Sun, Feb 1, 2026
[Archive]
Volume 16, Issue 50 (2023)
J Med Edu Dev 2023, 16(50): 21-27 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Anil D, Kumar D S, Murthy M R N. Self-directed learning: The impact among medical students. J Med Edu Dev 2023; 16 (50) :21-27
URL: http://edujournal.zums.ac.ir/article-1-1792-en.html
URL: http://edujournal.zums.ac.ir/article-1-1792-en.html
1- Department of Community Medicine JSS Medical College, JSS Academy of Higher Education and Research. , deepakanil7@gmail.com
2- Professor and Head, Department of Community Medicine, Department of Community Medicine, JSS Medical College, JSS Academy of Higher Education and Research, Sri Shivarathreeshwara Nagara, Mysuru- 570015, Karnataka, India.
3- Professor, Department of Community Medicine, JSS Medical College, JSS Academy of Higher Education and Research
2- Professor and Head, Department of Community Medicine, Department of Community Medicine, JSS Medical College, JSS Academy of Higher Education and Research, Sri Shivarathreeshwara Nagara, Mysuru- 570015, Karnataka, India.
3- Professor, Department of Community Medicine, JSS Medical College, JSS Academy of Higher Education and Research
Keywords: Medical education, Problem-based learning, Academic performance, Adult learning, Geographical Information System
Full-Text [PDF 406 kb]
(1254 Downloads)
| Abstract (HTML) (3550 Views)
Full-Text: (993 Views)
Abstract
Introduction
Self-Directed Learning (SDL) is seen as an important component of lifelong learning and is thus emphasized in medical school curricula. Medical education systems around the world have embraced SDL for medical students to develop SDL skills to continually equip themselves with relevant information and abilities in the ever-changing world of medicine (1). Due to the difficulty in memorizing vast medical information and complicated medical practices, SDL has become essential for health professionals to maintain competency by continuous learning and seeking knowledge upgrades throughout their careers (2,3).
Self-directed learning has been recognized as the most acceptable way of learning for adults and is described in determining what to learn and how much to learn. Individuals choose, manage, and evaluate their learning activities, which they can do at any time, in any location, using any method, and at any age (4). Self-directed learning is a process in which individuals assess their learning needs, formulate learning goals, discover human and material resources for learning, choose and apply appropriate learning strategies, and evaluate learning outcomes on their own or with the help of others (4,5). In recent years, there has been an increase in using student-centered methodologies such as problem-based learning (PBL) that emphasize SDL in medical education. The acceptance of such approaches is not universal, and it varies between cultures and countries (6).
SDL has been carried out in a variety of ways. It is preferable if the objectives are concrete so that learners do not struggle to achieve them while learning on their own. Giving case-based scenarios and guiding learners with questions, directing them to solutions using MBBS, making it the country with the maximum number of medical colleges and during this pandemic period, it is critical to maintain medical education in all colleges across the country (8). Undergraduate medical education in India follows a set of universal criteria for higher medical degrees, which states that Indian medical graduates should be lifelong learners committed to developing their skills and knowledge. They aim to produce graduates with the necessary knowledge, skills, attitudes and patient responsiveness to deliver appropriate and effective first-contact treatment for a community (1,9).
JSS Medical College is an eminent medical education institution in Mysuru, Karnataka, India. It has emerged as a renowned institute in the country by providing medical education of high standards and compassionate health care programs through internationalization and innovation in academic and research studies. The Institution is equipped with excellent state-of-the-art infrastructure, laboratories, and modern teaching aids. Chart discussions, tutorials, student seminars, e-learning, integrated Learning Programs, early clinical exposures, laboratory practicals, community projects, bedside clinics, research projects and secondary hospital programs are all opportunities for SDL within the curriculum (10).
Assessing junior students’ SDL abilities is seen as a vital component that will aid in identifying areas for improvement during the early stages of the program, where intervention may be possible.
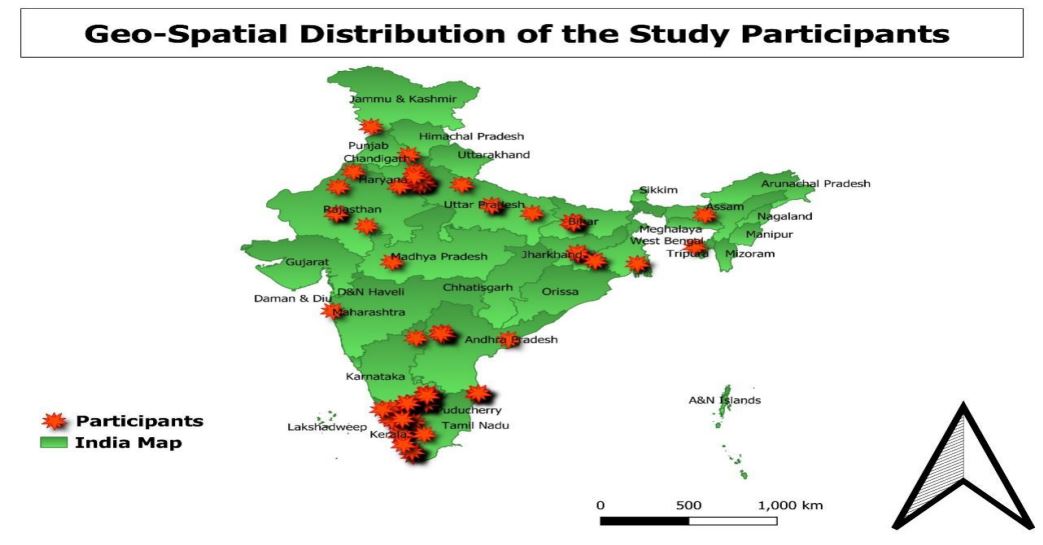
The objectives of the current study were to assess the impact of self-directed learning on medical students; to assess the perception of students regarding self-directed learning and to record the geospatial distribution of participants.
Material & methods
Design and setting(s)
A longitudinal study was conducted by researchers from the Department of Community Medicine, JSS Medical College, Mysuru. The study surveyed first-year medical students for two months (August 2021- September 2021) after obtaining approval from the Institutional Ethics Committee.
Participants and sampling
Expecting an overall online survey response rate of 80%, at a confidence interval of 95% and an absolute precision of 7%, the sample size was calculated as 125.
Sample size, n=Z2PQ÷L2, where Z = 1.96; P = 80% for the survey response rate, Q= (100-P) and d = 7%. As a result, the minimum number of participants required for this study was calculated to be 125 (Total responses-131). The study included all first-year medical students from JSS Medical College, Mysuru. Purposive sampling was used to collect data and all first-year medical students (N = 200) were required to complete the SDL assignment, but only those who signed individual consent forms (N = 131) were included in this study.
The participants rated the self-directed learning exercise on a scale of 1–5 (1 being the lowest and 5 being the highest) with 59.54 % of participants strongly agreeing with the self-directed learning program and 3.06 % unsure about it. (Table 2,3)
Discussion
Background & objective: Self-Directed Learning (SDL) has grown popular in the medical curriculum and is recommended as an effective learning approach for medical students. As medical research is continuously changing and information is exploding, it is critical to prepare doctors for SDL. The present study aimed to assess the impact and perception of SDL among medical students.
Materials & methods: This longitudinal study was done among 131 first-year medical students for 2 months. A poster competition was conducted and the students were asked to give their feedback through an online Google form, one week after the competition. Descriptive statistics were applied and analyzed using SPSS software. The location of the participants was obtained, and the geographical data were analyzed in the Quantum Geographical Information System (QGIS).
Results: Among the 131 study participants, 61.8% were female. Almost 94.7% of participants informed SDL was a helpful learning approach and 97.7% informed it had helped them learn at their own pace. SDL exercises also helped the participants determine their level of readiness to learn (52.67%), set learning goals (56.48%), engage in the learning process (75.57%), and evaluate their learning (47.33%).
Conclusion: SDL was deemed beneficial by the majority of participants in terms of grasping the subject and studying at their own speed. Studies correlating the SDL perception and the student’s academic performance are lacking, which makes it difficult to predict their success in the upcoming exams. As a result, additional research is needed in this area.
Materials & methods: This longitudinal study was done among 131 first-year medical students for 2 months. A poster competition was conducted and the students were asked to give their feedback through an online Google form, one week after the competition. Descriptive statistics were applied and analyzed using SPSS software. The location of the participants was obtained, and the geographical data were analyzed in the Quantum Geographical Information System (QGIS).
Results: Among the 131 study participants, 61.8% were female. Almost 94.7% of participants informed SDL was a helpful learning approach and 97.7% informed it had helped them learn at their own pace. SDL exercises also helped the participants determine their level of readiness to learn (52.67%), set learning goals (56.48%), engage in the learning process (75.57%), and evaluate their learning (47.33%).
Conclusion: SDL was deemed beneficial by the majority of participants in terms of grasping the subject and studying at their own speed. Studies correlating the SDL perception and the student’s academic performance are lacking, which makes it difficult to predict their success in the upcoming exams. As a result, additional research is needed in this area.
Introduction
Self-Directed Learning (SDL) is seen as an important component of lifelong learning and is thus emphasized in medical school curricula. Medical education systems around the world have embraced SDL for medical students to develop SDL skills to continually equip themselves with relevant information and abilities in the ever-changing world of medicine (1). Due to the difficulty in memorizing vast medical information and complicated medical practices, SDL has become essential for health professionals to maintain competency by continuous learning and seeking knowledge upgrades throughout their careers (2,3).
Self-directed learning has been recognized as the most acceptable way of learning for adults and is described in determining what to learn and how much to learn. Individuals choose, manage, and evaluate their learning activities, which they can do at any time, in any location, using any method, and at any age (4). Self-directed learning is a process in which individuals assess their learning needs, formulate learning goals, discover human and material resources for learning, choose and apply appropriate learning strategies, and evaluate learning outcomes on their own or with the help of others (4,5). In recent years, there has been an increase in using student-centered methodologies such as problem-based learning (PBL) that emphasize SDL in medical education. The acceptance of such approaches is not universal, and it varies between cultures and countries (6).
SDL has been carried out in a variety of ways. It is preferable if the objectives are concrete so that learners do not struggle to achieve them while learning on their own. Giving case-based scenarios and guiding learners with questions, directing them to solutions using MBBS, making it the country with the maximum number of medical colleges and during this pandemic period, it is critical to maintain medical education in all colleges across the country (8). Undergraduate medical education in India follows a set of universal criteria for higher medical degrees, which states that Indian medical graduates should be lifelong learners committed to developing their skills and knowledge. They aim to produce graduates with the necessary knowledge, skills, attitudes and patient responsiveness to deliver appropriate and effective first-contact treatment for a community (1,9).
JSS Medical College is an eminent medical education institution in Mysuru, Karnataka, India. It has emerged as a renowned institute in the country by providing medical education of high standards and compassionate health care programs through internationalization and innovation in academic and research studies. The Institution is equipped with excellent state-of-the-art infrastructure, laboratories, and modern teaching aids. Chart discussions, tutorials, student seminars, e-learning, integrated Learning Programs, early clinical exposures, laboratory practicals, community projects, bedside clinics, research projects and secondary hospital programs are all opportunities for SDL within the curriculum (10).
Assessing junior students’ SDL abilities is seen as a vital component that will aid in identifying areas for improvement during the early stages of the program, where intervention may be possible.
The objectives of the current study were to assess the impact of self-directed learning on medical students; to assess the perception of students regarding self-directed learning and to record the geospatial distribution of participants.
Material & methods
Design and setting(s)
A longitudinal study was conducted by researchers from the Department of Community Medicine, JSS Medical College, Mysuru. The study surveyed first-year medical students for two months (August 2021- September 2021) after obtaining approval from the Institutional Ethics Committee.
Participants and sampling
Expecting an overall online survey response rate of 80%, at a confidence interval of 95% and an absolute precision of 7%, the sample size was calculated as 125.
Sample size, n=Z2PQ÷L2, where Z = 1.96; P = 80% for the survey response rate, Q= (100-P) and d = 7%. As a result, the minimum number of participants required for this study was calculated to be 125 (Total responses-131). The study included all first-year medical students from JSS Medical College, Mysuru. Purposive sampling was used to collect data and all first-year medical students (N = 200) were required to complete the SDL assignment, but only those who signed individual consent forms (N = 131) were included in this study.
A poster competition was conducted among the first-year medical students of JSS Medical College, Mysuru, for which they were tasked with preparing a poster on sex ratio in India as part of their curriculum (NMC Competency - CM 9.1: Demography, demographic cycle, vital statistics). The feedback of the students on how this process had helped them in learning was assessed using an online questionnaire that was developed by the research team and validated by other subject experts.
Tools/Instruments
A pretested, semi-structured questionnaire was used to collect data from the participants. The questionnaire consisted of two parts. The first part of the questionnaire asked for sociodemographic details including, gender and address. The second section asked about the student’s perception of SDL, how it improved their learning and how much was this learning exercise beneficial to the participants (Likert scale, where 5=strongly agree,4= agree, 3=unsure, 2=disagree and 1=strongly disagree). A pilot study was conducted on 20 third-year students to assess the questionnaire’s accuracy and comprehension, who were later eliminated from the study. The Cronbach’s alpha score was 0.784. Hence, the validity and reliability of the questionnaire were established.
Data collection
The data was collected one week after the poster competition. The students who were willing to participate in the survey were asked to provide their feedback using an online Google Forms survey. A google form link of the questionnaire was shared on a WhatsApp group, and the participants’ responses were collected. The option in Google Forms that prevents submission of partially replied or filled items made it impossible to submit an incomplete survey form. To give participants adequate time to complete the assignment, the survey was kept open for one week from the start date.
Data analysis
The participant’s location was entered into a Microsoft Excel sheet and turned into a (CSV) file. The geographic data were analyzed using Quantum Geographical Information System (QGIS), a free and open-source geographic information system version 3.12.3. The socio-demographic data and data on perceptions of the SDL process were downloaded and entered into a Microsoft Excel 2019 spreadsheet followed by analysis using SPSS version 26 (Statistical package for the social science) Windows, Version 26.0. (IBM Corp. Released 2019. IBM SPSS Statistics for Armonk, NY, USA). Descriptive statistical measures, such as percentage, mean and standard deviation, were applied. Data were presented as tables/graphs as relevant. The Chi-Square test/ Fisher's exact test was used to determine the association between demographic variables and the overall feedback of the students. A p-value of less than 0.05 was considered statistically significant.
Results
A total of 131 students took part in the study. The majority of the participants were females (61.4%). The mean age of the study participants was 19.45+ 0.87 years and 73 out of the 131 participants were aged less than 20 years. Around 62(47.33%) participants were from Karnataka, 19(14.50%) were from Kerela, 9 (6.87%) from Tamil Nadu and the rest from other states (Table-1).
Tools/Instruments
A pretested, semi-structured questionnaire was used to collect data from the participants. The questionnaire consisted of two parts. The first part of the questionnaire asked for sociodemographic details including, gender and address. The second section asked about the student’s perception of SDL, how it improved their learning and how much was this learning exercise beneficial to the participants (Likert scale, where 5=strongly agree,4= agree, 3=unsure, 2=disagree and 1=strongly disagree). A pilot study was conducted on 20 third-year students to assess the questionnaire’s accuracy and comprehension, who were later eliminated from the study. The Cronbach’s alpha score was 0.784. Hence, the validity and reliability of the questionnaire were established.
Data collection
The data was collected one week after the poster competition. The students who were willing to participate in the survey were asked to provide their feedback using an online Google Forms survey. A google form link of the questionnaire was shared on a WhatsApp group, and the participants’ responses were collected. The option in Google Forms that prevents submission of partially replied or filled items made it impossible to submit an incomplete survey form. To give participants adequate time to complete the assignment, the survey was kept open for one week from the start date.
Data analysis
The participant’s location was entered into a Microsoft Excel sheet and turned into a (CSV) file. The geographic data were analyzed using Quantum Geographical Information System (QGIS), a free and open-source geographic information system version 3.12.3. The socio-demographic data and data on perceptions of the SDL process were downloaded and entered into a Microsoft Excel 2019 spreadsheet followed by analysis using SPSS version 26 (Statistical package for the social science) Windows, Version 26.0. (IBM Corp. Released 2019. IBM SPSS Statistics for Armonk, NY, USA). Descriptive statistical measures, such as percentage, mean and standard deviation, were applied. Data were presented as tables/graphs as relevant. The Chi-Square test/ Fisher's exact test was used to determine the association between demographic variables and the overall feedback of the students. A p-value of less than 0.05 was considered statistically significant.
Results
A total of 131 students took part in the study. The majority of the participants were females (61.4%). The mean age of the study participants was 19.45+ 0.87 years and 73 out of the 131 participants were aged less than 20 years. Around 62(47.33%) participants were from Karnataka, 19(14.50%) were from Kerela, 9 (6.87%) from Tamil Nadu and the rest from other states (Table-1).
Table 1: Distribution of participants based on the demographic details
| Variables | Category | Frequency (%) |
Gender |
Male | 50 (38.2%) |
| Female | 81 (61.8%) | |
Age |
18 | 15 (11.5 %) |
| 19 | 58 (44.3 %) | |
| 20 | 44 (33.6 %) | |
| 21 | 14 (10.7 %) | |
State-wise distribution of participants |
Karnataka | 62(47.33%) |
| Kerala | 19(14.50%) | |
| Tamil Nadu | 9(6.87%) | |
| Uttar Pradesh | 8(6.11%) | |
| New Delhi | 8(6.11%) | |
| Haryana | 6(4.58%) | |
| Andhra Pradesh | 4(3.06%) | |
| Rajasthan | 4(3.06%) | |
| Jharkhand | 3(2.29%) | |
| Bihar | 3(2.29%) | |
| Punjab | 1(0.76%) | |
| Jammu Kashmir | 1(0.76%) | |
| Maharashtra | 1(0.76%) | |
| Punjab | 1(0.76%) | |
| Madhya Pradesh | 1(0.76%) |
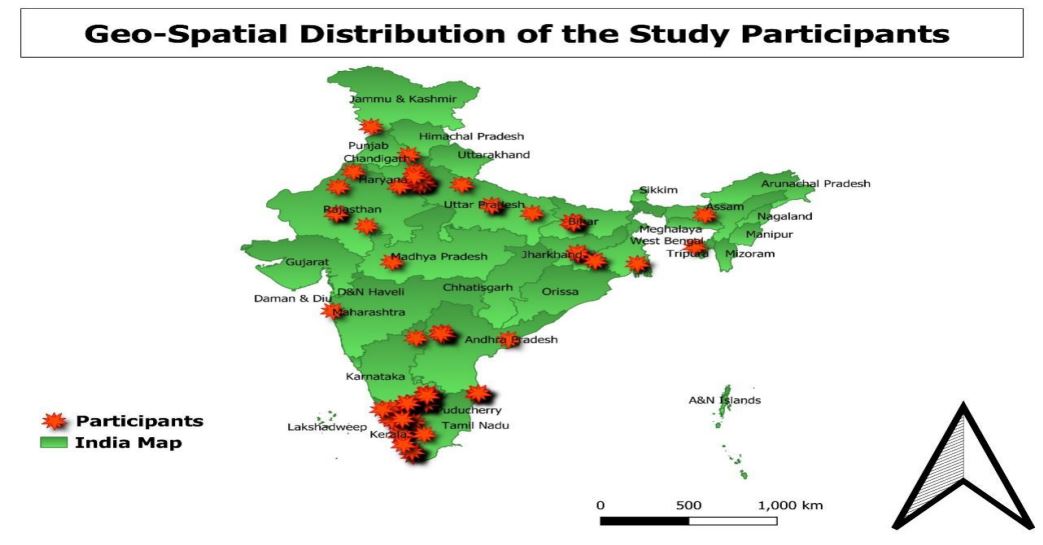
Figure 1: The geospatial distribution of the participants in the study
From the feedback obtained one week after the poster competition, around 125 (94.7%) participants stated SDL to be a very useful method of learning. Self-directed learning approaches, according to 97.7% of participants, allowed them to learn at their own pace, helped in better understanding of the topics and prepare for competitive exams. 52.67%, 56.48%, 75.57% and 47.33 % of the participants reported that self-directed learning methods helped them to assess readiness in learning, set learning goals, engage in the learning process and evaluate their learning, respectively (Figure 2).
Figure 2: Pie chart depicting the perception of students towards SDL methods and graph showing the positive impact of SDL among students
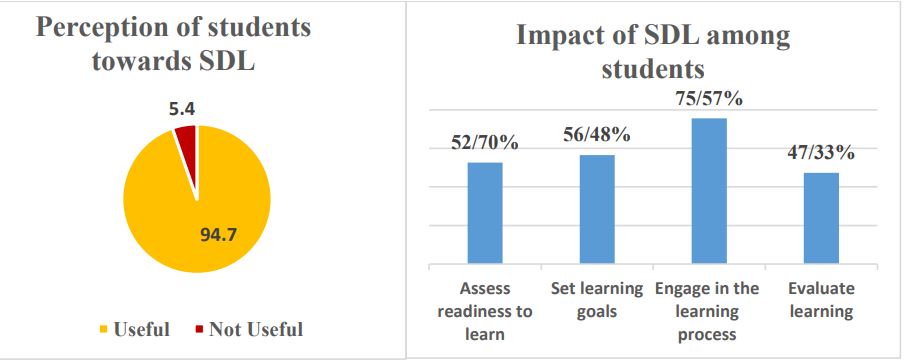
Figure 2: Pie chart depicting the perception of students towards SDL methods and graph showing the positive impact of SDL among students
The participants rated the self-directed learning exercise on a scale of 1–5 (1 being the lowest and 5 being the highest) with 59.54 % of participants strongly agreeing with the self-directed learning program and 3.06 % unsure about it. (Table 2,3)
Table 2: Feedback given by the participants based on different aspects of SDL
| Items | Strongly agree (%) | Agree (%) | Neutral (%) | Disagree (%) | Strongly disagree (%) |
| SDL should be implemented across all medical institutes | 78(59.54%) | 49(37.4%) | 4(3.06%) | 0 | 0 |
| SDL helped improve my team working skills | 75(57.26%) | 32(24.43%) | 22(16.79%) | 1(0.76%) | 1(0.76%) |
| SDL made my concepts clearer |
90(68.70%) | 29(22.14%) | 9(6.87%) | 3(2.29%) | 0 |
| SDL help in assessing different aspects of the topic | 53(40.46%) | 70(53.43%) | 5(3.82%) | 2(1.53%) | 1(0.76%) |
| SDL helped to analyze where I stood compared to my peers and gave me the scope for improvement | 44(33.59%) | 73(55.72%) | 14(10.69%) | 0 | 0 |
| SDL provided me with the opportunity to research the topic on my own and come up with creative ways to express what I learned through that research. | 65(49.62%) | 43(32.82%) | 20(15.27%) | 3(2.29%) | 0 |
| SDL makes us self-dependent and thinks in different ways | 83(63.37%) | 33(25.19%) | 13(9.92%) | 1(0.76%) | 1(0.76%) |
Table 3: Demographic profile and feedback of students regarding SDL
Charecteristics |
Feedback of students regarding overall SDL methods | Chi-square value | P-value | |||
| Strongly agree [n=78] (%) |
Agree [n=43] (%) |
Neutral [n=4] (%) | ||||
Gender |
Male | 22(44%) | 24(48%) | 4(8%) | 11.628 | 0.001* |
| Female | 56(69.1%) | 25(30.9%) | 0(0%) | |||
Age |
18 | 10(66.7%) | 5(33.3%) | 0(0%) | 2.814 | 0.626 |
| 19 | 33(56.9%) | 24(41.4%) | 1(1.7%) | |||
| 20 | 26(59.1%) | 15(34.1%) | 3(6.8%) | |||
| 21 | 9(64.3%) | 5(35.7%) | 0(1%) | |||
| SDL methods | Useful | 78(62.4%) | 43(34.4%) | 4(3.2%) | 10.030 | 0.014* |
| Not useful | 0(0%) | 6(100%) | 0(0%) | |||
p<0.05- statistical significance, * - Fisher’s Exact Test
Discussion
Medical students must develop a variety of learning qualities, including confidence, autonomy, motivation, and lifetime learning readiness. SDL is one of the abilities that medical students need to be lifelong learners, especially in a PBL-based medical curriculum. In a preclinical curriculum that is predominantly lecture-based, course activities must be purposefully planned to improve SDL skills. The purpose of the poster competition was to allow students to develop and practice skills that are needed for lifelong learning (11).
In the present study, 94.7% of the study participants responded that the SDL methods helped them in learning. This was found to be higher when compared to another study done by Sonia Gon et al. in 2017 where second-year medical students were divided into two groups and were taught the same topics by two different methods, i.e. through WhatsApp and via didactic lectures. 70% of students there reported self-directed learning to be useful while some of its disadvantages reported were message flooding, time consumption and eye strain (12).
In our study, SDL was found to be a very effective approach to learning first-year medical education. SDL has previously been proven to be a successful approach for boosting learners and creating a better understanding of the subject. Furthermore, earlier research also showed self-learning to be effective in enhancing knowledge about clinical medical management and a self-directed learning curriculum helped in improving the quality care of patients (13,14).
Motivation and self-identity are essential for self-directed learners. They will undervalue their work if it is not recognized by an external authority, thus the facilitator must encourage and reassure them to achieve greater results (15). The problem case in PBL motivates students to engage in independent self-directed learning. Students who learned utilizing a PBL approach expressed how the character of self-directed learning developed in them in one study. PBL engages students by motivating them to create their own learning goals and allowing them to participate in decisions that affect their learning (15,16).
In our study, 97.7% of the students felt self-directed learning methods helped them learn at their own pace and manage their learning. Similar results were obtained in a study done by Soumendra Sahoo in 2016 where the majority of the students reported SDL as a driving force for lifelong learning. The majority of students said that weekly SDL topic assessments were less stressful and had helped them to better utilize the SDL hours allocated in the teaching plan (17).
It has been said that students who were prepared for SDL can manage their own learning throughout their careers, and our study supports this claim.(18) The majority of students believed that the weekly evaluations of SDL topics were not burdensome but rather aided them in making the best use of the SDL time allotted to the lesson plan. According to one study, SDL levels were not necessarily related to learning activities or academic performance, especially when they were coupled with high levels of instructor control (19). In our study, instructor’s involvement was minimal.
According to the participants, SDL sessions were found to be an effective, entertaining, and straightforward approach in promoting active learning among students, hence by improving knowledge of a given subject. As the students were solely responsible for determining the solutions to the learning objectives assigned to them, they were pushed to think, conduct research, engage in group debate, and conclude. The learners were more impressed by this than by passive listening in didactic lectures (18). This also helps to strengthen long-term memory and boost memory recall. Students were almost forced to browse through the books, read the themes attentively, pick up the answers, and summarise, which they would not have done otherwise after a didactic session. These types of learner-centered instructional tools provide us with the ability to change our curriculum and produce a slew of new medical education innovations (9,20).
Limitations
Our study’s limitations include small sample size and not correlating students’ academic performance during undergraduate training. Further, the quality of the posters was not assessed in the study nor it was compared with the previous year’s results. Because the current study was based on a self-reported questionnaire that probed student perspectives, it is not a direct measure of their SDL preparation. This study was conducted at only one institution and only in one batch of first-year medical students, which means it may not apply to other courses or settings.
Conclusion
The present study revealed that the overall SDL readiness of participants was good. The students displayed a strong willingness to learn independently, and the SDL helped them in learning the subject thoroughly at their own pace. Self-directed learning is a method of knowledge acquisition that is distinct from traditional learning. It is not necessary to combine it with other educational styles. However, SDL can be improved further by re-examining the current teaching and learning practices. Faculty development programs are essential for the successful implementation of such changes. A longer-term study with a wide-ranging content area is necessary to establish the influence of SDL on standard curricula.
Ethical considerations
The study was approved by the Institutional Ethics Committee (JSSMC/IEC/240123/13NCT/2022-23 )
Acknowledgments
We, the authors, would like to thank the study participants for their cooperation. We also thank the Department of Community Medicine at JSS Medical College Mysuru for permitting us to conduct the study.
Funding
No funding sources
Conflict of interest
None declared
Author contributions
Dr. Sunil Kumar D and Dr. Deepak Anil designed and conducted the study, collected and analyzed the data, and drafted the manuscript. Dr M R Narayana Murthy participated in analysis and interpretation, read and approved the final manuscript: All authors approved the final draft.
In the present study, 94.7% of the study participants responded that the SDL methods helped them in learning. This was found to be higher when compared to another study done by Sonia Gon et al. in 2017 where second-year medical students were divided into two groups and were taught the same topics by two different methods, i.e. through WhatsApp and via didactic lectures. 70% of students there reported self-directed learning to be useful while some of its disadvantages reported were message flooding, time consumption and eye strain (12).
In our study, SDL was found to be a very effective approach to learning first-year medical education. SDL has previously been proven to be a successful approach for boosting learners and creating a better understanding of the subject. Furthermore, earlier research also showed self-learning to be effective in enhancing knowledge about clinical medical management and a self-directed learning curriculum helped in improving the quality care of patients (13,14).
Motivation and self-identity are essential for self-directed learners. They will undervalue their work if it is not recognized by an external authority, thus the facilitator must encourage and reassure them to achieve greater results (15). The problem case in PBL motivates students to engage in independent self-directed learning. Students who learned utilizing a PBL approach expressed how the character of self-directed learning developed in them in one study. PBL engages students by motivating them to create their own learning goals and allowing them to participate in decisions that affect their learning (15,16).
In our study, 97.7% of the students felt self-directed learning methods helped them learn at their own pace and manage their learning. Similar results were obtained in a study done by Soumendra Sahoo in 2016 where the majority of the students reported SDL as a driving force for lifelong learning. The majority of students said that weekly SDL topic assessments were less stressful and had helped them to better utilize the SDL hours allocated in the teaching plan (17).
It has been said that students who were prepared for SDL can manage their own learning throughout their careers, and our study supports this claim.(18) The majority of students believed that the weekly evaluations of SDL topics were not burdensome but rather aided them in making the best use of the SDL time allotted to the lesson plan. According to one study, SDL levels were not necessarily related to learning activities or academic performance, especially when they were coupled with high levels of instructor control (19). In our study, instructor’s involvement was minimal.
According to the participants, SDL sessions were found to be an effective, entertaining, and straightforward approach in promoting active learning among students, hence by improving knowledge of a given subject. As the students were solely responsible for determining the solutions to the learning objectives assigned to them, they were pushed to think, conduct research, engage in group debate, and conclude. The learners were more impressed by this than by passive listening in didactic lectures (18). This also helps to strengthen long-term memory and boost memory recall. Students were almost forced to browse through the books, read the themes attentively, pick up the answers, and summarise, which they would not have done otherwise after a didactic session. These types of learner-centered instructional tools provide us with the ability to change our curriculum and produce a slew of new medical education innovations (9,20).
Limitations
Our study’s limitations include small sample size and not correlating students’ academic performance during undergraduate training. Further, the quality of the posters was not assessed in the study nor it was compared with the previous year’s results. Because the current study was based on a self-reported questionnaire that probed student perspectives, it is not a direct measure of their SDL preparation. This study was conducted at only one institution and only in one batch of first-year medical students, which means it may not apply to other courses or settings.
Conclusion
The present study revealed that the overall SDL readiness of participants was good. The students displayed a strong willingness to learn independently, and the SDL helped them in learning the subject thoroughly at their own pace. Self-directed learning is a method of knowledge acquisition that is distinct from traditional learning. It is not necessary to combine it with other educational styles. However, SDL can be improved further by re-examining the current teaching and learning practices. Faculty development programs are essential for the successful implementation of such changes. A longer-term study with a wide-ranging content area is necessary to establish the influence of SDL on standard curricula.
Ethical considerations
The study was approved by the Institutional Ethics Committee (JSSMC/IEC/240123/13NCT/2022-23 )
Acknowledgments
We, the authors, would like to thank the study participants for their cooperation. We also thank the Department of Community Medicine at JSS Medical College Mysuru for permitting us to conduct the study.
Funding
No funding sources
Conflict of interest
None declared
Author contributions
Dr. Sunil Kumar D and Dr. Deepak Anil designed and conducted the study, collected and analyzed the data, and drafted the manuscript. Dr M R Narayana Murthy participated in analysis and interpretation, read and approved the final manuscript: All authors approved the final draft.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2022/11/28 | Accepted: 2023/02/20 | Published: 2023/05/17
Received: 2022/11/28 | Accepted: 2023/02/20 | Published: 2023/05/17
References
1. Premkumar K, Vinod E, Sathishkumar S, Pulimood AB, Umaefulam V, Samuel PP, John TA. Self-directed learning readiness of Indian medical students: a mixed method study. BMC medical education. 2018;18(1):1-0. [DOI]
2. Hill M, Peters M, Salvaggio M, Vinnedge J, Darden A. Implementation and evaluation of a self-directed learning activity for first-year medical students. Medical education online. 2020 1;25(1):1717780. [DOI]
3. Soliman M, Al-Shaikh G. Readiness for self-directed learning among first year Saudi medical students: A descriptive study. Pakistan Journal of Medical Sciences. 2015;31(4):799. [DOI]
4. Knowles MS. Innovations in teaching styles and approaches based upon adult learning. Journal of education for social work. 1972 1;8(2):32-9. [DOI]
5. Towle A, Cottrell D. Self directed learning. Archives of disease in childhood. 1996 Apr 1;74(4):357-9. [DOI]
6. Frambach JM, Driessen EW, Chan LC, van der Vleuten CP. Rethinking the globalisation of problem‐based learning: how culture challenges self‐directed learning. Medical education. 2012;46(8):738-47. [DOI]
7. Pai KM, Rao KR, Punja D, Kamath A. The effectiveness of self-directed learning (SDL) for teaching physiology to first-year medical students. The Australasian medical journal. 2014;7(11):448. [PubMed]
8. List of College Teaching MBBS | NMC [Internet]. [cited 2021 Nov 19]. Available from: [Article]
9. Kar SS, Premarajan KC, Ramalingam A, Iswarya S, Sujiv A, Subitha L. Self-directed learning readiness among fifth semester MBBS students in a teaching institution of South India. Education for Health. 2014;27(3):289. [DOI]
10. Jagadguru Sri Shivarathreeshwara University [Internet]. [cited 2021 Dec 2]. Available from: [Article]
11. Keator CS, Vandre DD, Morris AM. The challenges of developing a project-based self-directed learning component for undergraduate medical education. Medical Science Educator. 2016;26(4):801-5. [DOI]
12. Gon S, Rawekar A. Effectivity of e-learning through WhatsApp as a teaching learning tool. MVP Journal of Medical Sciences. 2017;4(1):19-25. [DOI]
13. Holmboe ES, Prince L, Green M. Teaching and improving quality of care in a primary care internal medicine residency clinic. Academic Medicine. 2005;80(6):571-7. [DOI]
14. Anderson SM, Helberg SB. Chart-based, case-based learning. South Dakota medicine: the journal of the South Dakota State Medical Association. 2007;60(10):391-3. [PubMed]
15. Shokar GS, Shokar NK, Romero CM, Bulik RJ. Self-directed learning: looking at outcomes with medical students. Family Medicine-Kansas City-. 2002;34(3):197-200. [PubMed]
16. Williams B. Self direction in a problem based learning program. Nurse Education Today. 2004;24(4):277-85. [DOI]
17. Sahoo S. Finding self-directed learning readiness and fostering self-directed learning through weekly assessment of self-directed learning topics during undergraduate clinical training in ophthalmology. International Journal of Applied and Basic Medical Research. 2016;6(3):166. [DOI]
18. Greveson GC, Spencer JA. Self-directed learning – The importance of concepts and contexts. Medical Education. 2005;39:348–9. [DOI]
19. McCune SK. Texas A & M University; 1988. A meta-analytic study of adult self-direction in learning: A review of the research from 1977 to 1987 [Dissertation]
20. Devi S, Bhat KS, Ramya SR, Ravichandran K, Kanungo R. Self-directed learning to enhance active learning among the 2nd-year undergraduate medical students in Microbiology: An experimental study. Journal of Current Research in Scientific Medicine. 2016;2(2):80. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |