Fri, Jan 30, 2026
[Archive]
Volume 18, Issue 3 (2025)
J Med Edu Dev 2025, 18(3): 26-34 |
Back to browse issues page
Ethics code: IR.ABZUMS.REC.1403.219
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahmatpour P, Eskanadari Z, Esmaeili Abdar M, Norouzinia R. The effects of drill-based triage education on the retention of applied knowledge, confidence, and satisfaction of Iranian nursing students. J Med Edu Dev 2025; 18 (3) :26-34
URL: http://edujournal.zums.ac.ir/article-1-2484-en.html
URL: http://edujournal.zums.ac.ir/article-1-2484-en.html
1- Health Sciences Research Unit: Nursing [UICISA: E], Nursing School of Coimbra [ESEnfC], Coimbra, Portugal.
2- Department of Pre-hospital Medical Emergencies, School of Nursing, Alborz University of Medical Sciences, Karaj, Iran
3- School of Nursing, Kashan University of Medical Sciences, Kashan, Iran & Department of Pre-hospital Medical Emergencies, School of Nursing, Alborz University of Medical Sciences, Karaj, Iran
4- Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran ,norouzinia.r@gmail.com
2- Department of Pre-hospital Medical Emergencies, School of Nursing, Alborz University of Medical Sciences, Karaj, Iran
3- School of Nursing, Kashan University of Medical Sciences, Kashan, Iran & Department of Pre-hospital Medical Emergencies, School of Nursing, Alborz University of Medical Sciences, Karaj, Iran
4- Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran ,
Full-Text [PDF 472 kb]
(398 Downloads)
| Abstract (HTML) (943 Views)
Full-Text: (28 Views)
Abstract
Background & Objective: Mass casualty incidents (MCIs) require rapid and accurate triage. Drill-based training may help nursing students get ready for MCIs. In this quasi-experimental study, we checked how well drill-based triage education works in improving applied knowledge, confidence, and satisfaction among Iranian nursing undergraduates.
Materials & Methods: In this quasi-experimental study, 30 sixth-semester nursing students enrolled in the course “Risk Management in Disasters and Emergencies” were selected using convenience sampling and randomized (1:1) into two groups: a control group, which received a lecture, case discussion, and video presentation, and an intervention group, which participated in the same training supplemented by a practical drill exercise. Both received 2 hours of didactic instruction on START and Jump-START protocols, video showing, and case discussion. One week later, the intervention group did a 2-hour high-fidelity MCI simulation with standardized patients. Pre- and one-month post-tests checked applied knowledge, self-rated confidence, and satisfaction. Data were analyses by ANCOVA, controlling for baseline scores using SPSS version 20.
Results: The average age of students was 22.43 ± 1.36 years, and 63.3% of them were female. Both groups showed significant gains in applied knowledge (control: 5.00 ± 1.77→12.47 ± 0.83, p < .001; intervention: 5.27 ± 1.16→12.53 ± 0.64, p < .001), but only the simulation group showed a significant confidence increase (1.93 ± 0.59→3.13 ± 0.74, p < .001). Satisfaction was high, but there was no significant difference between groups (control: 18.87 ± 4.01 vs. intervention: 19.33 ± 2.72; p = .712), and post-test between-group differences reached significance only for confidence (p < .001).
Conclusion: Drill-based triage training may help student confidence, though it showed no significant advantage over traditional methods in applied knowledge or satisfaction. A blended instructional approach appears equally effective. Further studies with larger samples are needed to confirm these findings.
Introduction
Mass Casualty Incidents (MCIs) place huge pressure on healthcare systems by causing many injuries at the same time in settings with limited resources and urgent time demands—often during natural disasters or human-made threats [1, 2]. Triage (the quick sorting of patients based on how serious their injuries are) helps make sure those who need care the most get it quickly [3]. The Simple Triage and Rapid Treatment (START) method, made for adults, guides responders to set a priority level within 60 seconds by checking breathing rate, blood flow, and mental state [4, 5]. Its version for children, Jump-START, takes into account their unique body systems and limits in understanding and following instructions [6]. As emergencies become more complex, full triage training becomes essential for nursing professionals who must make fast, life-saving choices [7].
Nursing students have basic knowledge and skills that can strengthen disaster response ability, making them an underused resource in MCIs [8, 9]. In fact, many students say they are willing to take on important roles; such as triage, treatment, clinical care, and rescue—during mass-casualty events [10].
In Iran, although the Emergency Medical Service Organization requires yearly triage training for nursing staff [11], reviews show ongoing problems in both triage knowledge and decision-making, which can lead to patients being sorted incorrectly and bad results [12–14]. Soola et al. reported that participants without organized triage education had big gaps in decision-making skills, leading to a recommendation for continued professional learning and focused training to improve triage accuracy and patient results [15]. Similarly, a Turkish study found that, although many prehospital emergency workers showed a medium level of knowledge about START, they still felt unready to use the method well in real situations [3].
Modern teaching methods stress that triage training must go beyond just memorizing steps to build situational awareness and critical thinking under stress [16]. As a result, the use of mass-casualty drills and realistic simulations—with different situations designed to copy chaotic environments—has become more popular as an active learning approach to improve decision-making in high-pressure settings [17].
Real-world evidence supports the effectiveness of simulation-based training: it greatly improves nursing students’ self-confidence and clinical triage skills, helping them get more ready for real emergencies [18], and deepens their understanding of disaster management when combined with classroom learning [4, 7]. However, traditional lectures and hands-on workshops, while good at boosting short-term learning, often do not keep knowledge over time [11]. Triage training more broadly has been shown to raise both knowledge and confidence among healthcare providers [19]. A “practice-first” trauma model by Awwad and Alqaissi (2025) led to big gains in triage skill for emergency nurses, mostly kept after three months but with a small drop—leading to a suggestion for training every two years [20]. Other studies show that realistic simulations increase confidence, understanding of theory, and real-world performance across different groups of learners [21], and that role-playing works better than lectures for improving hands-on triage skills in undergraduates [18]. Also, programs using trained actors in realistic disaster scenes clearly improve nursing students’ speed in making decisions, ability to talk with others, and teamwork skills [22, 23].
