Mon, Feb 23, 2026
[Archive]
Volume 18, Issue 3 (2025)
J Med Edu Dev 2025, 18(3): 145-154 |
Back to browse issues page
Ethics code: PMCH&RI/IHEC/2024/202, Dated: 06/08/2024
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Surapaneni K M. Design, development and validation of the “START CBME” module: a foundational program to acquaint first-year medical students with competency-based medical education. J Med Edu Dev 2025; 18 (3) :145-154
URL: http://edujournal.zums.ac.ir/article-1-2384-en.html
URL: http://edujournal.zums.ac.ir/article-1-2384-en.html
Department of Biochemistry, Panimalar Medical College Hospital & Research Institute, Varadharajapuram, Poonamallee, Chennai – 600 123, Tamil Nadu, India. & Department of Medical Education, Panimalar Medical College Hospital & Research Institute, Varadharajapuram, Poonamallee, Chennai – 600 123, Tamil Nadu, India. , krishnamohan.surapaneni@gmail.com
Keywords: CBME, medical education, competency-based learning, student engagement, early sensitization, structured training
Full-Text [PDF 748 kb]
(298 Downloads)
| Abstract (HTML) (1170 Views)
Full-Text: (44 Views)
Abstract
Background & Objective: Competency-Based Medical Education (CBME), introduced by the National Medical Commission (NMC) in India in 2019 and revised in 2024, represents a transformative shift toward outcome-driven, learner-centered medical training. Despite faculty development efforts, a gap remains in sensitizing medical students to CBME early in their education. This study aimed to develop and evaluate the START CBME (Sensitization and Training for Adapting to the Requirements of Transition in CBME) module to enhance first-year medical students' understanding and engagement with CBME.
Materials & Methods: A needs assessment was conducted among first-year medical students to evaluate their Knowledge, Attitudes, and Practices (KAP) regarding CBME. Based on findings, a structured module was developed, incorporating interactive lectures, small-group discussions, reflective exercises, and competency-mapping activities. The content validity of the module was evaluated using a Content Validity Index (CVI) of 0.92, while its reliability was confirmed with a Cronbach’s alpha of 0.87. It was pilot-tested among 24 students selected through random stratified sampling. Pre- and post-intervention assessments were conducted using a validated questionnaire, and statistical analysis measured the module’s impact.
Results: Post-intervention, knowledge scores improved significantly (p < 0.001), and student attitudes toward CBME became more positive. Participants rated the module highly for clarity, relevance, and effectiveness in easing their transition to CBME.
Conclusion: Early CBME sensitization through structured training improves student engagement, knowledge, and readiness for competency-based learning. The START CBME module serves as a replicable model for institutions seeking to enhance CBME preparedness among medical students.
Introduction
Competency-Based Medical Education (CBME), introduced by the National Medical Commission (NMC) in India in 2019 with revised guidelines released on Sep 12, 2024 [1], represents a paradigm shift in medical training. Unlike traditional time-based education models, CBME emphasizes learner progression based on demonstrated competence, ensuring that medical graduates are equipped with essential skills, knowledge, and professional behaviors necessary for high-quality patient care [2]. However, despite its structured framework, the transition to CBME in India has presented significant challenges, particularly for medical students who are accustomed to passive, exam-driven learning methodologies [3].
CBME is grounded in the philosophy of outcome-based education, wherein the curriculum is meticulously structured around explicitly defined competencies across diverse domains such as medical expertise, patient care, communication, professionalism, and systems-based practice [4]. By establishing clear performance benchmarks, CBME ensures that every medical graduate meets a standardized level of proficiency necessary for high-quality patient care [5]. The successful implementation of CBME relies heavily on medical institutions and faculty, who are tasked with not only delivering competency-based curricula but also fostering a supportive learning environment [6]. Faculty development programs ranging from Basic to Advanced training in medical education have been widely implemented to equip educators with the necessary pedagogical tools for CBME execution [7]. However, these efforts have largely focused on training faculty rather than preparing students to adapt to the new learning paradigm. Research indicates that while faculty members may be well-versed in CBME principles, students often struggle to engage with this educational shift due to a lack of early orientation and structured guidance [8]. Despite the established CBME structure and faculty development efforts, students still struggle to fully realize the intended benefits of the curriculum, often because they lack awareness of the foundational principles and the underlying meaning behind the CBME components [9]. A study conducted revealed that first-year students often experience confusion and anxiety when transitioning from traditional lecture-based learning to the self-directed, competency-driven approach required in CBME [10]. In particular, the sudden shift in assessment strategies from rote memorization to formative, workplace-based evaluations has been cited as a major source of student stress [11]. Without adequate sensitization, many students perceive CBME as an additional burden rather than a structured framework designed to enhance their learning experience. Medical students often feel like complete beginners as they start their journey in medical school. The learning environment, teaching faculty, curriculum, and various learning approaches can differ significantly, leaving students feeling overwhelmed about their performance. They are now expected to take greater responsibility for their learning, moving beyond passive absorption of knowledge to actively engaging in the learning process. This requires a higher level of discipline, adaptability, and a proactive approach to education [12]. Given these challenges, there is a pressing need for structured early sensitization programs that introduce students to CBME principles in a clear, engaging, and supportive manner. To address this gap, we developed the START CBME (Sensitization and Training for Adapting to the Requirements of Transition in CBME) module—a structured orientation program designed specifically for first-year medical students. This initiative is aimed at bridging the knowledge gap, easing the transition to competency-based learning, and equipping students with the necessary mindset to thrive in CBME [13]. It is important for students to recognize that CBME is not merely a curricular innovation or a pedagogical trend; it is rather a transformative approach that redefines what it means to be a medical professional [14]. Without a proper introduction to CBME's underlying philosophy, students may perceive the demands of this new approach as burdensome or even arbitrary. This misalignment can lead to disengagement, as students struggle to see the relevance of the competencies they are being asked to develop. Early sensitization, therefore, serves as a critical bridge between students' prior educational experiences and the new expectations placed upon them. It is essential that this sensitization goes beyond a superficial introduction to CBME's mechanics. It should involve a deep, reflective engagement with the principles of competency-based learning, helping students to internalize the notion that medical education is not about accumulating knowledge for its own sake, but about developing the skills, attitudes, and behaviors that will enable them to serve their future patients effectively [15].
Furthermore, this early engagement with CBME can cultivate a mindset of lifelong learning and adaptability. As students come to understand that their education is not a finite process but a continuous journey of professional development, they are more likely to embrace the self-directed learning, critical reflection, and continuous improvement that CBME encourages [16]. In this way, early sensitization to CBME does more than prepare students for the immediate challenges of medical school; it lays the foundation for a career characterized by competence, compassion, and a commitment to excellence.
Materials & Methods
Design and setting(s)
This study was conducted in two phases at Panimalar Medical College Hospital & Research Institute, Chennai, India. The first phase involved a cross-sectional needs assessment to evaluate first-year medical students' baseline KAP regarding CBME. The second phase was a quasi-experimental pre-post pilot study designed to assess the effectiveness of the START CBME module in improving students' understanding and engagement with CBME principles. Approval was obtained from the Institutional Ethics Committee of Panimalar Medical College Hospital & Research Institute (PMCHRI-IHEC) prior to the start of this study (Approval Number: PMCH&RI/IHEC/2024/202; dated: 06.08.2024).
Participants and sampling
For the needs assessment, 150 first-year medical students were recruited through convenience sampling to participate in a structured questionnaire-based survey. In the pilot testing phase, 24 students were randomly selected using stratified random sampling to ensure diverse representation. These students completed a pre-test, engaged with the START CBME module for two weeks, and then completed a post-test and feedback survey to evaluate the module’s impact.
Tools/Instruments
The needs assessment was conducted with 150 first-year medical students to evaluate their knowledge, attitudes, and practices concerning the core components of Competency-Based Medical Education (CBME) using a 36-item validated online questionnaire. The questionnaire comprised 9 knowledge, 15 attitude, and 12 practice-based questions. Reliability testing revealed a high Cronbach’s alpha of 0.86, indicating strong internal consistency. The knowledge responses were structured as Yes/No/Not Sure. Attitudes and practices were assessed using a 5-point Likert scale (Strongly Agree/Agree/Neither Agree nor Disagree/Disagree/Strongly Disagree for attitudes and Always/Often/Sometimes/Rarely/Never for practices).
The knowledge section assessed students' familiarity with key CBME principles, including competency-based assessment methods, the role of self-directed learning, active learning strategies such as flipped classrooms and small-group discussions, constructivist learning theory, and the significance of group dynamics in medical education.
The attitudes section evaluated students' perceptions of CBME's effectiveness in preparing them for real-world medical practice, their comfort with competency-based assessment over traditional time-bound progression, and their willingness to engage in self-directed and reflective learning approaches. The practices section measured students' prior engagement with CBME-aligned learning methodologies, including participation in structured reflection sessions, usage of logbooks, involvement in formative assessments, engagement with simulated learning environments, and experience with feedback-driven competency assessments. The needs assessment results revealed a mean knowledge score of 4.4 ± 1.2 out of 9, knowledge
knowledge score of 4.4 ± 1.2 out of 9, indicating limited awareness of CBME principles. The mean attitude score was 6.2 ± 0.8 out of 15, demonstrating moderate acceptance but uncertainty about CBME’s effectiveness. The mean practice score was 5.3 ± 1.1 out of 12, suggesting infrequent engagement with CBME methodologies. These findings highlighted a critical gap in student preparedness. The START CBME module was then designed as a comprehensive structured orientation program for first-year medical students [17] . The module included all components described in the NMC-mandated Revised CBME Curriculum (2024). Unlike conventional orientation programs, the START CBME module integrates competency-based learning strategies with structured guidance on adapting to medical education. It incorporates reflective exercises grounded in constructivist learning theory, allowing students to develop self-awareness, critical thinking, and adaptability. This theoretical framework was chosen to promote experiential learning, emphasizing active engagement over passive knowledge acquisition. The conceptual framework of the design of START CBME module is given in Figure 1. The 32 components described in the module include: Rethinking Your Approach to Learning, Introduction to Adult Learning Principles, The 12+1 Roles of Student in Medical Education, Educational Theories and Principles, Introduction to CBME, Roles of the Indian Medical Graduate (IMG), Understanding Goals, Competencies & Learning Objectives, Overview of Group Dynamics, Foundation Course, Alignment & Integration, Early Clinical Exposure (ECE), Attitudes, Ethics and Communication (AETCOM), Role of Logbooks, Role of Electives, Family Adoption Program (FAP), Mentorship in Medical Education, Personal Well-Being, Managing Stress & Burnout, Coping with Failure, Introduction to the Learner-Doctor Method, Research, Emerging Role of Artificial Intelligence, Pandemic Management, Online Learning & Assessment, Simulation-Based Learning, Large Group Teaching (LGT), Small Group Teaching (SGT), Self-Directed Learning (SDL), Flipped Classroom, Demonstrate, Observe, Assist and Perform (DOAP), Assessments in Medical Education, Entrustable Professional Activities (EPA), Effective Feedback for Learning, and Evaluation & Student Feedback. These components orient students to the CBME framework and provide strategies to adapt from their first professional year to internship.

Data collection methods
Validation of the Module
The validity and reliability of the START CBME module were assessed using a 36-item online questionnaire. Purposive sampling was used to recruit 10 medical education experts, consisting of internal and external faculty members at the level of Professor or Associate Professor, all of whom were members of their institution’s Medical Education Unit or curriculum committee. An email invitation with a SurveyMonkey link and a soft copy of the module was sent, with a follow-up reminder after one week.
Face validity was performed to evaluate the module’s clarity, relevance, and suitability, providing an average evaluation score of 4.7/5 across all criteria. Content validity was assessed using both the Item Content Validity Index (I-CVI) for individual components and the Scale Content Validity Index for Universal Agreement (S-CVI/UA). Reliability was confirmed with an Intraclass Correlation Coefficient (ICC) of 0.87, indicating strong internal consistency and reproducibility. These specific validity measures were chosen to ensure a robust evaluation of the module’s effectiveness. Face validity assessed the comprehensibility and usability of the content. The I-CVI and S-CVI/UA established content alignment with CBME principles. The ICC measured consistency across multiple evaluators, confirming the module’s reliability in different educational settings.
Pilot testing & evaluation of the module
Following validation, the START CBME module was pilot-tested with 24 first-year medical students. As this was a pilot study, medical students were invited to participate, and out of the volunteers, 24 were selected by randomization which was performed using a computerized selection algorithm to ensure unbiased allocation. Random stratified sampling was applied to ensure diverse representation across gender and academic backgrounds, minimizing selection bias. Written informed consent was obtained from all students. A pre-test assessment was conducted using 25 scenario-based multiple-choice questions, designed to evaluate students’ ability to apply CBME principles in real-world medical training situations. The test covered key areas such as competency mapping, self-directed learning, formative assessments, and professionalism. The module was provided in hard copy format for self-paced study over two weeks. A post-test was then conducted, using the same 25 MCQs, to measure improvement in students’ application of CBME concepts. To evaluate the module’s usability and effectiveness, a 9-item feedback questionnaire was administered using a 10-point rating scale, assessing clarity, relevance, ease of use, and impact on learning.
Data analysis
Pre- and post-test scores were analyzed using paired t-tests to assess the significance of knowledge improvement. Descriptive statistics summarized student feedback on the module. Validation metrics, including I-CVI, S-CVI/UA, and ICC, were employed to evaluate content validity and reliability. All statistical analyses were conducted using the Statistical Package for Social Sciences (SPSS), version 17, developed by SPSS Inc., USA, for Microsoft Windows. A p-value of less than 0.05 was considered statistically significant.
Results
The needs assessment revealed significant gaps in students' knowledge, attitudes, and practices regarding CBE. Knowledge scores were notably low (4.4 ± 1.2 out of 9), with a high frequency of “Not sure” responses, particularly in areas such as competency-based assessments, self-directed learning strategies, and group dynamics. More than 60% of students were unfamiliar with the flipped classroom model, and over 65% lacked awareness of formative assessments and their role in CBME.
Attitude scores were also suboptimal (6.2 ± 0.8 out of 15), with the majority of students selecting “Neither agree nor disagree” or lower, indicating uncertainty about CBME’s effectiveness. Notably, only 28% of students agreed that CBME adequately prepares them for real-world medical practice, while 35% expressed concerns about their ability to engage in self-directed learning.
Practices related to CBE were infrequent, as reflected in the predominance of “Rarely” and “Never” responses across the 12 practice items, with an overall practice score of 5.3 ± 1.1. Only 22% of students reported regularly engaging in self-directed learning, and fewer than 30% had experience with structured reflection sessions, which are integral to CBME. These findings highlight a critical need for targeted interventions to enhance students’ understanding, foster more positive attitudes, and improve their practical engagement with CBME principles (Figure 2).
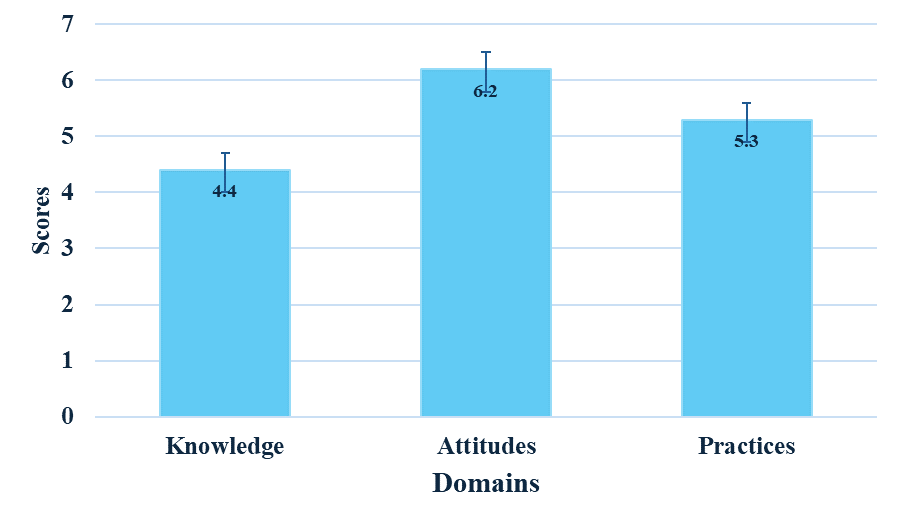
Figure 2. Needs assessment revealing knowledge, attitudes, and practices of first-year medical students
This figure presents baseline scores showing low knowledge (4.4), moderate attitudes (6.2), and limited practices (5.3) in Competency-Based Medical Education (CBME).
The module demonstrated high validity and reliability, confirming its effectiveness as a structured orientation tool for CBME. Face validity yielded an average evaluation score of 0.97 ± 0.048, reflecting strong agreement among experts regarding the module’s clarity, relevance, and usability.
Content validity results were equally strong, with an I-CVI of 0.97 ± 0.048 and a S-CVI/UA of 0.95 ± 0.046, confirming that the module comprehensively covers essential CBME components.
Reliability assessment yielded an ICC of 0.87, indicating strong internal consistency and reproducibility across different evaluators. Pre-test results, measured with 25 scenario-based multiple-choice questions, showed an average score of 8.0 ± 2.1, indicating limited initial comprehension of CBME concepts and their application in clinical and educational settings. Students particularly struggled with competency mapping, Entrustable Professional Activities (EPAs), and self-directed learning principles, where over 65% of responses were incorrect.
Following two weeks of module engagement, post-test scores improved significantly to an average of 21.2 ± 1.8, with a statistically significant difference (p < 0.0001).
The highest improvements were observed in applying competency-based assessment principles (average score increase of 64%) and understanding self-directed learning strategies (increase of 58%). These results suggest that the module was effective in enhancing students’ ability to apply CBME concepts in a structured and meaningful manner.
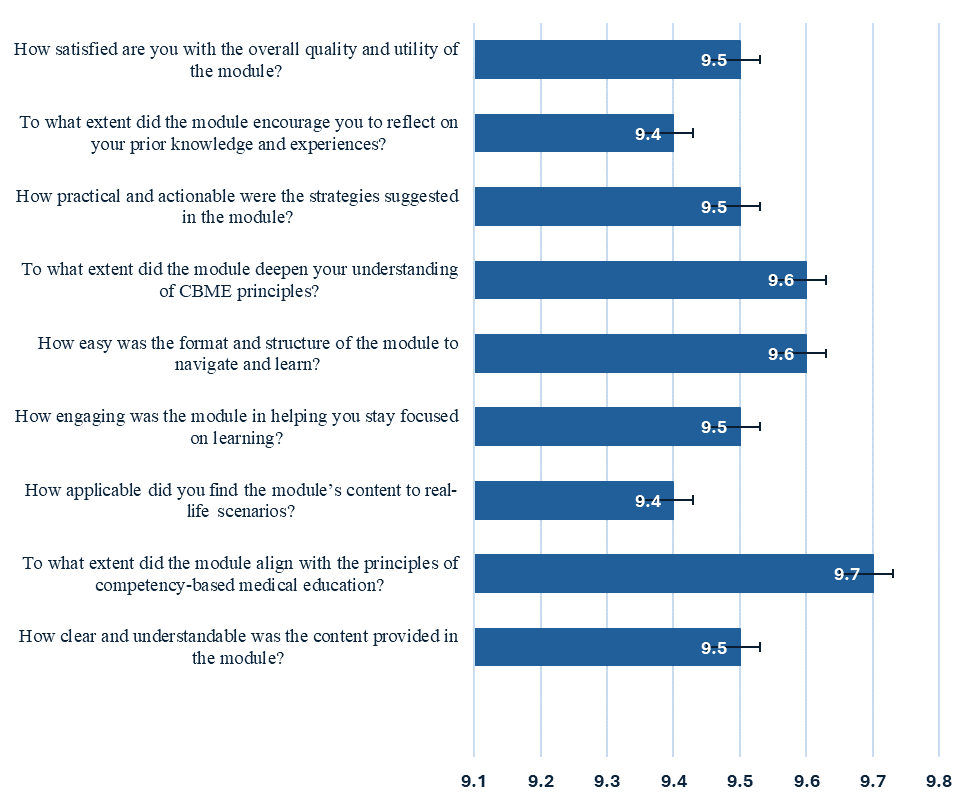
Feedback on the module was collected using a 9-item questionnaire rated on a 10-point scale, providing insights into its clarity, relevance, and practical value. Students expressed high satisfaction, with ratings consistently above 9.4 across all parameters (Figure 3). Specifically, 95% of students reported that the module effectively clarified CBME principles and their role in medical education. Additionally, 92% of students found the reflective exercises particularly useful in helping them internalize competency-based learning concepts, while 94% agreed that the module provided actionable strategies for transitioning into CBME.
Overall, the results indicate that the START CBME module significantly improved students’ knowledge, attitudes, and practical engagement with CBME, effectively addressing the gaps identified in the needs assessment.
Discussion
The shift to CBME is equally challenging for medical students. The transition is not just about mastering content but clearly understanding the purpose and relevance behind each component of CBME such that they are guided in an informed and responsible way. Studies conducted previously have explored students’ positive perceptions towards CBME through faculty-driven and curriculum-based implementations [18, 19]. However, students’ ability to comprehend the meaning behind each component is not well studied. A study conducted in an Indian medical school found that while students appreciated the emphasis on competencies, many struggled with self-directed learning and competency-based assessments due to a lack of structured orientation at the beginning of their medical education [20]. Similar concerns have been reported in studies from the UK and Canada, where students transitioning into CBME expressed difficulty in adapting to entrustable professional activities and formative assessments without early guidance [21, 22].
The introduction of START CBME module stands as a critical need for first professional medical students to get acquainted about CBME. The module has been validated
for its content with high reliability scores. By embedding reflective exercises and aligning content with the NMC’s revised guidelines, the module not only addresses knowledge deficits but also fosters a proactive learning mindset among students [23]. Compared to other CBME orientation programs, START CBME distinguishes itself by integrating constructivist learning principles with competency mapping exercises, a feature lacking in traditional foundation courses offered in Indian medical colleges. An analysis of early CBME sensitization programs in Singapore suggests that incorporating structured self-reflection significantly enhances student engagement with competency-based frameworks [24]. The strong post-test gains observed in this study align with these international findings, reinforcing the importance of reflective learning in medical education.
The significant gains in post-test scores, coupled with positive feedback on module clarity and relevance, highlight the importance of familiarizing students with CBME principles from the onset of their medical education. The improvement in self-directed learning scores is particularly noteworthy, as previous studies have reported that Indian medical students often struggle with autonomous learning due to a predominantly teacher-driven pre-university education [25]. Addressing this gap early may improve students’ adaptability and engagement in competency-based curricula.
Furthermore, the structured, outcome-based approach of START CBME supports students in transitioning from passive learning to an active, self-directed educational model.
This shift is essential in preparing future physicians who are adaptable, skilled, and committed to continuous professional development [26]. In the context of CBME implementation in India, these findings suggest that early exposure to competency-based learning frameworks should become a standardized component of the medical curriculum [27]. Faculty development efforts have primarily focused on training educators in CBME principles, but student sensitization remains an overlooked aspect [28]. Integrating structured CBME orientation modules within the foundation course could address this issue, ensuring that students and faculty progress toward competency-based learning with shared expectations.
Despite these strengths, this study has some limitations. The pilot test was conducted with a relatively small sample of 24 students, which may limit the generalizability of the findings. Additionally, as this was a single-institution study, variations in curriculum delivery and institutional support structures in other medical schools may influence the effectiveness of the module in different settings. Future research should expand the sample size and evaluate the module’s impact across multiple institutions to ensure its broader applicability. Longitudinal studies assessing the retention of CBME concepts and their influence on student performance in later academic years would provide valuable insights into the long-term effectiveness of CBME sensitization.
Future research should also explore the long-term impact of CBME orientation modules on clinical performance, assessment scores, and professional development. A mixed-methods approach incorporating qualitative feedback from students and faculty could provide deeper insights into the challenges and benefits of CBME sensitization. Furthermore, the integration of technology-enhanced learning tools could be investigated to enhance the effectiveness of competency-based training.
The module’s design and outcomes could serve as a model for other institutions aiming to enhance CBME comprehension and engagement, contributing to the broader goal of quality-driven medical education in India. As competency-based education continues to evolve, early sensitization programs such as START CBME could play a pivotal role in bridging the gap between traditional medical training and outcome-driven learning, ultimately shaping more competent and self-directed healthcare professionals.
Conclusion
The START CBME module provides a structured and reflective approach to bridging the transition from traditional learning to competency-based medical education for first-year students. By introducing CBME principles early, the module enhances student understanding, fosters self-directed learning, and improves engagement with competency-based training. The significant gains in knowledge, attitudes, and practical application of CBME concepts highlight its effectiveness in addressing the initial challenges students face in adapting to this educational model. These findings underscore the importance of structured CBME sensitization programs in fostering adaptability, critical thinking, and professional responsibility among medical students.
As competency-based education becomes the standard in medical training, this module can serve as a model for institutions aiming to strengthen student readiness, ensuring a smoother transition into CBME and promoting lifelong learning habits essential for future healthcare professionals.
Ethical considerations
This study was approved by the Institutional Human Ethics Committee of Panimalar Medical College Hospital & Research Institute, PMCH&RI/IHEC/2024/202, Dated: 06/08/2024. All data collected was used only for research purpose and confidentiality was maintained throughout the study.
Artificial intelligence utilization for article writing
No artificial intelligence (AI) tools were used for the writing of this article
Acknowledgment
None to be acknowledged.
Conflict of interest statement
None to be declared.
Author contributions
Conceptualization: KMS; Methodology: KMS; Software: KMS; Validation: KMS; Formal analysis: KMS; Investigation: KMS; Resources: KMS; Data curation: KMS; Writing—original draft preparation: KMS; Writing—review and editing: KMS; Visualization: KMS; Supervision: KMS; Project administration: KMS; and Funding acquisition: KMS. All authors have read and agreed to the published version of the manuscript.
Funding
None to be declared
Data availability statement
All information is available in the article.
Background & Objective: Competency-Based Medical Education (CBME), introduced by the National Medical Commission (NMC) in India in 2019 and revised in 2024, represents a transformative shift toward outcome-driven, learner-centered medical training. Despite faculty development efforts, a gap remains in sensitizing medical students to CBME early in their education. This study aimed to develop and evaluate the START CBME (Sensitization and Training for Adapting to the Requirements of Transition in CBME) module to enhance first-year medical students' understanding and engagement with CBME.
Materials & Methods: A needs assessment was conducted among first-year medical students to evaluate their Knowledge, Attitudes, and Practices (KAP) regarding CBME. Based on findings, a structured module was developed, incorporating interactive lectures, small-group discussions, reflective exercises, and competency-mapping activities. The content validity of the module was evaluated using a Content Validity Index (CVI) of 0.92, while its reliability was confirmed with a Cronbach’s alpha of 0.87. It was pilot-tested among 24 students selected through random stratified sampling. Pre- and post-intervention assessments were conducted using a validated questionnaire, and statistical analysis measured the module’s impact.
Results: Post-intervention, knowledge scores improved significantly (p < 0.001), and student attitudes toward CBME became more positive. Participants rated the module highly for clarity, relevance, and effectiveness in easing their transition to CBME.
Conclusion: Early CBME sensitization through structured training improves student engagement, knowledge, and readiness for competency-based learning. The START CBME module serves as a replicable model for institutions seeking to enhance CBME preparedness among medical students.
Introduction
CBME is grounded in the philosophy of outcome-based education, wherein the curriculum is meticulously structured around explicitly defined competencies across diverse domains such as medical expertise, patient care, communication, professionalism, and systems-based practice [4]. By establishing clear performance benchmarks, CBME ensures that every medical graduate meets a standardized level of proficiency necessary for high-quality patient care [5]. The successful implementation of CBME relies heavily on medical institutions and faculty, who are tasked with not only delivering competency-based curricula but also fostering a supportive learning environment [6]. Faculty development programs ranging from Basic to Advanced training in medical education have been widely implemented to equip educators with the necessary pedagogical tools for CBME execution [7]. However, these efforts have largely focused on training faculty rather than preparing students to adapt to the new learning paradigm. Research indicates that while faculty members may be well-versed in CBME principles, students often struggle to engage with this educational shift due to a lack of early orientation and structured guidance [8]. Despite the established CBME structure and faculty development efforts, students still struggle to fully realize the intended benefits of the curriculum, often because they lack awareness of the foundational principles and the underlying meaning behind the CBME components [9]. A study conducted revealed that first-year students often experience confusion and anxiety when transitioning from traditional lecture-based learning to the self-directed, competency-driven approach required in CBME [10]. In particular, the sudden shift in assessment strategies from rote memorization to formative, workplace-based evaluations has been cited as a major source of student stress [11]. Without adequate sensitization, many students perceive CBME as an additional burden rather than a structured framework designed to enhance their learning experience. Medical students often feel like complete beginners as they start their journey in medical school. The learning environment, teaching faculty, curriculum, and various learning approaches can differ significantly, leaving students feeling overwhelmed about their performance. They are now expected to take greater responsibility for their learning, moving beyond passive absorption of knowledge to actively engaging in the learning process. This requires a higher level of discipline, adaptability, and a proactive approach to education [12]. Given these challenges, there is a pressing need for structured early sensitization programs that introduce students to CBME principles in a clear, engaging, and supportive manner. To address this gap, we developed the START CBME (Sensitization and Training for Adapting to the Requirements of Transition in CBME) module—a structured orientation program designed specifically for first-year medical students. This initiative is aimed at bridging the knowledge gap, easing the transition to competency-based learning, and equipping students with the necessary mindset to thrive in CBME [13]. It is important for students to recognize that CBME is not merely a curricular innovation or a pedagogical trend; it is rather a transformative approach that redefines what it means to be a medical professional [14]. Without a proper introduction to CBME's underlying philosophy, students may perceive the demands of this new approach as burdensome or even arbitrary. This misalignment can lead to disengagement, as students struggle to see the relevance of the competencies they are being asked to develop. Early sensitization, therefore, serves as a critical bridge between students' prior educational experiences and the new expectations placed upon them. It is essential that this sensitization goes beyond a superficial introduction to CBME's mechanics. It should involve a deep, reflective engagement with the principles of competency-based learning, helping students to internalize the notion that medical education is not about accumulating knowledge for its own sake, but about developing the skills, attitudes, and behaviors that will enable them to serve their future patients effectively [15].
Furthermore, this early engagement with CBME can cultivate a mindset of lifelong learning and adaptability. As students come to understand that their education is not a finite process but a continuous journey of professional development, they are more likely to embrace the self-directed learning, critical reflection, and continuous improvement that CBME encourages [16]. In this way, early sensitization to CBME does more than prepare students for the immediate challenges of medical school; it lays the foundation for a career characterized by competence, compassion, and a commitment to excellence.
Materials & Methods
Design and setting(s)
This study was conducted in two phases at Panimalar Medical College Hospital & Research Institute, Chennai, India. The first phase involved a cross-sectional needs assessment to evaluate first-year medical students' baseline KAP regarding CBME. The second phase was a quasi-experimental pre-post pilot study designed to assess the effectiveness of the START CBME module in improving students' understanding and engagement with CBME principles. Approval was obtained from the Institutional Ethics Committee of Panimalar Medical College Hospital & Research Institute (PMCHRI-IHEC) prior to the start of this study (Approval Number: PMCH&RI/IHEC/2024/202; dated: 06.08.2024).
Participants and sampling
For the needs assessment, 150 first-year medical students were recruited through convenience sampling to participate in a structured questionnaire-based survey. In the pilot testing phase, 24 students were randomly selected using stratified random sampling to ensure diverse representation. These students completed a pre-test, engaged with the START CBME module for two weeks, and then completed a post-test and feedback survey to evaluate the module’s impact.
Tools/Instruments
The needs assessment was conducted with 150 first-year medical students to evaluate their knowledge, attitudes, and practices concerning the core components of Competency-Based Medical Education (CBME) using a 36-item validated online questionnaire. The questionnaire comprised 9 knowledge, 15 attitude, and 12 practice-based questions. Reliability testing revealed a high Cronbach’s alpha of 0.86, indicating strong internal consistency. The knowledge responses were structured as Yes/No/Not Sure. Attitudes and practices were assessed using a 5-point Likert scale (Strongly Agree/Agree/Neither Agree nor Disagree/Disagree/Strongly Disagree for attitudes and Always/Often/Sometimes/Rarely/Never for practices).
The knowledge section assessed students' familiarity with key CBME principles, including competency-based assessment methods, the role of self-directed learning, active learning strategies such as flipped classrooms and small-group discussions, constructivist learning theory, and the significance of group dynamics in medical education.
The attitudes section evaluated students' perceptions of CBME's effectiveness in preparing them for real-world medical practice, their comfort with competency-based assessment over traditional time-bound progression, and their willingness to engage in self-directed and reflective learning approaches. The practices section measured students' prior engagement with CBME-aligned learning methodologies, including participation in structured reflection sessions, usage of logbooks, involvement in formative assessments, engagement with simulated learning environments, and experience with feedback-driven competency assessments. The needs assessment results revealed a mean knowledge score of 4.4 ± 1.2 out of 9, knowledge
knowledge score of 4.4 ± 1.2 out of 9, indicating limited awareness of CBME principles. The mean attitude score was 6.2 ± 0.8 out of 15, demonstrating moderate acceptance but uncertainty about CBME’s effectiveness. The mean practice score was 5.3 ± 1.1 out of 12, suggesting infrequent engagement with CBME methodologies. These findings highlighted a critical gap in student preparedness. The START CBME module was then designed as a comprehensive structured orientation program for first-year medical students [17] . The module included all components described in the NMC-mandated Revised CBME Curriculum (2024). Unlike conventional orientation programs, the START CBME module integrates competency-based learning strategies with structured guidance on adapting to medical education. It incorporates reflective exercises grounded in constructivist learning theory, allowing students to develop self-awareness, critical thinking, and adaptability. This theoretical framework was chosen to promote experiential learning, emphasizing active engagement over passive knowledge acquisition. The conceptual framework of the design of START CBME module is given in Figure 1. The 32 components described in the module include: Rethinking Your Approach to Learning, Introduction to Adult Learning Principles, The 12+1 Roles of Student in Medical Education, Educational Theories and Principles, Introduction to CBME, Roles of the Indian Medical Graduate (IMG), Understanding Goals, Competencies & Learning Objectives, Overview of Group Dynamics, Foundation Course, Alignment & Integration, Early Clinical Exposure (ECE), Attitudes, Ethics and Communication (AETCOM), Role of Logbooks, Role of Electives, Family Adoption Program (FAP), Mentorship in Medical Education, Personal Well-Being, Managing Stress & Burnout, Coping with Failure, Introduction to the Learner-Doctor Method, Research, Emerging Role of Artificial Intelligence, Pandemic Management, Online Learning & Assessment, Simulation-Based Learning, Large Group Teaching (LGT), Small Group Teaching (SGT), Self-Directed Learning (SDL), Flipped Classroom, Demonstrate, Observe, Assist and Perform (DOAP), Assessments in Medical Education, Entrustable Professional Activities (EPA), Effective Feedback for Learning, and Evaluation & Student Feedback. These components orient students to the CBME framework and provide strategies to adapt from their first professional year to internship.

Figure 1. Conceptual framework of the START CBME module
This figure illustrates challenges in transitioning to Competency-Based Medical Education (CBME) and how the START CBME module addresses these gaps through a structured, student-centered approach, enhancing understanding, confidence, and engagement in CBME.
This figure illustrates challenges in transitioning to Competency-Based Medical Education (CBME) and how the START CBME module addresses these gaps through a structured, student-centered approach, enhancing understanding, confidence, and engagement in CBME.
Data collection methods
Validation of the Module
The validity and reliability of the START CBME module were assessed using a 36-item online questionnaire. Purposive sampling was used to recruit 10 medical education experts, consisting of internal and external faculty members at the level of Professor or Associate Professor, all of whom were members of their institution’s Medical Education Unit or curriculum committee. An email invitation with a SurveyMonkey link and a soft copy of the module was sent, with a follow-up reminder after one week.
Face validity was performed to evaluate the module’s clarity, relevance, and suitability, providing an average evaluation score of 4.7/5 across all criteria. Content validity was assessed using both the Item Content Validity Index (I-CVI) for individual components and the Scale Content Validity Index for Universal Agreement (S-CVI/UA). Reliability was confirmed with an Intraclass Correlation Coefficient (ICC) of 0.87, indicating strong internal consistency and reproducibility. These specific validity measures were chosen to ensure a robust evaluation of the module’s effectiveness. Face validity assessed the comprehensibility and usability of the content. The I-CVI and S-CVI/UA established content alignment with CBME principles. The ICC measured consistency across multiple evaluators, confirming the module’s reliability in different educational settings.
Pilot testing & evaluation of the module
Following validation, the START CBME module was pilot-tested with 24 first-year medical students. As this was a pilot study, medical students were invited to participate, and out of the volunteers, 24 were selected by randomization which was performed using a computerized selection algorithm to ensure unbiased allocation. Random stratified sampling was applied to ensure diverse representation across gender and academic backgrounds, minimizing selection bias. Written informed consent was obtained from all students. A pre-test assessment was conducted using 25 scenario-based multiple-choice questions, designed to evaluate students’ ability to apply CBME principles in real-world medical training situations. The test covered key areas such as competency mapping, self-directed learning, formative assessments, and professionalism. The module was provided in hard copy format for self-paced study over two weeks. A post-test was then conducted, using the same 25 MCQs, to measure improvement in students’ application of CBME concepts. To evaluate the module’s usability and effectiveness, a 9-item feedback questionnaire was administered using a 10-point rating scale, assessing clarity, relevance, ease of use, and impact on learning.
Data analysis
Pre- and post-test scores were analyzed using paired t-tests to assess the significance of knowledge improvement. Descriptive statistics summarized student feedback on the module. Validation metrics, including I-CVI, S-CVI/UA, and ICC, were employed to evaluate content validity and reliability. All statistical analyses were conducted using the Statistical Package for Social Sciences (SPSS), version 17, developed by SPSS Inc., USA, for Microsoft Windows. A p-value of less than 0.05 was considered statistically significant.
Results
The needs assessment revealed significant gaps in students' knowledge, attitudes, and practices regarding CBE. Knowledge scores were notably low (4.4 ± 1.2 out of 9), with a high frequency of “Not sure” responses, particularly in areas such as competency-based assessments, self-directed learning strategies, and group dynamics. More than 60% of students were unfamiliar with the flipped classroom model, and over 65% lacked awareness of formative assessments and their role in CBME.
Attitude scores were also suboptimal (6.2 ± 0.8 out of 15), with the majority of students selecting “Neither agree nor disagree” or lower, indicating uncertainty about CBME’s effectiveness. Notably, only 28% of students agreed that CBME adequately prepares them for real-world medical practice, while 35% expressed concerns about their ability to engage in self-directed learning.
Practices related to CBE were infrequent, as reflected in the predominance of “Rarely” and “Never” responses across the 12 practice items, with an overall practice score of 5.3 ± 1.1. Only 22% of students reported regularly engaging in self-directed learning, and fewer than 30% had experience with structured reflection sessions, which are integral to CBME. These findings highlight a critical need for targeted interventions to enhance students’ understanding, foster more positive attitudes, and improve their practical engagement with CBME principles (Figure 2).
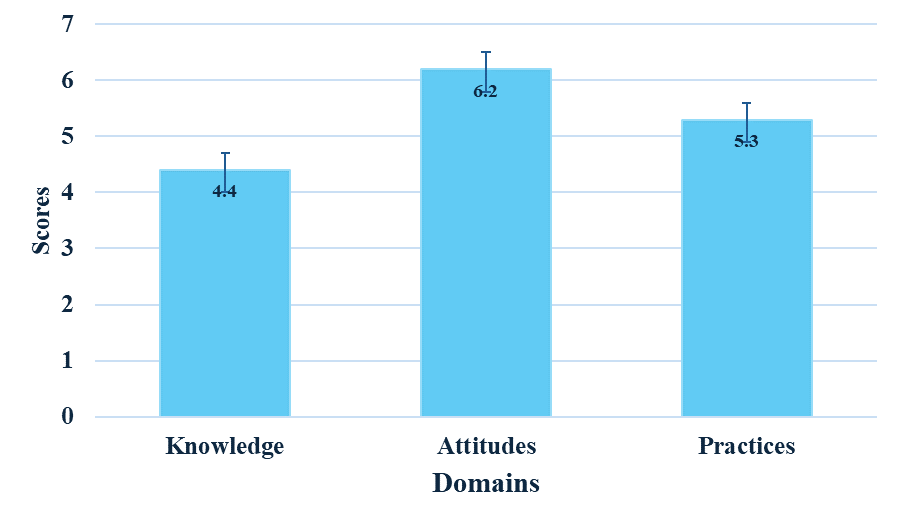
Figure 2. Needs assessment revealing knowledge, attitudes, and practices of first-year medical students
This figure presents baseline scores showing low knowledge (4.4), moderate attitudes (6.2), and limited practices (5.3) in Competency-Based Medical Education (CBME).
The module demonstrated high validity and reliability, confirming its effectiveness as a structured orientation tool for CBME. Face validity yielded an average evaluation score of 0.97 ± 0.048, reflecting strong agreement among experts regarding the module’s clarity, relevance, and usability.
Content validity results were equally strong, with an I-CVI of 0.97 ± 0.048 and a S-CVI/UA of 0.95 ± 0.046, confirming that the module comprehensively covers essential CBME components.
Reliability assessment yielded an ICC of 0.87, indicating strong internal consistency and reproducibility across different evaluators. Pre-test results, measured with 25 scenario-based multiple-choice questions, showed an average score of 8.0 ± 2.1, indicating limited initial comprehension of CBME concepts and their application in clinical and educational settings. Students particularly struggled with competency mapping, Entrustable Professional Activities (EPAs), and self-directed learning principles, where over 65% of responses were incorrect.
Following two weeks of module engagement, post-test scores improved significantly to an average of 21.2 ± 1.8, with a statistically significant difference (p < 0.0001).
The highest improvements were observed in applying competency-based assessment principles (average score increase of 64%) and understanding self-directed learning strategies (increase of 58%). These results suggest that the module was effective in enhancing students’ ability to apply CBME concepts in a structured and meaningful manner.
Feedback on the module was collected using a 9-item questionnaire rated on a 10-point scale, providing insights into its clarity, relevance, and practical value. Students expressed high satisfaction, with ratings consistently above 9.4 across all parameters (Figure 3). Specifically, 95% of students reported that the module effectively clarified CBME principles and their role in medical education. Additionally, 92% of students found the reflective exercises particularly useful in helping them internalize competency-based learning concepts, while 94% agreed that the module provided actionable strategies for transitioning into CBME.
Overall, the results indicate that the START CBME module significantly improved students’ knowledge, attitudes, and practical engagement with CBME, effectively addressing the gaps identified in the needs assessment.
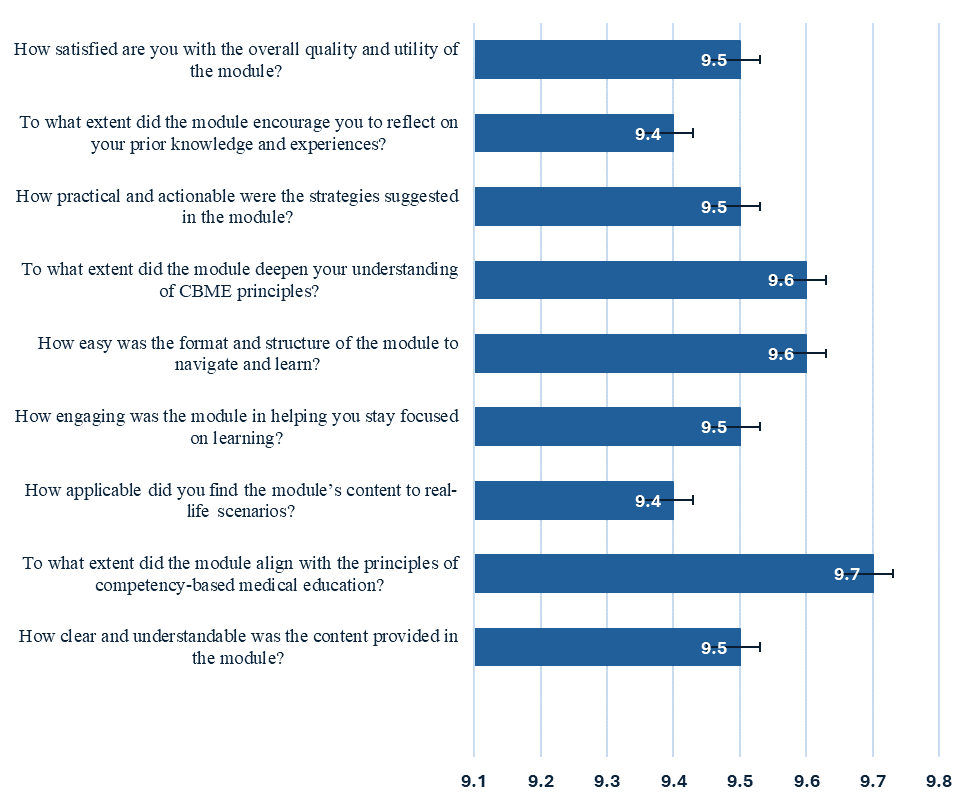
Figure 3. Students’ feedback about the START CBME module
This figure presents students’ high satisfaction regarding the module’s clarity, structure, engagement, applicability, and alignment with CBME principles.
This figure presents students’ high satisfaction regarding the module’s clarity, structure, engagement, applicability, and alignment with CBME principles.
Discussion
The shift to CBME is equally challenging for medical students. The transition is not just about mastering content but clearly understanding the purpose and relevance behind each component of CBME such that they are guided in an informed and responsible way. Studies conducted previously have explored students’ positive perceptions towards CBME through faculty-driven and curriculum-based implementations [18, 19]. However, students’ ability to comprehend the meaning behind each component is not well studied. A study conducted in an Indian medical school found that while students appreciated the emphasis on competencies, many struggled with self-directed learning and competency-based assessments due to a lack of structured orientation at the beginning of their medical education [20]. Similar concerns have been reported in studies from the UK and Canada, where students transitioning into CBME expressed difficulty in adapting to entrustable professional activities and formative assessments without early guidance [21, 22].
The introduction of START CBME module stands as a critical need for first professional medical students to get acquainted about CBME. The module has been validated
for its content with high reliability scores. By embedding reflective exercises and aligning content with the NMC’s revised guidelines, the module not only addresses knowledge deficits but also fosters a proactive learning mindset among students [23]. Compared to other CBME orientation programs, START CBME distinguishes itself by integrating constructivist learning principles with competency mapping exercises, a feature lacking in traditional foundation courses offered in Indian medical colleges. An analysis of early CBME sensitization programs in Singapore suggests that incorporating structured self-reflection significantly enhances student engagement with competency-based frameworks [24]. The strong post-test gains observed in this study align with these international findings, reinforcing the importance of reflective learning in medical education.
The significant gains in post-test scores, coupled with positive feedback on module clarity and relevance, highlight the importance of familiarizing students with CBME principles from the onset of their medical education. The improvement in self-directed learning scores is particularly noteworthy, as previous studies have reported that Indian medical students often struggle with autonomous learning due to a predominantly teacher-driven pre-university education [25]. Addressing this gap early may improve students’ adaptability and engagement in competency-based curricula.
Furthermore, the structured, outcome-based approach of START CBME supports students in transitioning from passive learning to an active, self-directed educational model.
This shift is essential in preparing future physicians who are adaptable, skilled, and committed to continuous professional development [26]. In the context of CBME implementation in India, these findings suggest that early exposure to competency-based learning frameworks should become a standardized component of the medical curriculum [27]. Faculty development efforts have primarily focused on training educators in CBME principles, but student sensitization remains an overlooked aspect [28]. Integrating structured CBME orientation modules within the foundation course could address this issue, ensuring that students and faculty progress toward competency-based learning with shared expectations.
Despite these strengths, this study has some limitations. The pilot test was conducted with a relatively small sample of 24 students, which may limit the generalizability of the findings. Additionally, as this was a single-institution study, variations in curriculum delivery and institutional support structures in other medical schools may influence the effectiveness of the module in different settings. Future research should expand the sample size and evaluate the module’s impact across multiple institutions to ensure its broader applicability. Longitudinal studies assessing the retention of CBME concepts and their influence on student performance in later academic years would provide valuable insights into the long-term effectiveness of CBME sensitization.
Future research should also explore the long-term impact of CBME orientation modules on clinical performance, assessment scores, and professional development. A mixed-methods approach incorporating qualitative feedback from students and faculty could provide deeper insights into the challenges and benefits of CBME sensitization. Furthermore, the integration of technology-enhanced learning tools could be investigated to enhance the effectiveness of competency-based training.
The module’s design and outcomes could serve as a model for other institutions aiming to enhance CBME comprehension and engagement, contributing to the broader goal of quality-driven medical education in India. As competency-based education continues to evolve, early sensitization programs such as START CBME could play a pivotal role in bridging the gap between traditional medical training and outcome-driven learning, ultimately shaping more competent and self-directed healthcare professionals.
Conclusion
The START CBME module provides a structured and reflective approach to bridging the transition from traditional learning to competency-based medical education for first-year students. By introducing CBME principles early, the module enhances student understanding, fosters self-directed learning, and improves engagement with competency-based training. The significant gains in knowledge, attitudes, and practical application of CBME concepts highlight its effectiveness in addressing the initial challenges students face in adapting to this educational model. These findings underscore the importance of structured CBME sensitization programs in fostering adaptability, critical thinking, and professional responsibility among medical students.
As competency-based education becomes the standard in medical training, this module can serve as a model for institutions aiming to strengthen student readiness, ensuring a smoother transition into CBME and promoting lifelong learning habits essential for future healthcare professionals.
Ethical considerations
This study was approved by the Institutional Human Ethics Committee of Panimalar Medical College Hospital & Research Institute, PMCH&RI/IHEC/2024/202, Dated: 06/08/2024. All data collected was used only for research purpose and confidentiality was maintained throughout the study.
Artificial intelligence utilization for article writing
No artificial intelligence (AI) tools were used for the writing of this article
Acknowledgment
None to be acknowledged.
Conflict of interest statement
None to be declared.
Author contributions
Conceptualization: KMS; Methodology: KMS; Software: KMS; Validation: KMS; Formal analysis: KMS; Investigation: KMS; Resources: KMS; Data curation: KMS; Writing—original draft preparation: KMS; Writing—review and editing: KMS; Visualization: KMS; Supervision: KMS; Project administration: KMS; and Funding acquisition: KMS. All authors have read and agreed to the published version of the manuscript.
Funding
None to be declared
Data availability statement
All information is available in the article.
Article Type : Short Communication |
Subject:
Medical Education
Received: 2025/01/10 | Accepted: 2025/07/21 | Published: 2025/10/1
Received: 2025/01/10 | Accepted: 2025/07/21 | Published: 2025/10/1
References
1. National Medical Commission. UG Curriculum [Internet]. NMC. Available from: [cited 2024 Aug 14].
2. Rege N. Towards competency-based learning in medical education: building evidence in India. J Postgrad Med. 2020;66(1):9-10. [DOI:10.4103/jpgm.JPGM_749_19] [PMID] []
3. Alharbi NS. Evaluating competency-based medical education: a systematized review of current practices.
4. BMC Med Educ. 2024;24(1):612.
5. Levine MF, Shorten G. Competency-based medical education: its time has arrived. Can J Anaesth. 2016;63(7):802-6. [DOI:10.1007/s12630-016-0638-6] [PMID]
6. Ryan MS, Blood AD, Park YS, Farnan JM. Competency-based frameworks in medical school education programs: a thematic analysis of the academic medicine snapshots, 2020. Acad Med. 2022;97(11S):S63-S70. [DOI:10.1097/ACM.0000000000004912] [PMID]
7. Whitcomb ME. More on competency-based education. Acad Med. 2004;79(6):493-4. [DOI:10.1097/00001888-200406000-00001] [PMID]
8. Whitcomb ME. Finding ways to close the gap. Acad Med. 2004;79(8):719-20. [DOI:10.1097/00001888-200408000-00001] [PMID]
9. Sirianni G, Glover Takahashi S, Myers J. Taking stock of what is known about faculty development in competency-based medical education: a scoping review paper. Med Teach. 2020;42(8):909-15. [DOI:10.1080/0142159X.2020.1763285] [PMID]
10. Mahajan R, Virk A, Saiyad S, Shah N, Kahar P, Sharma A, et al. Stages of concern of medical faculty toward adoption of competency-based medical education in India: a multicentric survey. Int J Appl Basic Med Res. 2022;12(2):87-94. [DOI:10.4103/ijabmr.ijabmr_816_21] [PMID] []
11. Soundariya K, Kalaiselvan G, Rajalakshmi M, Sindhuri R. Implementation and evaluation of competency-based medical education in phase I of undergraduate medical curriculum. J Adv Med Educ Prof. 2022;10(4):228-34.
12. Davis MH, Harden RM. Planning and implementing an undergraduate medical curriculum: the lessons learned. Med Teach. 2003;25(6):596-608. [DOI:10.1080/0142159032000144383] [PMID]
13. Surapaneni KM. START CBME: Sensitization and Training for Adapting to the Requirements of Transition in Competency Based Medical Education [Preprint] [Internet]. figshare. 2024. Available from: [cited 2025 Jul 21].
14. Kim S, Kyung SY, Park IB, Yune SJ, Park KH. The effectiveness of competency-based global health education programs for medical students. Korean J Med Educ. 2024;36(3):243-54. [DOI:10.3946/kjme.2024.299] [PMID] []
15. Romanova A, Touchie C, Ruller S, Kaka S, Moschella A, Zucker M, et al. Learning plan use in undergraduate medical education: a scoping review. Acad Med. 2024;99(9):1038-45. [DOI:10.1097/ACM.0000000000005781] [PMID]
16. Holmboe ES, Sherbino J, Englander R, Snell L, Frank JR, Icbme Collaborators. A call to action: the controversy of and rationale for competency-based medical education. Med Teach. 2017;39(6):574-81. [DOI:10.1080/0142159X.2017.1315067] [PMID]
17. Ten Cate O, Billett S. Competency‐based medical education: origins, perspectives and potentialities. Med Educ. 2014;48(3):325-32. [DOI:10.1111/medu.12355] [PMID]
18. Sharma S, Chhatwal J. Perspectives of undergraduate medical students regarding competency-based curriculum. Natl Med J India. 2023;36(6):379-83. [DOI:10.25259/NMJI_461_2022] [PMID]
19. Sulena S, Kulkarni A, Mathur M, Jyoti N, Sidhu TK, Badyal D, et al. Challenges in implementing competency-based medical education in India-stakeholders' perspective: a mixed-method analysis. Int J Appl Basic Med Res. 2024;14(3):141-8. [DOI:10.4103/ijabmr.ijabmr_268_24] [PMID] []
20. Kar SK. Competency-based medical education in India: barriers in implementation in psychiatry. Odisha J Psychiatry. 2022;18(2):65-6. [DOI:10.4103/OJP.OJP_5_23]
21. Gopalakrishnan S, Catherine AP, Kandasamy S, Ganesan H. Challenges and opportunities in the implementation of competency-based medical education-a cross-sectional survey among medical faculty in India. J Educ Health Promot. 2022;11:206. [DOI:10.4103/jehp.jehp_1130_21] [PMID] []
22. Lockyer J, Bursey F, Richardson D, Frank JR, Snell L, Campbell C, et al. Competency-based medical education and continuing professional development: a conceptualization for change. Med Teach. 2017;39(6):617-22. [DOI:10.1080/0142159X.2017.1315064] [PMID]
23. Crawford L, Cofie N, Mcewen L, Dagnone D, Taylor SW. Perceptions and barriers to competency‐based education in Canadian postgraduate medical education. J Eval Clin Pract. 2020;26(4):1124-31. [DOI:10.1111/jep.13371] [PMID]
24. Shah N, Desai C, Jorwekar G, Badyal D, Singh T. Competency-based medical education: an overview and application in pharmacology. Indian J Pharmacol. 2016;48(Suppl 1):S5-S12. [DOI:10.4103/0253-7613.193312] [PMID] []
25. Macneill P, Joseph R, Lysaght T, Samarasekera DD, Hooi SC. A professionalism program in medical education and training-from broad values to specific applications: YLL School of Medicine, Singapore. Med Teach. 2020;42(5):561-71. [DOI:10.1080/0142159X.2020.1714021] [PMID]
26. Boyd VA, Whitehead CR, Thille P, Ginsburg S, Brydges R, Kuper A. Competency‐based medical education: the discourse of infallibility. Med Educ. 2018;52(1):45-57. [DOI:10.1111/medu.13467] [PMID]
27. Anusha G, Nagaraj C, Shobhitha D, Anil R. Readiness of medical students for self-directed learning under competency based medical education-a cross-sectional study. APIK J Int Med. 2023;11(3):156-60.
28. Shrivastava SR, Shrivastava PS. How to successfully implement competency-based medical education in India. Educ Health Prof. 2018;1(2):61-3. [DOI:10.4103/EHP.EHP_20_18]
29. Bansal P, Supe A, Sahoo S, Vyas R. Faculty development for competency based medical education: global, national and regional perspectives. Natl J Integr Res Med. 2017;8(5):1-6.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




