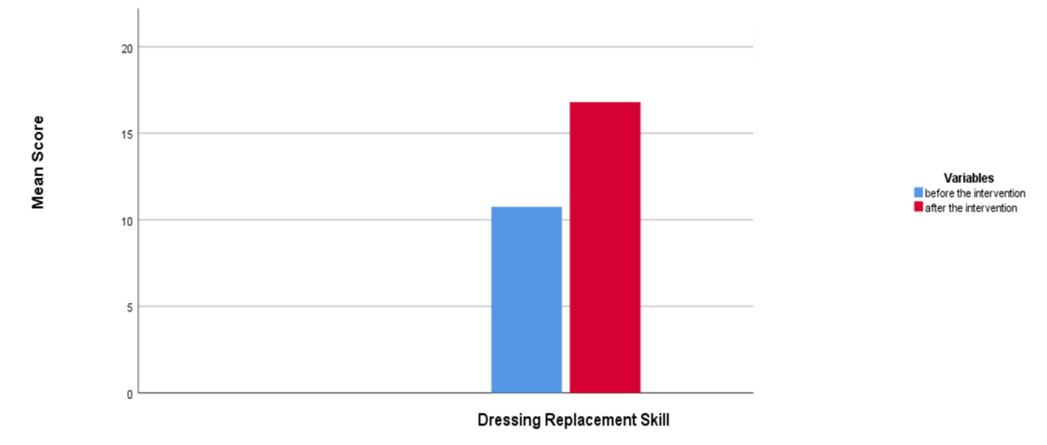
Table 3. Comparison of interprofessional attitude mean scores between medical and nursing students
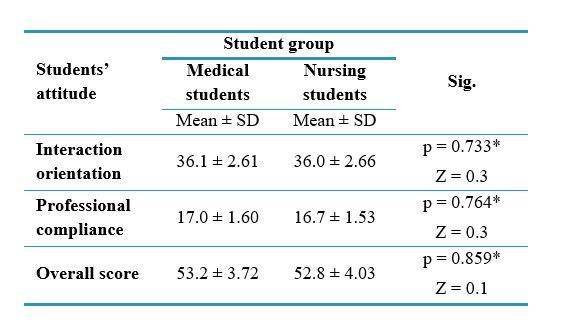
Notes: * Mann-Whitney was used to compare the interprofessional attitude mean scores in medical and nursing students
Abbreviations: SD, standard deviation; p, probability-value
Discussion
This study sought to determine the impact of an IPE program on the clinical skills and attitudes of medical and nursing students. The results showed that the mean dressing replacement skill score in both groups of students increased significantly after the IPE intervention. These findings support the effectiveness of the IPE program in enhancing dressing replacement skills. The results demonstrated a significant difference in mean scores between the two groups of students both before and after the intervention. Notably, nursing students demonstrated higher baseline mean scores, potentially attributable to prior exposure to related competencies and increased practical experience. While nursing students maintained a performance advantage after the intervention, the disparity between groups was lessened, highlighting the IPE program’s particular benefit for medical students in acquiring this clinical skill. The pronounced initial skill discrepancy between the two disciplines underscores the imperative for interprofessional learning to optimize clinical skills and teamwork. Analysis of student attitudes toward the IPE program revealed high mean scores, reflecting a positive disposition toward IPE. A comparative analysis of mean attitude scores between nursing and medical students yielded no significant differences, suggesting a shared positive attitude towards IPE and alignment across both domains of the questionnaire (interaction-orientedness and professional compliance).
Research has explored IPE within clinical settings [4, 11]. Braun et al.'s study titled "Impact of Interprofessional Education for Medical and Nursing Students on the Nutritional Management of In-Patients" employed IPE across different student groups. The study aimed to develop skills in patient-centered care, professional role development, communication, teamwork, ethical decision-making, and patient advocacy. The results demonstrate that learners' clinical performance is enhanced as their roles and understanding of their professions evolve [11].
IPE has proven to be an effective teaching approach in clinical environments. Research by Dyess et al., Renschler et al., Cino et al., and Mahdizadeh et al. demonstrate that IPE greatly improves students' knowledge and clinical skills. Additionally, by promoting collaborative learning and teamwork, IPE has the potential to substantially enhance patient safety outcomes [3, 4, 15, 16]. These findings are consistent with our study on the effectiveness of IPE in a clinical setting. The results of Renschler et al.'s study, titled “Effect of Interprofessional Clinical Education Programme Length on Students’ Attitudes Towards Teamwork,” indicated that IPE in clinical settings improves students’ understanding of professional roles and responsibilities, ultimately leading to better patient care [4]. A study by Mahdizadeh et al. titled "Clinical Interdisciplinary Collaboration Models and Frameworks: From Similarities to Differences," conducted as a systematic review, highlights the importance of interprofessional collaboration between physicians and nurses in clinical settings. The study's findings reveal that successful implementation of these partnerships can lead to fewer adverse events and better patient outcomes. This collaborative model shows great potential for enhancing the efficiency and safety of patient care across various healthcare stakeholders [15]. However, the results of a systematic review conducted by Dyess et al. titled "Impact of Interprofessional Education on Students of the Health Professions" highlights that establishing and maintaining interprofessional collaboration within a multidisciplinary surgery team with diverse characteristics is complex. This complexity can influence practices and patient care [3]. Barrios and Torres, in a study titled "Interprofessional Health Education Teacher Training at the University of Chile," emphasized that the main goal of IPE is to prepare learners to improve their professional roles within healthcare teams. Therefore, teachers need to be equipped to function as effective and supportive interprofessional teams as well. They recommend that teachers employ practical strategies to enhance the effectiveness and success of IPE [17]. A study by Irajpour et al. titled "Situation Analysis and Designing an Interprofessional Curriculum for Palliative Care of Cancer Patients" conducted in Iran, revealed that IPE can be a fundamental framework for promoting collaborative care among healthcare providers addressing the complex needs of palliative care patients [18]. The findings of this study align with our research, which demonstrates the potential of IPE to enhance patient care. However, one possible explanation for the lack of significant differences in attitudes between the two groups of medical and nursing students is the limited duration of exposure to the IPE program.
Mattiazzi et al. conducted a systematic literature review titled "Behavioral Outcomes of Interprofessional Education within Clinical Settings for Health Professional Students," which found that IPE in clinical settings can help students develop competencies in interprofessional collaborative practice. However, the review also notes methodological limitations in the studies that assess behavioral outcomes [19]. Additionally, findings from studies by Kent et al. and Olson & Bialocerkowski indicate that IPE interventions in clinical settings significantly enhance students' collaborative clinical skills. Additionally, providing healthcare services in a coordinated and integrated way through team activities leads to better clinical performance [20, 21]. The findings of this study differ from these results, which may be attributed to inconsistencies in the implementation of IPE across various healthcare disciplines. Our study demonstrates that IPE is effective in enhancing students' clinical performance, and it is suggested that early integration of IPE from the start of the clinical phase could significantly improve the development of practical skills. Ayala et al., in their study titled "A Cross-Sectional Analysis of Perceptions of Interprofessional Education in Medical Students," found that fourth-year medical students with more extensive exposure to IPE in clinical settings demonstrated higher readiness and willingness for IPE compared to first-year students [22]. This underscores the significance of early IPE exposure in enhancing clinical performance.
Additionally, a study conducted by Christian et al., titled "Evaluating Attitudes Toward Interprofessional Collaboration and Education Among Health Professional Learners," predominantly highlights a positive attitude toward IPE among healthcare professionals [23]. Bedford et al., in a study titled "Supervision in Interprofessional Education: Benefits, Challenges, and Lessons Learned," revealed that IPE, despite its challenges, promotes collaboration and skills among participants by preparing students for teamwork [24]. Pakpour et al., in their study conducted in Iran titled "Viewpoint of Nurses on Inter-professional Relationship between Nurses and Doctors," emphasized the critical role of effective interprofessional collaboration in optimizing healthcare delivery. The study advocates for incorporating IPE into nursing and medical curricula to promote a collaborative culture and improve professional attitudes. The findings also show that nurses have a positive attitude toward IPE [25]. These results are consistent with our current study's findings, which highlight the establishment of positive attitudes and interprofessional learning among nursing and medical students.
The research findings of Ahmady et al. in their study titled "Challenges to the Implementation of Interprofessional Education in Health Profession Education in Iran" indicate that attitudes toward IPE and cultural issues pose significant challenges to the successful implementation of this approach [26]. Consequently, fostering a positive attitude toward IPE may greatly enhance its efficacy. Additionally, Berger-Estilita et al., in a study examining medical students’ attitudes toward IPE, found that female students and those with more extensive pre-clinical experience tended to exhibit more favorable attitudes toward IPE [27]. However, a systematic review by Berger-Estilita et al. titled “Attitudes Towards Interprofessional Education in the Medical Curriculum” demonstrated that integrating IPE within both pre-clinical and clinical phases of medical training fostered positive student attitudes toward this pedagogical approach [28]. Therefore, introducing IPE early in students' academic careers is essential to maximize its effectiveness.
Olson and Bialocerkowski, in their systematic review titled "Interprofessional Education in Allied Health," highlighted the significance of IPE in clinical settings and its role in enhancing healthcare outcomes. They also suggested conducting qualitative research to further evaluate IPE [21]. These findings are consistent with our study.
Conversely, Hulen et al., Luebbers et al., Mette et al., and Ng et al. emphasized the necessity of establishing infrastructure and organizational support to allocate funding, provide collaborative practice time, facilitate staff collaboration, and encourage student involvement to promote IPE [29-32].
Given the challenges students faced in mastering complex clinical procedures, which were further complicated by the constraints imposed by the Covid-19 pandemic, the focus was narrowed to a single foundational skill. This specific skill was considered essential for improving the quality and feasibility of implementation while ensuring patient safety. Additionally, the nursing staff in the surgical ward voiced concerns about the clinical competency of students, particularly medical students. Consequently, the evaluation of students’ dressing replacement skill was conducted using a manikin to mitigate potential risks to patients.
This study has several key strengths. Notably, it emphasized the IPE process within the clinical setting. In the current study, alongside the interprofessional attitude, the emphasis was placed on shared clinical skills. This dual emphasis ensures a comprehensive approach to enhancing teamwork and competency among medical and nursing students.
Several limitations of this research should be acknowledged. First, participants were restricted to students from two faculties, and the sample size was small; therefore, the generalizability of the findings may be limited. Due to the concurrent emergence of the Covid-19, pandemic and associated restrictions on student ward presence, this study was designed as a single-group educational intervention. Nonetheless, the integration of IPE within this context, characterized by its potential to enhance student clinical skill through learner motivation, small group collaboration, and mentorship, offers a valuable framework for future IPE delivery in clinical settings. Therefore, it is recommended that future studies be conducted with a larger sample size and a control group.
Implementing IPE courses and training workshops in various clinical settings can further enhance clinical skills and foster interprofessional collaboration among healthcare professionals. Rigorous evaluation of IPE's impact on patient care outcomes is crucial. Disseminating evidence-based research findings has been shown to effectively cultivate positive attitudes towards IPE and facilitate the learning process.
Conclusion
Our findings underscore the effectiveness of IPE in improving the clinical skills of both medical and nursing students, which in turn enhances patient care. The results also show a positive attitude among students towards IPE, with high mean attitude scores. Effective and practical implementation of IPE in health professions is crucial for cultivating a positive attitude toward this approach. Therefore, introducing students to IPE early on is essential for developing the necessary clinical skills and fostering a culture of interprofessional collaboration and teamwork. It is evident that IPE offers substantial benefits, and ensuring its proper implementation can lead to improved healthcare outcomes.
Ethical considerations
The protocol of the study was approved by the National Agency for Strategic Research in Medical Education. Tehran. Iran. under the identifier 980543. The ethical approval letter for this study was issued by the National Agency for Strategic Research in Medical Education (NASR) and is attached. The study purpose and importance were explained to participants. Participants were also assured that their data would remain confidential and that they could withdraw from the study at any time.
Artificial intelligence utilization for article writing
The authors confirm that generative Artificial Intelligence (AI) and AI-assisted technologies were not used in the writing process of this paper.
Acknowledgment
We highly appreciate the respectable faculty members and medical and nursing students who participated in this study.
Conflict of interest statement
The authors declare no conflict of interest in this study.
Author contributions
SD designed the study and drafted the manuscript. ZA conceived the initial idea for the study and contributed to the study design, data collection, statistical analysis, and final editing of the article. All authors read and approved the final manuscript.
Funding
This study was funded by the National Agency for Strategic Research in Medical Education in Tehran, Iran, under Grant No. 980543.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Background & Objective: Interprofessional education is widely recognized as a fundamental approach for fostering collaborative teamwork and enhancing healthcare delivery. This study examined the impact of an interprofessional education program on the attitudes and clinical skills of medical and nursing students in surgery wards.
Materials & Methods: This quasi-experimental study used a single group, pre- and post-test design. Ten 3-hour Interprofessional education sessions were held in the surgery ward for 10 small groups of medical and nursing students (n = 42). Pretests and posttests were administered using a checklist to evaluate the students' clinical skills in dressing replacement. Furthermore, the attitudes of both groups of students toward interprofessional education were assessed with a valid and reliable questionnaire following the educational intervention. Data were analyzed in SPSS software using chi-square, t-test, and Mann-Whitney U tests.
Results: A significant difference was observed in the mean scores for dressing replacement skills between medical and nursing students before and after the intervention (p < 0.001). The Mann-Whitney U test indicated that there was no significant difference in the mean scores for attitudes in the two domains of interaction-orientedness (p = 0.733) and professional compliance (p = 0.764).
Conclusion: The findings of this study suggest that interprofessional education can effectively enhance the clinical skills of both medical and nursing students, thereby promoting better patient care. It is crucial to foster a positive attitude among learners and educators through training programs to maximize the effectiveness of interprofessional education.
Introduction
IPE encourages students to cultivate a positive attitude toward collaborating with various healthcare professionals. It helps them understand and respect the unique roles and responsibilities of their colleagues, leading to better service delivery and fewer medical errors [5]. IPE serves as a fundamental element in building a strong and flexible healthcare workforce. It creates a positive environment and boosts motivation for collaboration among health professionals, thereby playing a crucial role in developing human resources that can provide efficient and responsive care [6]. Moreover, medical educators are increasingly recognizing the significance of integrating IPE into their curricula [2]. This emphasis arises from the understanding that solitary professional identity formation, devoid of IPE exposure, can hinder effective collaboration within the complex dynamics of the patient care team and pose challenges for future professional trajectories [1].
Ineffective collaboration between physicians and nurses can result in lower-quality patient care, reduced job satisfaction, and increased treatment costs. Therefore, IPE is a vital part of healthcare education, especially for nursing and medical students [7]. Hence, effective IPE implementation is expected to reduce medical errors, boost patient satisfaction, and ultimately culminate in improved patient care outcomes [3].
Integrating IPE into medical science curricula is essential for ensuring patient safety [8]. Research highlights IPE's effectiveness in promoting interprofessional thinking, patient-centered care, shared knowledge, and improved mutual understanding [1]. Research on the effectiveness of IPE shows that it positively affects teamwork and communication skills among participants [1, 9, 10]. Studies on IPE in clinical settings underscore its critical role in improving communication, teamwork, and, ultimately, patient care and safety [4, 11]. A Best Evidence Medical Education (BEME) guide supports these findings, highlighting IPE's impact on learner attitudes and learning [8]. Although there is ample evidence supporting IPE, it remains underrecognized and is not effectively utilized in educational institutions within the country [12]. IPE can improve attitudes toward teamwork and collaboration, potentially leading to better patient care post-graduation. However, the optimal timing for introducing medical students to IPE remains a matter of debate [13]. This investigation was motivated by a perceived lack of IPE in our university's surgery ward. Given the documented benefits of IPE and the paucity of research examining its efficacy in clinical settings, this investigation aimed to assess the impact of IPE on the clinical skills and attitudes of medical and nursing students.
Materials & Methods
Design and setting(s)
This quasi-experimental study used a single group, pre- and post-test design at Birjand University of Medical Sciences in Iran from 21 April 2022 to 22 July 2022. It is important to note that random selection of students was not possible, as they had already been assigned to apprenticeship groups by the faculty.
Participants and sampling
The study population comprised all medical and nursing students in the clinical phase of their respective programs who were willing to participate. It is important to note that students who were absent for more than one day were excluded from the study. Additionally, eight nursing students opted not to participate. A total of 42 students were recruited using the census method (Figure 1).
Tools/Instruments
The demographic information form collected data on participants' age, gender, field of study, and GPA.
A dressing replacement skill checklist was created based on a standard nursing textbook to evaluate student skills before and after the IPE intervention. This checklist consisted of 16 dichotomous items (yes/no, 1/0), corresponding to the procedural steps of dressing replacement. Each item was scored as either correct or left blank. The total score for each student ranged from 0 to 20 to facilitate easier interpretation and analysis.
Content validity was established through expert review by ten clinical nursing and medical faculty members from the surgery ward. To confirm the face validity of the checklist, it was administered to 20 nursing students. Test-retest reliability for the dressing replacement skill checklist was assessed using Pearson’s correlation coefficient over a two-week interval (r = 0.55, p = 0.011, n = 20), indicating a moderate level of temporal stability for the tool.
Medical and nursing students completed a questionnaire to assess their attitudes toward IPE following the educational intervention. We utilized the Attitudes to IPE Questionnaire, which had been previously translated into Persian in Sohrabi et al.'s study, where its validity and reliability were confirmed [14]. We referenced this study in our article. In the Sohrabi et al. study, the original 15-item instrument was translated into Persian and underwent a psychometric evaluation to confirm its content, structure, and construct validity, as well as its internal consistency and test-retest reliability. Ten participants and 10 experts assessed content validity and content validity index; construct validity was evaluated using exploratory factor analysis. According to the impact item score above 1.5, the index of content validity of 0.62, and the content validity index of 0.7, 12 questions were preserved. Based on exploratory factor analysis, 12 items were kept in scale. The final questionnaire consisted of 12 items that participants responded to using a 5-point Likert scale, ranging from "completely agree" to "completely disagree." The questionnaire items focused on two primary constructs: interaction-orientedness (8 items) and professional compliance (4 items). The reliability of the attitude scale was established by computing the stability coefficient (Spearman’s ρ = 0.92) and internal consistency (Cronbach’s ά = 0.866) [14].
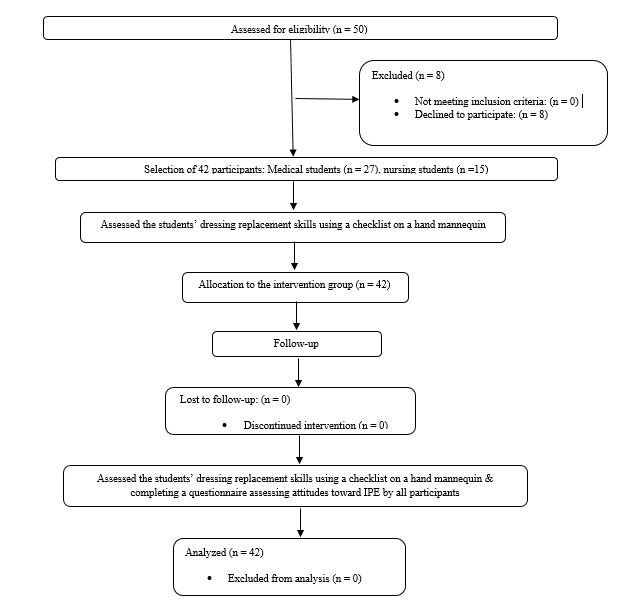
Figure 1. Flow chart of the study
Data collection methods
The educational intervention was delivered through an IPE program integrated into the formal coursework.
Clinical faculty members from both medicine and nursing, who are responsible for the undergraduate curricula in the surgical ward, were brought together to discuss the rationale for implementing IPE. A comprehensive analysis of common essential competencies/skills within the surgical context was conducted, drawing upon both medical and nursing curricula. Participants were asked to identify a fundamental skill that is essential for all students. Due to a preference for skills that are readily attainable, the dressing replacement skill was chosen as the selected competency.
Prior to the intervention, a briefing session was conducted to familiarize students with the concept of IPE. Before the start of the IPE training sessions, a pretest was administered to evaluate students’ dressing replacement skills using a manikin. The assessor was a senior nursing graduate who had experience working in the surgical department. Ten small groups were formed, each comprising four to five nursing (consisting of eighth semester nursing students) and medical students (consisting of fourth and sixth year medical students) in clinical phases who were willing to participate in the study. A master's degree in nursing with surgical ward experience and a surgical chief resident served as mentors for these learning cohorts. Before the intervention, to ensure proper skill transfer by students in both groups, medical students underwent targeted training in history-taking under the mentorship of the surgical chief resident. Nursing students training in dressing replacement began with an instructional video, followed by guided practice under the supervision of a mentor. Each group of medical and nursing students was then assigned two patients, for whom they were responsible during their clinical training, with oversight from a supervisor.
Efforts were made to ensure that nursing students were present while medical students took the patients' histories. Similarly, medical students were present when nursing students changed the dressings. The program spanned two weeks, encompassing ten three-hour sessions conducted in the surgery ward between 8:00 AM and 11:00 AM. This timeframe allowed for concurrent skill training and patient care. After the intervention, the students’ dressing replacement skills were reevaluated using the same checklist on the
manikin. One by one, students entered the testing room and were asked to dress a wound on a hand mannequin. The observer, who was a senior nurse with clinical experience, assessed their skills using a checklist. Additionally, students completed the attitude questionnaire upon program conclusion.
Data analysis
Because the data did not follow a normal distribution, non-parametric tests were used for data analysis. The Wilcoxon test was employed to compare the mean scores of dressing replacement skills before and after the intervention, while the Mann-Whitney test was used to compare the interprofessional attitude mean scores between medical and nursing students. Data analysis was conducted using SPSS version 23.
Results
The study sample consisted of 42 students (54.8% female, n = 23; 45.2% male, n = 19), with a mean age of 23.9 ± 3.03 years (Table 1). The results of the statistical tests indicated no significant differences between medical and nursing students regarding the variables analyzed (age, gender, and GPA), demonstrating that the groups were homogeneous (p > 0.05).
Table 1. Demographic characteristics of the students (n = 42)
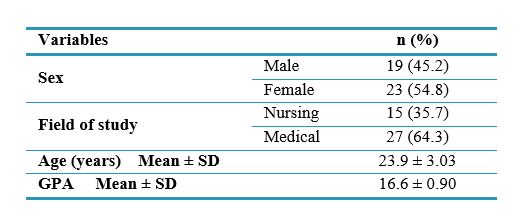
Abbreviations: n, number of participants; SD, standard deviation; GPA, grade point average.
A significant difference was observed in the mean scores for dressing replacement skills (out of 20) before and after the intervention (p < 0.001) (Table 2, Figure 2).
Table 2. Comparison of mean scores for dressing replacement skill before and after the intervention
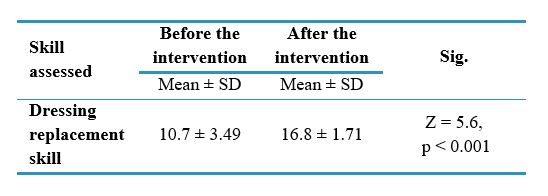
Notes: Wilcoxon was used to compare mean scores of the dressing replacement skill before and after the intervention
Abbreviations: SD, standard deviation; Sig., statistical significance.
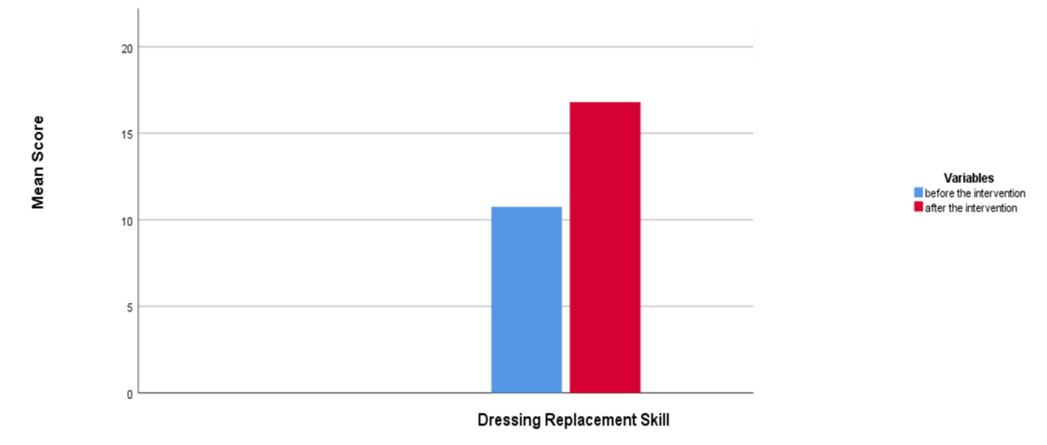
Figure 2. Comparison of mean scores of the dressing replacement skill before and after the intervention
The mean scores for dressing replacement skills in both medical and nursing students were significantly higher after the IPE intervention compared to before (p < 0.001). Additionally, a significant difference was observed in the mean scores of dressing replacement skills between medical and nursing students both before and after the intervention (p < 0.001), with nursing students achieving higher mean scores than their medical counterparts. In terms of attitudes, the mean score for the domain of interaction-orientedness was 36.1 ± 2.61 for medical students and 36.0 ± 2.66 for nursing students. For the domain of professional compliance, the mean scores were 17.0 ± 1.60 for medical students and 16.7 ± 1.53 for nursing students. The results of the Mann-Whitney U test indicated that both groups were similar, with no significant differences observed in the mean scores for attitudes in the domains of interaction-orientedness and professional compliance (Table 3).
Table 3. Comparison of interprofessional attitude mean scores between medical and nursing students
Notes: * Mann-Whitney was used to compare the interprofessional attitude mean scores in medical and nursing students
Abbreviations: SD, standard deviation; p, probability-value
Discussion
This study sought to determine the impact of an IPE program on the clinical skills and attitudes of medical and nursing students. The results showed that the mean dressing replacement skill score in both groups of students increased significantly after the IPE intervention. These findings support the effectiveness of the IPE program in enhancing dressing replacement skills. The results demonstrated a significant difference in mean scores between the two groups of students both before and after the intervention. Notably, nursing students demonstrated higher baseline mean scores, potentially attributable to prior exposure to related competencies and increased practical experience. While nursing students maintained a performance advantage after the intervention, the disparity between groups was lessened, highlighting the IPE program’s particular benefit for medical students in acquiring this clinical skill. The pronounced initial skill discrepancy between the two disciplines underscores the imperative for interprofessional learning to optimize clinical skills and teamwork. Analysis of student attitudes toward the IPE program revealed high mean scores, reflecting a positive disposition toward IPE. A comparative analysis of mean attitude scores between nursing and medical students yielded no significant differences, suggesting a shared positive attitude towards IPE and alignment across both domains of the questionnaire (interaction-orientedness and professional compliance).
Research has explored IPE within clinical settings [4, 11]. Braun et al.'s study titled "Impact of Interprofessional Education for Medical and Nursing Students on the Nutritional Management of In-Patients" employed IPE across different student groups. The study aimed to develop skills in patient-centered care, professional role development, communication, teamwork, ethical decision-making, and patient advocacy. The results demonstrate that learners' clinical performance is enhanced as their roles and understanding of their professions evolve [11].
IPE has proven to be an effective teaching approach in clinical environments. Research by Dyess et al., Renschler et al., Cino et al., and Mahdizadeh et al. demonstrate that IPE greatly improves students' knowledge and clinical skills. Additionally, by promoting collaborative learning and teamwork, IPE has the potential to substantially enhance patient safety outcomes [3, 4, 15, 16]. These findings are consistent with our study on the effectiveness of IPE in a clinical setting. The results of Renschler et al.'s study, titled “Effect of Interprofessional Clinical Education Programme Length on Students’ Attitudes Towards Teamwork,” indicated that IPE in clinical settings improves students’ understanding of professional roles and responsibilities, ultimately leading to better patient care [4]. A study by Mahdizadeh et al. titled "Clinical Interdisciplinary Collaboration Models and Frameworks: From Similarities to Differences," conducted as a systematic review, highlights the importance of interprofessional collaboration between physicians and nurses in clinical settings. The study's findings reveal that successful implementation of these partnerships can lead to fewer adverse events and better patient outcomes. This collaborative model shows great potential for enhancing the efficiency and safety of patient care across various healthcare stakeholders [15]. However, the results of a systematic review conducted by Dyess et al. titled "Impact of Interprofessional Education on Students of the Health Professions" highlights that establishing and maintaining interprofessional collaboration within a multidisciplinary surgery team with diverse characteristics is complex. This complexity can influence practices and patient care [3]. Barrios and Torres, in a study titled "Interprofessional Health Education Teacher Training at the University of Chile," emphasized that the main goal of IPE is to prepare learners to improve their professional roles within healthcare teams. Therefore, teachers need to be equipped to function as effective and supportive interprofessional teams as well. They recommend that teachers employ practical strategies to enhance the effectiveness and success of IPE [17]. A study by Irajpour et al. titled "Situation Analysis and Designing an Interprofessional Curriculum for Palliative Care of Cancer Patients" conducted in Iran, revealed that IPE can be a fundamental framework for promoting collaborative care among healthcare providers addressing the complex needs of palliative care patients [18]. The findings of this study align with our research, which demonstrates the potential of IPE to enhance patient care. However, one possible explanation for the lack of significant differences in attitudes between the two groups of medical and nursing students is the limited duration of exposure to the IPE program.
Mattiazzi et al. conducted a systematic literature review titled "Behavioral Outcomes of Interprofessional Education within Clinical Settings for Health Professional Students," which found that IPE in clinical settings can help students develop competencies in interprofessional collaborative practice. However, the review also notes methodological limitations in the studies that assess behavioral outcomes [19]. Additionally, findings from studies by Kent et al. and Olson & Bialocerkowski indicate that IPE interventions in clinical settings significantly enhance students' collaborative clinical skills. Additionally, providing healthcare services in a coordinated and integrated way through team activities leads to better clinical performance [20, 21]. The findings of this study differ from these results, which may be attributed to inconsistencies in the implementation of IPE across various healthcare disciplines. Our study demonstrates that IPE is effective in enhancing students' clinical performance, and it is suggested that early integration of IPE from the start of the clinical phase could significantly improve the development of practical skills. Ayala et al., in their study titled "A Cross-Sectional Analysis of Perceptions of Interprofessional Education in Medical Students," found that fourth-year medical students with more extensive exposure to IPE in clinical settings demonstrated higher readiness and willingness for IPE compared to first-year students [22]. This underscores the significance of early IPE exposure in enhancing clinical performance.
Additionally, a study conducted by Christian et al., titled "Evaluating Attitudes Toward Interprofessional Collaboration and Education Among Health Professional Learners," predominantly highlights a positive attitude toward IPE among healthcare professionals [23]. Bedford et al., in a study titled "Supervision in Interprofessional Education: Benefits, Challenges, and Lessons Learned," revealed that IPE, despite its challenges, promotes collaboration and skills among participants by preparing students for teamwork [24]. Pakpour et al., in their study conducted in Iran titled "Viewpoint of Nurses on Inter-professional Relationship between Nurses and Doctors," emphasized the critical role of effective interprofessional collaboration in optimizing healthcare delivery. The study advocates for incorporating IPE into nursing and medical curricula to promote a collaborative culture and improve professional attitudes. The findings also show that nurses have a positive attitude toward IPE [25]. These results are consistent with our current study's findings, which highlight the establishment of positive attitudes and interprofessional learning among nursing and medical students.
The research findings of Ahmady et al. in their study titled "Challenges to the Implementation of Interprofessional Education in Health Profession Education in Iran" indicate that attitudes toward IPE and cultural issues pose significant challenges to the successful implementation of this approach [26]. Consequently, fostering a positive attitude toward IPE may greatly enhance its efficacy. Additionally, Berger-Estilita et al., in a study examining medical students’ attitudes toward IPE, found that female students and those with more extensive pre-clinical experience tended to exhibit more favorable attitudes toward IPE [27]. However, a systematic review by Berger-Estilita et al. titled “Attitudes Towards Interprofessional Education in the Medical Curriculum” demonstrated that integrating IPE within both pre-clinical and clinical phases of medical training fostered positive student attitudes toward this pedagogical approach [28]. Therefore, introducing IPE early in students' academic careers is essential to maximize its effectiveness.
Olson and Bialocerkowski, in their systematic review titled "Interprofessional Education in Allied Health," highlighted the significance of IPE in clinical settings and its role in enhancing healthcare outcomes. They also suggested conducting qualitative research to further evaluate IPE [21]. These findings are consistent with our study.
Conversely, Hulen et al., Luebbers et al., Mette et al., and Ng et al. emphasized the necessity of establishing infrastructure and organizational support to allocate funding, provide collaborative practice time, facilitate staff collaboration, and encourage student involvement to promote IPE [29-32].
Given the challenges students faced in mastering complex clinical procedures, which were further complicated by the constraints imposed by the Covid-19 pandemic, the focus was narrowed to a single foundational skill. This specific skill was considered essential for improving the quality and feasibility of implementation while ensuring patient safety. Additionally, the nursing staff in the surgical ward voiced concerns about the clinical competency of students, particularly medical students. Consequently, the evaluation of students’ dressing replacement skill was conducted using a manikin to mitigate potential risks to patients.
This study has several key strengths. Notably, it emphasized the IPE process within the clinical setting. In the current study, alongside the interprofessional attitude, the emphasis was placed on shared clinical skills. This dual emphasis ensures a comprehensive approach to enhancing teamwork and competency among medical and nursing students.
Several limitations of this research should be acknowledged. First, participants were restricted to students from two faculties, and the sample size was small; therefore, the generalizability of the findings may be limited. Due to the concurrent emergence of the Covid-19, pandemic and associated restrictions on student ward presence, this study was designed as a single-group educational intervention. Nonetheless, the integration of IPE within this context, characterized by its potential to enhance student clinical skill through learner motivation, small group collaboration, and mentorship, offers a valuable framework for future IPE delivery in clinical settings. Therefore, it is recommended that future studies be conducted with a larger sample size and a control group.
Implementing IPE courses and training workshops in various clinical settings can further enhance clinical skills and foster interprofessional collaboration among healthcare professionals. Rigorous evaluation of IPE's impact on patient care outcomes is crucial. Disseminating evidence-based research findings has been shown to effectively cultivate positive attitudes towards IPE and facilitate the learning process.
Conclusion
Our findings underscore the effectiveness of IPE in improving the clinical skills of both medical and nursing students, which in turn enhances patient care. The results also show a positive attitude among students towards IPE, with high mean attitude scores. Effective and practical implementation of IPE in health professions is crucial for cultivating a positive attitude toward this approach. Therefore, introducing students to IPE early on is essential for developing the necessary clinical skills and fostering a culture of interprofessional collaboration and teamwork. It is evident that IPE offers substantial benefits, and ensuring its proper implementation can lead to improved healthcare outcomes.
Ethical considerations
The protocol of the study was approved by the National Agency for Strategic Research in Medical Education. Tehran. Iran. under the identifier 980543. The ethical approval letter for this study was issued by the National Agency for Strategic Research in Medical Education (NASR) and is attached. The study purpose and importance were explained to participants. Participants were also assured that their data would remain confidential and that they could withdraw from the study at any time.
Artificial intelligence utilization for article writing
The authors confirm that generative Artificial Intelligence (AI) and AI-assisted technologies were not used in the writing process of this paper.
Acknowledgment
We highly appreciate the respectable faculty members and medical and nursing students who participated in this study.
Conflict of interest statement
The authors declare no conflict of interest in this study.
Author contributions
SD designed the study and drafted the manuscript. ZA conceived the initial idea for the study and contributed to the study design, data collection, statistical analysis, and final editing of the article. All authors read and approved the final manuscript.
Funding
This study was funded by the National Agency for Strategic Research in Medical Education in Tehran, Iran, under Grant No. 980543.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2024/10/6 | Accepted: 2025/03/30 | Published: 2025/04/14
Received: 2024/10/6 | Accepted: 2025/03/30 | Published: 2025/04/14
References
1. Park YC, Park KH. Interprofessional education program for medical and nursing students: interprofessional versus uniprofessional. Korean Journal of Medical Education. 2021;33(1):1-10. [DOI]
2. Smith BS, Anderson K. Attitudes toward interprofessional education: comparing physical
therapist and other health care professions' students. Journal of Physical Therapy Education. 2018;32(2):183-90 [DOI]
3. Dyess AL, Brown JS, Brown ND, Flautt KM, Barnes LJ. Impact of interprofessional education on students of the health professions: a systematic review. Journal of Educational Evaluation for Health Professions. 2019;16 [DOI]
4. Renschler L, Rhodes D, Cox C. Effect of interprofessional clinical education programme length on students’ attitudes towards teamwork. Journal of Interprofessional Care. 2016;30(3):338-46 [DOI]
5. Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews. 2013(3) [DOI]
6. Khossravi Shoobe J, Khaghanizade m, Parandeh a, vafadar z. Effectiveness of educational workshop based on interprofessional approach in changing health science students’ attitudes towards interprofessional learning and collaboration. Bimonthly of Education Strategies in Medical Sciences. [Online]. Available from: [Accessed: Feb. 26, 2025] [DOI]
7. Aghamohammadi D, Dadkhah B, Aghamohammadi M, Nasiri E. Inter professional collaboration: attitude of nurses and physicians of Ardabil's intensive care units. Journal of Health and Care. [Online]. Available from: [Accessed: Feb. 26, 2025] [DOI]
8. Reeves S, Fletcher S, Barr H, et al. A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Medical Teacher. 2016;38(7):656-68 [DOI]
9. Lin YC, Chan TF, Lai CS, Chin CC, Chou FH, Lin HJ. The impact of an interprofessional problem-based learning curriculum of clinical ethics on medical and nursing students' attitudes and ability of interprofessional collaboration: a pilot study. The Kaohsiung Journal of Medical Sciences. 2013;29(9):505-11. [DOI]
10. Berger S, Mahler C, Krug K, Szecsenyi J, Schultz J-H. Evaluation of interprofessional education: lessons learned through the development and implementation of an interprofessional seminar on team communication for undergraduate health care students in Heidelberg–a project report. GMS Journal for Medical Education. 2016;33(2) [DOI]
11. Braun B, Grünewald M, Adam-Paffrath R, et al. Impact of interprofessional education for medical and nursing students on the nutritional management of in-patients. GMS Journal for Medical Education. 2019;36(2). [DOI]
12. vafadar Z, Vanaki Z, Ebadi A. An overview of the most prominent applied models of inter-professional education in health sciences in the world. Research in Medical Education. 2017;8(4):69-80 [DOI]
13. Makino T, Shinozaki H, Hayashi K, et al. Attitudes toward interprofessional healthcare teams: a comparison between undergraduate students and alumni. Journal of Interprofessional Care. 2013;27(3):261-8. [DOI]
14. Sohrabi Z, Saeed A, Salehi L. Investigation of the validity and reliability of attitude towards inter-professional education (IPE) in health care. Iranian Journal of Health Education and Health Promotion. 2018;6(1):12-9. [DOI]
15. Cino K, Austin R, Casa C, Nebocat C, Spencer A. Interprofessional ethics education seminar for undergraduate health science students: a pilot study. Journal of Interprofessional Care. 2018;32(2):239-41 [DOI]
16. Mahdizadeh M, Heydari A, Moonaghi HK. Clinical interdisciplinary collaboration models and frameworks from similarities to differences: a systematic review. Global Journal of Health Science. 2015;7(6):170 [DOI]
17. Barrios ME, Torres SO. Interprofessional health education teacher training at the university of Chile. Journal of Educational Evaluation for Health Professions. 2021;18 [DOI]
18. Irajpour A, Alavi M, Izadikhah A. Situation analysis and designing an interprofessional curriculum for palliative care of the cancer patients. Iranian Journal of Medical Education. [Online]. Available from: [Accessed: Feb. 26, 2025] [DOI]
19. Mattiazzi S, Cottrell N, Ng N, Beckman E. Behavioural outcomes of interprofessional education within clinical settings for health professional students: a systematic literature review. Journal of Interprofessional Care. 2024;38(2):294-307 [DOI]
20. Kent F, Hayes J, Glass S, Rees CE. Pre‐registration interprofessional clinical education in the workplace: a realist review. Medical Education. 2017;51(9):903-17. [DOI]
21. Olson R, Bialocerkowski A. Interprofessional education in allied health: a systematic review. Medical Education. 2014;48(3):236-46. [DOI]
22. Ayala N, MacDonnell P, Dumenco L, Dollase R, George P. A cross-sectional analysis of perceptions of interprofessional education in medical students. Annals of Behavioral Science and Medical Education. 2014;20(2):6-9 [DOI]
23. Christian LW, Hassan Z, Shure A, Joshi K, Lillie E, Fung K. Evaluating attitudes toward interprofessional collaboration and education among health professional learners. Medical Science Educator. 2020;30:467-78 [DOI]
24. Bedford S, Repa L, Renouf A. Supervision in interprofessional education: benefits, challenges, and lessons learned. Journal of Psychotherapy Integration. 2020;30(1):16 [DOI]
25. Pakpour V, Hojat M, Salehi H, Rahmani A, Shahim A, Mohammadi R. Viewpoint of nurses on inter-professional relationship between nurses and doctors. Journal of Hayat. [Online]. Available from: [Accessed: Feb. 26, 2025] [DOI]
26. Ahmady S, Mirmoghtadaie Z, Rasouli D. Challenges to the implementation of interprofessional education in health profession education in Iran. Advances in Medical Education and Practice.
2020:227-36. [DOI]
27. Berger-Estilita J, Chiang H, Stricker D, Fuchs A, Greif R, McAleer S. Attitudes of medical students towards interprofessional education: a mixed-methods study. PLOS One. 2020;15(10): e0240835. [DOI]
28. Berger-Estilita J, Fuchs A, Hahn M, Chiang H, Greif R. Attitudes towards Interprofessional education in the medical curriculum: a systematic review of the literature. BMC Medical Education. 2020;20:1-17. [DOI]
29. Hulen E, Edwards ST, Poppe AP, Singh MK, Shunk R, Tuepker A. Creating change, challenging structure: graduate and faculty perspectives on the implementation of an interprofessional education program in veterans affairs primary care. Journal of Interprofessional Care. 2020;34(6):756-62 [DOI]
30. Luebbers EL, Dolansky MA, Vehovec A, Petty G. Implementation and evaluation of a community-based interprofessional learning activity. Journal of Interprofessional Care. 2017;31(1):91-7. [DOI]
31. Mette M, Baur C, Hinrichs J, Narciß E. Gaining interprofessional knowledge and interprofessional competence on a training ward. Medical Teacher. 2021;43(5):583-9. [DOI]
32. Ng E, Hu T, McNaughton N, Martimianakis MA. Transformative learning in an interprofessional student-run clinic: a qualitative study. Journal of Interprofessional Care. 2021;35(5):701-9. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