Despite strong international evidence, no Iranian study has directly compared drill-based triage education with improved classroom teaching for undergraduate nursing students. To fill this gap, the present quasi-experimental study looks at the added effects of a single, realistic drill session—added to standard lectures, videos, and case discussions—on nursing students’ practical triage knowledge, self-confidence, and satisfaction.
Materials & Methods
Design and setting(s)
This study used a two-group pretest-posttest quasi-experimental design to check the effects of a training program held between September 13, 2024, and January 4, 2025, at Alborz University of Medical Sciences.
Participants and sampling
The study group included nursing students enrolled in the "Risk Management in Disasters and Emergencies" course through convenience sampling. To be included, students had to be in their second semester or higher, have chosen the course, and be willing to take part in the study. Students were excluded if they missed class or simulation sessions or did not take the pre-test or post-test.
The class had 35 sixth-semester undergraduate nursing students, five of whom decided not to join the study and attended only the class session. The remaining 30 students were chosen and randomly split into two groups of 15 each. To assign students to the two groups, their student ID numbers were sorted from lowest to highest and then given alternately to the intervention and control groups.
Since this course is only offered in the sixth semester and only one group of nursing students takes it each academic term, the study had a small sample size. Because the main goal was to study how practical training affects keeping applied knowledge, confidence, and satisfaction, student interaction was not seen as a factor that could affect the results.
Tools/Instruments
Demographic: Asked for students’ age, sex, and GPA. Triage applied knowledge: A multiple-choice test, made up of 14 victim case stories from a mass casualty incident, was created by faculty members of the Health in Emergencies and Disasters Department based on standard textbooks and matched to the course goals. Each question showed the condition of a bus accident victim at different triage levels.
So, the test checked not only students' knowledge of the triage steps but also their judgment and decision-making skills.
However, since their performance was not tested in a real, high-pressure incident situation, the term "applied knowledge" was used to describe their shown skills. The test was reviewed by a panel of five experts to make sure of content and face validity. Since there is only one right answer in knowledge tests, the correct answer was given a score of 1, and the three wrong choices were scored 0. As a result, the Kuder–Richardson 20 method was used to calculate reliability. Reliability was confirmed by a calculated Kuder–Richardson 20 value of 0.72.
Confidence: Students' confidence was checked through a 5-point question asking them to choose their confidence level in helping with or leading a response to a mass casualty incident (MCI): no: “I would avoid the situation entirely.” (score = 0); unsure: “I would need guidance on what steps to take.” (score = 1); maybe: “I could help with some direction.” (score = 2); yes: “I usually know how to handle most situations.” (score = 3); definitely: “I can manage any situation with confidence.” (score = 4). This question was used in the study by Yu & Coffey [19].
Satisfaction: To check student satisfaction with the lecture-only and video demonstration parts and the drill exercise, students answered 5 questions with responses from very low (1) to very high (5) (questions included: How satisfied are you with your overall experience in this educational course?
In your opinion, how much did taking part in this educational course affect the depth of your learning?
How satisfied were you with the teaching and help methods in this educational course? How interesting was this educational course to you? To what extent did this class help you better understand how to use triage in real-life situations?) Content validity was confirmed by a panel of 10 faculty members from medical education, nursing, and emergency medicine. Reliability was shown using Cronbach’s alpha, which was calculated at 0.876 for the control group and 0.706 for the intervention group.
Data collection methods
Figure 1 shows the study flow. Before any instruction, all participants completed a pre-test made up of demographic questions and checked applied-knowledge and confidence questionnaires.
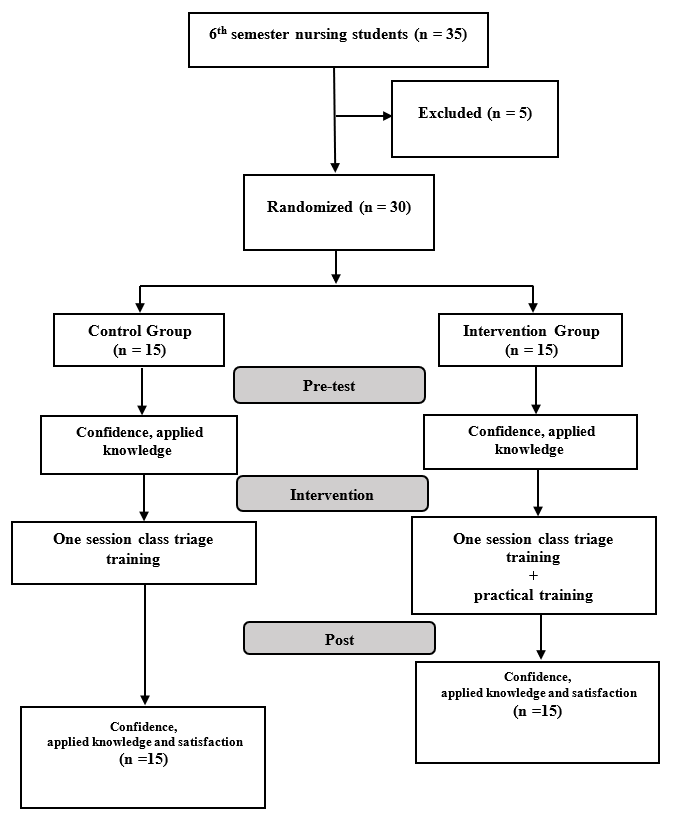
Figure 1. Flowchart of study procedure
Didactic training: A single 2-hour classroom session of the “Risk Management in Disasters and Emergencies” course covered START and Jump-START triage. The session was given by a Ph.D. faculty member from the Department of Emergency Medical Services with lots of triage-training experience.
Instruction methods included a lecture on triage theory and steps, case discussion of mass-casualty situations, a video showing a made-up bus accident triage, and guided group discussion with instructor-led feedback on student decisions.
Drill intervention: One week later, only the intervention group (n = 15) took part in an individual high-fidelity simulation—Drill— (20 minutes per student), copying a chaotic mass-casualty setting. “A drill is a coordinated, supervised exercise activity, usually used to test a single specific operation or function” [24].
To avoid interaction between control and intervention groups, ten trained undergraduate emergency-medical students acted as standardized patients, made up to show realistic wounds.
Then, each student entered the scene alone, triaged victims within the usual 30–60 seconds per patient, was watched by an evaluator who filled out a standardized checklist, and went to an isolation area after finishing the task.
A structured debrief came after each participant’s run, during which the evaluator gave feedback on decision-making and error correction. Snack packs were offered as a token of appreciation.
One month after the simulation, all 30 students repeated theapplied-knowledge, confidence, and satisfaction questionnaires.
Although control-group students were invited to join the simulation exercise, none could attend because of scheduling conflicts with their lectures and clinical internships.
Table 3. Score changes of triage applied knowledge and confidence of intervention and control groups
Note: ANCOVA test was used to compare post-test scores between the intervention and control groups.
Abbreviations: SD, standard deviation; F, analysis of variance test statistic; p, probability-value; η², eta squared (effect size).
Discussion
This study looked at how effective drill-based START and Jump-START triage training—combined with hands-on practice—was in improving applied knowledge, confidence, and satisfaction among nursing students during MCIs.
Our results show that a single didactic session combining lectures, case discussion, and video demonstrations led to clear knowledge retention at one month, with no extra benefit from the drill exercise. In contrast, Delnavaz et al. found role-playing better than lecture-only methods for triage education [18]. The difference between our study and theirs is that we used lecture and practice for the intervention group, creating a stronger intervention with several active learning methods. Similarly, Andreatta et al. reported equal START-algorithm performance between Virtual-Reality (VR)
and standardized-patient groups, concluding that VR offers a practical, repeatable alternative for disaster-triage training [25]. Along with our findings, these data suggest that any teaching method that fully covers learning goals—whether standardized patients vs. VR or classroom plus case/video vs. hands-on simulation—can produce similar knowledge gains.
Supporting this, Pouraghaei et al. noticed important improvements in prehospital personnel knowledge and performance after START training [26], and Aslan et al. recorded clear triage knowledge increases among nursing students following first-aid instruction [27]. These show that structured triage programs reliably raise cognitive outcomes.
By contrast, only the drill group in our study yielded an important boost in self-reported confidence, both within-group and versus controls. Immersion in a high-stress, chaotic MCI scenario—coupled with immediate, performance-focused feedback—likely accounts for this effect, reflecting reports that simulation helps clinicians’ self-efficacy in acute scenarios [28-30]. Lima et al. similarly found that simulated MCI drills foster teamwork, clinical reasoning, and confidence in both helping and leading disaster responses [31], and Alshammari showed confidence gains after role-play exercises [32]. Other triage-drill studies confirm these confidence improvements among nursing students and prehospital providers [33, 34].
Although intervention-group satisfaction trended higher, the difference did not reach importance, perhaps because our control condition was itself engaging, or because the intense realism of the drill was less “enjoyable” than more gamified role-play formats reported by Khan et al. and Ahmady et al. to increase learner satisfaction [35, 36]. Equally skilled instruction across both groups may also have equalized learners’ overall experience.
This study’s limitations include its small, single-site sample (N=30), a one-month follow-up preventing long-term retention analysis, and reliance on self-reported confidence and satisfaction measures. In addition, we used one question to check the confidence of students; thus, it is recommended to use a valid and reliable scale to measure this concept. Future multicenter trials with larger cohorts, extended follow-up, objective performance metrics, and qualitative feedback will help confirm and extend these findings.
Conclusion
The study’s findings must be interpreted with caution given its small sample size. Drill‐based triage exercises significantly improved student confidence—likely reflecting the immersive, context‐rich environment they provide—whereas both drill and classroom‐based instruction produced comparable gains in applied knowledge, with no significant differences between methods. Satisfaction scores likewise did not differ significantly. These results suggest that, for objectives centered on applied‐knowledge acquisition or learner satisfaction, a blended approach of lectures, case discussion, and video shows may be as effective as full‐scale drill. Nonetheless, larger studies are needed to confirm these conclusions and to determine which specific educational outcomes get the greatest benefit from drill‐based learning. Nonetheless, further research with larger sample sizes is warranted to confirm these findings and to more precisely identify which educational outcomes benefit most from drill-based learning.
Ethical considerations
This study was approved under the ethical committee of Alborz University of Medical Sciences (IR.ABZUMS.REC.1403.219). Informed consent was gotten from all participants, including the group of undergraduate emergency medical students who acted as simulated patients in the study, as well as all nursing students prior to their involvement in the research. They were provided with detailed information about the study's purpose and the drill procedures and were assured of their right to withdraw at any time without consequences. Participation was entirely voluntary. All collected data were kept confidential and securely stored. Participants’ identities were anonymized, and any identifying information was removed to protect their privacy. At the end of the study, participants were told about the educational intervention, and any questions or concerns were answered. The present study was performed under the international ethical standards of the Declaration of Helsinki.
Artificial intelligence utilization for article writing
English language editing of this manuscript was helped by Grammarly, an AI-based writing tool. No AI tools were used for content generation, data analysis, or interpretation.
Acknowledgment
The authors would like to extend their gratitude to the Research and Technology Deputy of Alborz University of Medical Sciences for their invaluable support. Furthermore, we appreciate the students who helped with this project.
Conflict of interest statement
No conflict of interest has been declared by the authors.
Author contributions
RN and ZE were involved in the creation and organization of the study. ZE and MEA were involved in carrying out the drill and data collection. RN and PR took part in statistical analysis design. RN prepared the first draft of the manuscript. All authors contributed to the critical review and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Background & Objective: Mass casualty incidents (MCIs) require rapid and accurate triage. Drill-based training may help nursing students get ready for MCIs. In this quasi-experimental study, we checked how well drill-based triage education works in improving applied knowledge, confidence, and satisfaction among Iranian nursing undergraduates.
Materials & Methods: In this quasi-experimental study, 30 sixth-semester nursing students enrolled in the course “Risk Management in Disasters and Emergencies” were selected using convenience sampling and randomized (1:1) into two groups: a control group, which received a lecture, case discussion, and video presentation, and an intervention group, which participated in the same training supplemented by a practical drill exercise. Both received 2 hours of didactic instruction on START and Jump-START protocols, video showing, and case discussion. One week later, the intervention group did a 2-hour high-fidelity MCI simulation with standardized patients. Pre- and one-month post-tests checked applied knowledge, self-rated confidence, and satisfaction. Data were analyses by ANCOVA, controlling for baseline scores using SPSS version 20.
Results: The average age of students was 22.43 ± 1.36 years, and 63.3% of them were female. Both groups showed significant gains in applied knowledge (control: 5.00 ± 1.77→12.47 ± 0.83, p < .001; intervention: 5.27 ± 1.16→12.53 ± 0.64, p < .001), but only the simulation group showed a significant confidence increase (1.93 ± 0.59→3.13 ± 0.74, p < .001). Satisfaction was high, but there was no significant difference between groups (control: 18.87 ± 4.01 vs. intervention: 19.33 ± 2.72; p = .712), and post-test between-group differences reached significance only for confidence (p < .001).
Conclusion: Drill-based triage training may help student confidence, though it showed no significant advantage over traditional methods in applied knowledge or satisfaction. A blended instructional approach appears equally effective. Further studies with larger samples are needed to confirm these findings.
Introduction
Mass Casualty Incidents (MCIs) place huge pressure on healthcare systems by causing many injuries at the same time in settings with limited resources and urgent time demands—often during natural disasters or human-made threats [1, 2]. Triage (the quick sorting of patients based on how serious their injuries are) helps make sure those who need care the most get it quickly [3]. The Simple Triage and Rapid Treatment (START) method, made for adults, guides responders to set a priority level within 60 seconds by checking breathing rate, blood flow, and mental state [4, 5]. Its version for children, Jump-START, takes into account their unique body systems and limits in understanding and following instructions [6]. As emergencies become more complex, full triage training becomes essential for nursing professionals who must make fast, life-saving choices [7].
Nursing students have basic knowledge and skills that can strengthen disaster response ability, making them an underused resource in MCIs [8, 9]. In fact, many students say they are willing to take on important roles; such as triage, treatment, clinical care, and rescue—during mass-casualty events [10].
In Iran, although the Emergency Medical Service Organization requires yearly triage training for nursing staff [11], reviews show ongoing problems in both triage knowledge and decision-making, which can lead to patients being sorted incorrectly and bad results [12–14]. Soola et al. reported that participants without organized triage education had big gaps in decision-making skills, leading to a recommendation for continued professional learning and focused training to improve triage accuracy and patient results [15]. Similarly, a Turkish study found that, although many prehospital emergency workers showed a medium level of knowledge about START, they still felt unready to use the method well in real situations [3].
Modern teaching methods stress that triage training must go beyond just memorizing steps to build situational awareness and critical thinking under stress [16]. As a result, the use of mass-casualty drills and realistic simulations—with different situations designed to copy chaotic environments—has become more popular as an active learning approach to improve decision-making in high-pressure settings [17].
Real-world evidence supports the effectiveness of simulation-based training: it greatly improves nursing students’ self-confidence and clinical triage skills, helping them get more ready for real emergencies [18], and deepens their understanding of disaster management when combined with classroom learning [4, 7]. However, traditional lectures and hands-on workshops, while good at boosting short-term learning, often do not keep knowledge over time [11]. Triage training more broadly has been shown to raise both knowledge and confidence among healthcare providers [19]. A “practice-first” trauma model by Awwad and Alqaissi (2025) led to big gains in triage skill for emergency nurses, mostly kept after three months but with a small drop—leading to a suggestion for training every two years [20]. Other studies show that realistic simulations increase confidence, understanding of theory, and real-world performance across different groups of learners [21], and that role-playing works better than lectures for improving hands-on triage skills in undergraduates [18]. Also, programs using trained actors in realistic disaster scenes clearly improve nursing students’ speed in making decisions, ability to talk with others, and teamwork skills [22, 23].
Despite strong international evidence, no Iranian study has directly compared drill-based triage education with improved classroom teaching for undergraduate nursing students. To fill this gap, the present quasi-experimental study looks at the added effects of a single, realistic drill session—added to standard lectures, videos, and case discussions—on nursing students’ practical triage knowledge, self-confidence, and satisfaction.
Materials & Methods
Design and setting(s)
This study used a two-group pretest-posttest quasi-experimental design to check the effects of a training program held between September 13, 2024, and January 4, 2025, at Alborz University of Medical Sciences.
Participants and sampling
The study group included nursing students enrolled in the "Risk Management in Disasters and Emergencies" course through convenience sampling. To be included, students had to be in their second semester or higher, have chosen the course, and be willing to take part in the study. Students were excluded if they missed class or simulation sessions or did not take the pre-test or post-test.
The class had 35 sixth-semester undergraduate nursing students, five of whom decided not to join the study and attended only the class session. The remaining 30 students were chosen and randomly split into two groups of 15 each. To assign students to the two groups, their student ID numbers were sorted from lowest to highest and then given alternately to the intervention and control groups.
Since this course is only offered in the sixth semester and only one group of nursing students takes it each academic term, the study had a small sample size. Because the main goal was to study how practical training affects keeping applied knowledge, confidence, and satisfaction, student interaction was not seen as a factor that could affect the results.
Tools/Instruments
Demographic: Asked for students’ age, sex, and GPA. Triage applied knowledge: A multiple-choice test, made up of 14 victim case stories from a mass casualty incident, was created by faculty members of the Health in Emergencies and Disasters Department based on standard textbooks and matched to the course goals. Each question showed the condition of a bus accident victim at different triage levels.
So, the test checked not only students' knowledge of the triage steps but also their judgment and decision-making skills.
However, since their performance was not tested in a real, high-pressure incident situation, the term "applied knowledge" was used to describe their shown skills. The test was reviewed by a panel of five experts to make sure of content and face validity. Since there is only one right answer in knowledge tests, the correct answer was given a score of 1, and the three wrong choices were scored 0. As a result, the Kuder–Richardson 20 method was used to calculate reliability. Reliability was confirmed by a calculated Kuder–Richardson 20 value of 0.72.
Confidence: Students' confidence was checked through a 5-point question asking them to choose their confidence level in helping with or leading a response to a mass casualty incident (MCI): no: “I would avoid the situation entirely.” (score = 0); unsure: “I would need guidance on what steps to take.” (score = 1); maybe: “I could help with some direction.” (score = 2); yes: “I usually know how to handle most situations.” (score = 3); definitely: “I can manage any situation with confidence.” (score = 4). This question was used in the study by Yu & Coffey [19].
Satisfaction: To check student satisfaction with the lecture-only and video demonstration parts and the drill exercise, students answered 5 questions with responses from very low (1) to very high (5) (questions included: How satisfied are you with your overall experience in this educational course?
In your opinion, how much did taking part in this educational course affect the depth of your learning?
How satisfied were you with the teaching and help methods in this educational course? How interesting was this educational course to you? To what extent did this class help you better understand how to use triage in real-life situations?) Content validity was confirmed by a panel of 10 faculty members from medical education, nursing, and emergency medicine. Reliability was shown using Cronbach’s alpha, which was calculated at 0.876 for the control group and 0.706 for the intervention group.
Data collection methods
Figure 1 shows the study flow. Before any instruction, all participants completed a pre-test made up of demographic questions and checked applied-knowledge and confidence questionnaires.
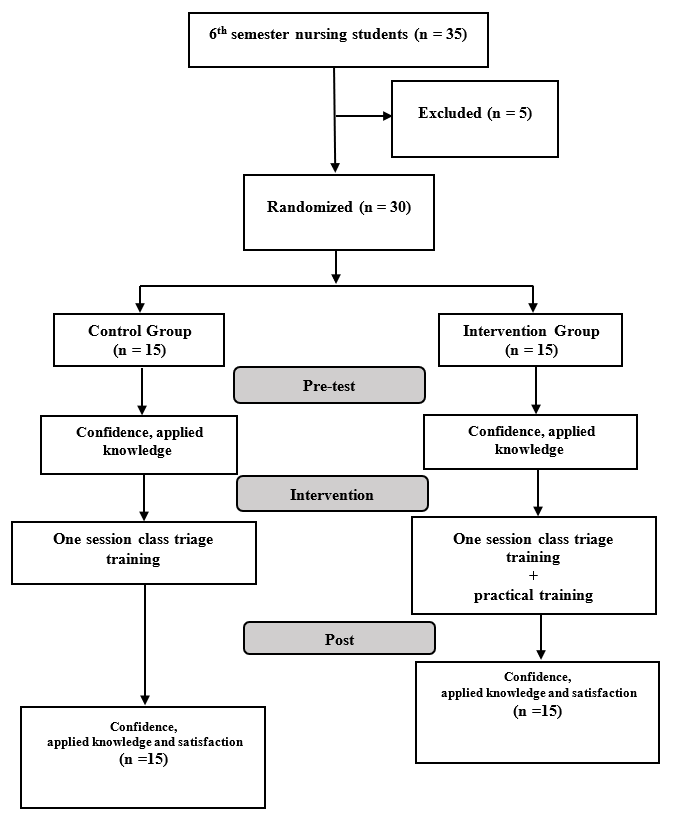
Figure 1. Flowchart of study procedure
Didactic training: A single 2-hour classroom session of the “Risk Management in Disasters and Emergencies” course covered START and Jump-START triage. The session was given by a Ph.D. faculty member from the Department of Emergency Medical Services with lots of triage-training experience.
Instruction methods included a lecture on triage theory and steps, case discussion of mass-casualty situations, a video showing a made-up bus accident triage, and guided group discussion with instructor-led feedback on student decisions.
Drill intervention: One week later, only the intervention group (n = 15) took part in an individual high-fidelity simulation—Drill— (20 minutes per student), copying a chaotic mass-casualty setting. “A drill is a coordinated, supervised exercise activity, usually used to test a single specific operation or function” [24].
To avoid interaction between control and intervention groups, ten trained undergraduate emergency-medical students acted as standardized patients, made up to show realistic wounds.
Then, each student entered the scene alone, triaged victims within the usual 30–60 seconds per patient, was watched by an evaluator who filled out a standardized checklist, and went to an isolation area after finishing the task.
A structured debrief came after each participant’s run, during which the evaluator gave feedback on decision-making and error correction. Snack packs were offered as a token of appreciation.
One month after the simulation, all 30 students repeated theapplied-knowledge, confidence, and satisfaction questionnaires.
Although control-group students were invited to join the simulation exercise, none could attend because of scheduling conflicts with their lectures and clinical internships.
Data analysis
The collected data were then analyzed using SPSS version 20, using descriptive and inferential statistics. The Shapiro-Wilk test was done to check the normality of the data distribution. Since the results showed a normal distribution, an independent t-test was used to compare the variables between groups, the Chi-square test was used to compare variables with more than one group, and paired t-tests were used to compare the scores before and after the test. Finally, ANCOVA was applied to compare post-test scores between the intervention and control groups while controlling for pre-test scores to adjust for possible baseline differences.
Results
A review of the demographics of the 30 participants showed an average age of 22.43 ± 1.36 years, with most (63.3%) being female. The details of participant characteristics are shown in Table 1 based on their group.
There were no differences between the groups in terms of starting variables.
Table 1. Characteristic profile of research samples and assessment of groups' homogeneity

Note: Independent t-test was used for comparing continuous variables between groups. Chi-square test was used for comparing categorical variables.
Abbreviations: n, number of participants; SD, standard deviation; GPA, grade point average; Sig, statistical significance; χ², Chi-square test; t, independent t-test; p, probability-value.
Paired t-tests showed that there were significant differences between the pre- and post-test scores for applied knowledge in both the control and intervention groups (p < 0.001). However, for confidence in triage, only the pre- and post-test scores in the intervention group were significant (p < 0.001) (Table 2).
Table 2. Comparison of triage applied knowledge and confidence scores pre- and post-test
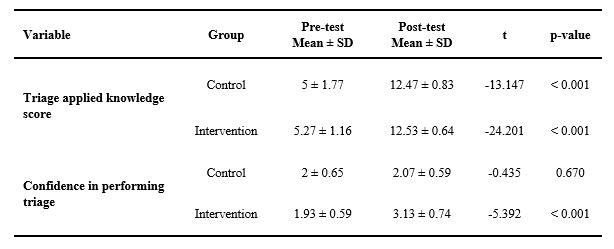
Note: Paired t-test was used to compare pre- and post-test means within each group.
Abbreviations: SD, standard deviation; t, paired t-test statistic; p, probability-value.
The ANCOVA test results (Table 3) showed that the average confidence score after training was statistically different between the intervention group (3.13) and the control group (2.06) (F = 21.67, p < 0.001, η² = 0.44). However, the average applied knowledge scores for the intervention group (12.53) and control group (12.47) were not statistically different (p = 0.76). The average satisfaction scores for the control and intervention groups were 18.87 ± 4.01 and 19.33 ± 2.72, in that order, and there were no differences between the groups (p = 0.71).
The collected data were then analyzed using SPSS version 20, using descriptive and inferential statistics. The Shapiro-Wilk test was done to check the normality of the data distribution. Since the results showed a normal distribution, an independent t-test was used to compare the variables between groups, the Chi-square test was used to compare variables with more than one group, and paired t-tests were used to compare the scores before and after the test. Finally, ANCOVA was applied to compare post-test scores between the intervention and control groups while controlling for pre-test scores to adjust for possible baseline differences.
Results
A review of the demographics of the 30 participants showed an average age of 22.43 ± 1.36 years, with most (63.3%) being female. The details of participant characteristics are shown in Table 1 based on their group.
There were no differences between the groups in terms of starting variables.
Table 1. Characteristic profile of research samples and assessment of groups' homogeneity

Note: Independent t-test was used for comparing continuous variables between groups. Chi-square test was used for comparing categorical variables.
Abbreviations: n, number of participants; SD, standard deviation; GPA, grade point average; Sig, statistical significance; χ², Chi-square test; t, independent t-test; p, probability-value.
Paired t-tests showed that there were significant differences between the pre- and post-test scores for applied knowledge in both the control and intervention groups (p < 0.001). However, for confidence in triage, only the pre- and post-test scores in the intervention group were significant (p < 0.001) (Table 2).
Table 2. Comparison of triage applied knowledge and confidence scores pre- and post-test
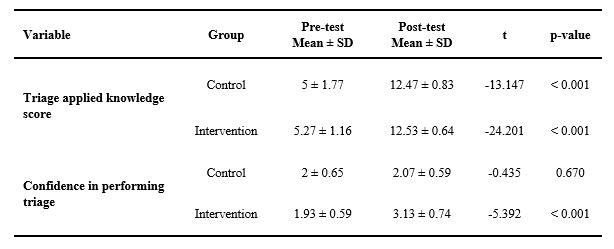
Note: Paired t-test was used to compare pre- and post-test means within each group.
Abbreviations: SD, standard deviation; t, paired t-test statistic; p, probability-value.
The ANCOVA test results (Table 3) showed that the average confidence score after training was statistically different between the intervention group (3.13) and the control group (2.06) (F = 21.67, p < 0.001, η² = 0.44). However, the average applied knowledge scores for the intervention group (12.53) and control group (12.47) were not statistically different (p = 0.76). The average satisfaction scores for the control and intervention groups were 18.87 ± 4.01 and 19.33 ± 2.72, in that order, and there were no differences between the groups (p = 0.71).
Table 3. Score changes of triage applied knowledge and confidence of intervention and control groups

Note: ANCOVA test was used to compare post-test scores between the intervention and control groups.
Abbreviations: SD, standard deviation; F, analysis of variance test statistic; p, probability-value; η², eta squared (effect size).
Discussion
This study looked at how effective drill-based START and Jump-START triage training—combined with hands-on practice—was in improving applied knowledge, confidence, and satisfaction among nursing students during MCIs.
Our results show that a single didactic session combining lectures, case discussion, and video demonstrations led to clear knowledge retention at one month, with no extra benefit from the drill exercise. In contrast, Delnavaz et al. found role-playing better than lecture-only methods for triage education [18]. The difference between our study and theirs is that we used lecture and practice for the intervention group, creating a stronger intervention with several active learning methods. Similarly, Andreatta et al. reported equal START-algorithm performance between Virtual-Reality (VR)
and standardized-patient groups, concluding that VR offers a practical, repeatable alternative for disaster-triage training [25]. Along with our findings, these data suggest that any teaching method that fully covers learning goals—whether standardized patients vs. VR or classroom plus case/video vs. hands-on simulation—can produce similar knowledge gains.
Supporting this, Pouraghaei et al. noticed important improvements in prehospital personnel knowledge and performance after START training [26], and Aslan et al. recorded clear triage knowledge increases among nursing students following first-aid instruction [27]. These show that structured triage programs reliably raise cognitive outcomes.
By contrast, only the drill group in our study yielded an important boost in self-reported confidence, both within-group and versus controls. Immersion in a high-stress, chaotic MCI scenario—coupled with immediate, performance-focused feedback—likely accounts for this effect, reflecting reports that simulation helps clinicians’ self-efficacy in acute scenarios [28-30]. Lima et al. similarly found that simulated MCI drills foster teamwork, clinical reasoning, and confidence in both helping and leading disaster responses [31], and Alshammari showed confidence gains after role-play exercises [32]. Other triage-drill studies confirm these confidence improvements among nursing students and prehospital providers [33, 34].
Although intervention-group satisfaction trended higher, the difference did not reach importance, perhaps because our control condition was itself engaging, or because the intense realism of the drill was less “enjoyable” than more gamified role-play formats reported by Khan et al. and Ahmady et al. to increase learner satisfaction [35, 36]. Equally skilled instruction across both groups may also have equalized learners’ overall experience.
This study’s limitations include its small, single-site sample (N=30), a one-month follow-up preventing long-term retention analysis, and reliance on self-reported confidence and satisfaction measures. In addition, we used one question to check the confidence of students; thus, it is recommended to use a valid and reliable scale to measure this concept. Future multicenter trials with larger cohorts, extended follow-up, objective performance metrics, and qualitative feedback will help confirm and extend these findings.
Conclusion
The study’s findings must be interpreted with caution given its small sample size. Drill‐based triage exercises significantly improved student confidence—likely reflecting the immersive, context‐rich environment they provide—whereas both drill and classroom‐based instruction produced comparable gains in applied knowledge, with no significant differences between methods. Satisfaction scores likewise did not differ significantly. These results suggest that, for objectives centered on applied‐knowledge acquisition or learner satisfaction, a blended approach of lectures, case discussion, and video shows may be as effective as full‐scale drill. Nonetheless, larger studies are needed to confirm these conclusions and to determine which specific educational outcomes get the greatest benefit from drill‐based learning. Nonetheless, further research with larger sample sizes is warranted to confirm these findings and to more precisely identify which educational outcomes benefit most from drill-based learning.
Ethical considerations
This study was approved under the ethical committee of Alborz University of Medical Sciences (IR.ABZUMS.REC.1403.219). Informed consent was gotten from all participants, including the group of undergraduate emergency medical students who acted as simulated patients in the study, as well as all nursing students prior to their involvement in the research. They were provided with detailed information about the study's purpose and the drill procedures and were assured of their right to withdraw at any time without consequences. Participation was entirely voluntary. All collected data were kept confidential and securely stored. Participants’ identities were anonymized, and any identifying information was removed to protect their privacy. At the end of the study, participants were told about the educational intervention, and any questions or concerns were answered. The present study was performed under the international ethical standards of the Declaration of Helsinki.
Artificial intelligence utilization for article writing
English language editing of this manuscript was helped by Grammarly, an AI-based writing tool. No AI tools were used for content generation, data analysis, or interpretation.
Acknowledgment
The authors would like to extend their gratitude to the Research and Technology Deputy of Alborz University of Medical Sciences for their invaluable support. Furthermore, we appreciate the students who helped with this project.
Conflict of interest statement
No conflict of interest has been declared by the authors.
Author contributions
RN and ZE were involved in the creation and organization of the study. ZE and MEA were involved in carrying out the drill and data collection. RN and PR took part in statistical analysis design. RN prepared the first draft of the manuscript. All authors contributed to the critical review and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2025/05/19 | Accepted: 2025/08/30 | Published: 2025/10/1
Received: 2025/05/19 | Accepted: 2025/08/30 | Published: 2025/10/1
References
1. Burkle FM Jr. Triage and the lost art of decoding vital signs: restoring physiologically based triage skills in complex humanitarian emergencies. Disaster Med Public Health Prep. 2018;12(1):76-85. [DOI:10.1017/dmp.2017.40]
2. Khorram-Manesh A, Nordling J, Carlström E, Goniewicz K, Faccincani R, Burkle FM. A translational triage research development tool: standardizing prehospital triage decision-making systems in mass casualty incidents. Scand J Trauma Resusc Emerg Med. 2021;29(1):119. [DOI:10.1186/s13049-021-00932-z]
3. Aslan R, Şahinöz S, Şahinöz T. Determination of START triage skill and knowledge levels of prehospital emergency medical staff: a cross sectional study. Int Emerg Nurs. 2021;56:101004. [DOI:10.1016/j.ienj.2021.101004]
4. US Department of Health and Human Services. Chemical hazards emergency medical management. Federal Register. 2018;73. [Internet]. Available from: [cited 2025 Apr 19].
5. Bhalla MC, Frey J, Rider C, Nord M, Hegerhorst M. Simple triage algorithm and rapid treatment and sort, assess, lifesaving, interventions, treatment, and transportation mass casualty triage methods for sensitivity, specificity, and predictive values. Am J Emerg Med. 2015;33(11):1687-91. [DOI:10.1016/j.ajem.2015.08.021]
6. Yancey CC, O'Rourke MC. Emergency Department Triage. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023 Aug 28.
7. Zagalioti S-C, Fyntanidou B, Exadaktylos A, Lallas K, Ziaka M. The first positive evidence that training improves triage decisions in Greece: evidence from emergency nurses at an academic tertiary care emergency department. BMC Emerg Med. 2023;23(1):60. [DOI:10.1186/s12873-023-00827-5]
8. Cusack L, Arbon P, Ranse J. What is the role of nursing students and schools of nursing during disaster? A discussion paper. Collegian. 2010;17(4):193-7. [DOI:10.1016/j.colegn.2010.09.006]
9. Fang D, Htut AM, Bednash GD, Nursing AAoCo. 2007-2008 Salaries of Instructional and Administrative Nursing Faculty in Baccalaureate and Graduate Programs in Nursing. Available from: [cited 2025 Mar 12].
10. Tayebi Z, Norouzinia R, Moatadelro Z, Pour AF, Nourian B. Nursing students' willingness to respond in disasters: a cross sectional study of facilitators and barriers. BMC Nurs. 2024;23(1):416. [DOI:10.1186/s12912-024-02088-4]
11. Javadi N, Rostamnia L, Raznahan R, Ghanbari V. Triage training in Iran from 2010 to 2020: a systematic review on educational intervention studies. Iran J Nurs Midwifery Res. 2021;26(3):189-95. [DOI:10.4103/ijnmr.IJNMR_155_20]
12. Azizpour I, Mehri S, Soola AH. Disaster preparedness knowledge and its relationship with triage decision-making among hospital and pre-hospital emergency nurses-Ardabil, Iran. BMC Health Serv Res. 2022;22(1):934. [DOI:10.1186/s12913-022-08311-9]
13. Haghigh S, Ashrafizadeh H, Mojaddami F, Kord B. A survey on knowledge level of the nurses about hospital Triage. J Nurs Educ. 2017;5(6):46-52. [DOI:10.21859/jne-05067]
14. Hedayati H, Mogharrab M, Moasheri N, Sharifzadeh G. Studying of BUMS' students' knowledge about hospital triage in 2011. Modern Care, Scientific Quarterly of Birjand Nursing and Midwifery Faculty. 2012;9(3):237-44.
15. Soola AH, Mehri S, Azizpour I. Evaluation of the factors affecting triage decision-making among emergency department nurses and emergency medical technicians in Iran: a study based on Benner's theory. BMC Emerg Med. 2022;22(1):174. [DOI:10.1186/s12873-022-00729-y]
16. Khorram-Manesh A. Teaching triage in disaster medicine-same subject, but different approach. Scand J Trauma Resusc Emerg Med. 2025;33(1):9. [DOI:10.1186/s13049-025-01322-5]
17. Alfred D, Chilton J, Connor D, Deal B, Fountain R, Hensarling J, et al. Preparing for disasters: education and management strategies explored. Nurse Educ Pract. 2015;15(1):82-9. [DOI:10.1016/j.nepr.2014.08.001]
18. Delnavaz S, Hassankhani H, Roshangar F, Dadashzadeh A, Sarbakhsh P, Ghafourifard M, et al. Comparison of scenario-based triage education by lecture and role playing on knowledge and practice of nursing students. Nurse Educ Today. 2018;70:54-9. [DOI:10.1016/j.nedt.2018.08.006]
19. Yu E, Coffey C. Prehospital mass casualty incident triage simulation builds knowledge and confidence in medical trainees. AEM Educ Train. 2024;8(2):e10962. [DOI:10.1002/aet2.10962]
20. Awwad K, Alqaissi N. Effectiveness of targeted multiple injuries nurses' training on emergency department nurses' knowledge and triage skills: a randomized control trial. Front Emerg Med. 2025;9(1). [DOI:10.18502/fem.v9i1.18067]
21. Sweeney AL, Lui YL, Watkins N, McNamee P, Samsuddin A, Huang C, et al. Simulation exercises increase staff confidence, knowledge and skills in managing mass casualty incidents: a pretest-posttest study. Tasman Med J. 2021;3(4):112-9.
22. Hamdi A, Al Thobaity A. Enhancing Disaster Triage competencies through Simulation-based training: an interventional study among undergraduate nursing students. Sustainability. 2023;15(21):15513. [DOI:10.3390/su152115513]
23. Park YM, Hwang WJ. Development and effect of a simulation-based disaster nursing education program for nursing students using standardized patients. J Nurs Res. 2024;32(1):e314. [DOI:10.1097/jnr.0000000000000596]
24. Federal Emergency Management Agency. Types of Training and Exercises. In IS-559 Emergency Management Institute Course Materials. [Internet]. Available from: [cited 2025 Apr 3].
25. Andreatta PB, Maslowski E, Petty S, Shim W, Marsh M, Hall T, et al. Virtual reality triage training provides a viable solution for disaster‐preparedness. Acad Emerg Med. 2010;17(8):870-6. [DOI:10.1111/j.1553-2712.2010.00728.x]
26. Pouraghaei M, Tabrizi JS, Moharamzadeh P, Ghafori RR, Rahmani F, Mirfakhraei BN. The effect of start triage education on knowledge and practice of emergency medical technicians in disasters. J Caring Sci. 2017;6(2):119. [DOI:10.15171/jcs.2017.012]
27. Aslan S, Yeşilçınar İ, Şahin E. Evaluation of knowledge level of nursing students receiving disaster and first aid training on triage practices during disaster: a quasi-experimental study. İnönü Üniversitesi Sağlık Hizmetleri Meslek Yüksek Okulu Dergisi. 2024;12(1):204-14. [DOI:10.33715/inonusaglik.1289603]
28. Crowe S, Ewart L, Derman S. The impact of simulation-based education on nursing confidence, knowledge and patient outcomes on general medicine units. Nurse Educ Pract. 2018;29:70-5. [DOI:10.1016/j.nepr.2017.11.017]
29. Figueroa MI, Sepanski R, Goldberg SP, Shah S. Improving teamwork, confidence, and collaboration among members of a pediatric cardiovascular intensive care unit multidisciplinary team using simulation-based team training. Pediatr Cardiol. 2013;34:612-9. [DOI:10.1007/s00246-012-0506-2]
30. Hart PL, Brannan JD, Long JM, Maguire MBR, Brooks BK, Robley LR. Effectiveness of a structured curriculum focused on recognition and response to acute patient deterioration in an undergraduate BSN program. Nurse Educ Pract. 2014;14(1):30-6. [DOI:10.1016/j.nepr.2013.06.010]
31. Lima DS, de-Vasconcelos IF, Queiroz EF, Cunha TA, Dos-Santos VS, Arruda FA, et al. Multiple victim's incident simulation: training professionals and university teaching. Rev Col Bras Cir. 2019;46(3):e20192163. [DOI:10.1590/0100-6991e-20192163]
32. Alshammari E. Simulated role-playing in pharmacy. Int J Pharm Qual Assur. 2020;11(1):176-81. [DOI:10.25258/ijpqa.11.1.27]
33. Curtis T. Lessons learned from health care students playing victim in mass casualty incident disaster drill. Int J Innov Educ Res. 2022;10(1):1-24. [DOI:10.31686/ijier.vol10.iss1.3576]
34. Strout K, Saber DA, Caruso LS, Ingwell-Spolan C, Koplovsky A, Caron EM, et al. Interprofessional mass casualty incident simulation design protocol to prepare prelicensure nursing students to respond to a disaster. Nurse Educ. 2017;42(5):E1-4. [DOI:10.1097/NNE.0000000000000365]
35. Khan HS, Sheikh NS. Role-play: a simulated teaching technique in physiology. Pak J Physiol. 2021;17(4):46-50. [DOI:10.69656/pjp.v17i4.1288]
36. Ahmady S, Shahbazi S, Khajeali N. Comparing the effect of traditional and role-play training methods on nursing students' performance and satisfaction in the principles of patient education course. J Educ Health Promot. 2021;10(1):146. [DOI:10.4103/jehp.jehp_722_20]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |