Sat, Jan 31, 2026
[Archive]
Volume 18, Issue 1 (2025)
J Med Edu Dev 2025, 18(1): 140-146 |
Back to browse issues page
Ethics code: SS2024REC-014
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hu H, Hashim H, Li X. Bridging language and learning: A CLIL-ized TMI model for international students in traditional Chinese medicine. J Med Edu Dev 2025; 18 (1) :140-146
URL: http://edujournal.zums.ac.ir/article-1-2358-en.html
URL: http://edujournal.zums.ac.ir/article-1-2358-en.html
1- Faculty of Education, Universiti Kebangsaan Malaysia, Bangi, Malaysia , p108937@siswa.ukm.edu.my
2- Faculty of Education, Universiti Kebangsaan Malaysia, Bangi, Malaysia. University Research Group on Eduxcellence: Development of Innovative Curriculum & Pedagogy, Universiti Kebangsaan Malaysia, Bangi, Malaysia
3- School of Traditional Chinese Medicine, Shandong Second Medical University, Weifang, China
2- Faculty of Education, Universiti Kebangsaan Malaysia, Bangi, Malaysia. University Research Group on Eduxcellence: Development of Innovative Curriculum & Pedagogy, Universiti Kebangsaan Malaysia, Bangi, Malaysia
3- School of Traditional Chinese Medicine, Shandong Second Medical University, Weifang, China
Full-Text [PDF 753 kb]
(630 Downloads)
| Abstract (HTML) (1099 Views)
Full-Text: (261 Views)
Abstract
Background & Objective: The increasing number of international students studying Traditional Chinese Medicine (TCM) in China has brought to light challenges related to the linguistic complexity and specialized terminology of TCM courses, which are primarily conducted in Chinese or English. This Short Communication paper presents an innovative teaching model that combines language instruction with subject-specific content to address these challenges.
Materials & Methods: The model was implemented with 128 international students at a Chinese university. Data collection involved tests assessing English and Chinese language skills, TCM knowledge, and student satisfaction through a questionnaire.
Results: Students showed significant improvements in language proficiency and TCM knowledge. Responses from the questionnaires indicated high levels of satisfaction, with participants noting advancements in their linguistic skills, mastery of content, and cultural understanding.
Conclusion: Integrating language support into subject-specific teaching effectively addresses challenges in international TCM education, offering a replicable model for similar contexts.
Introduction
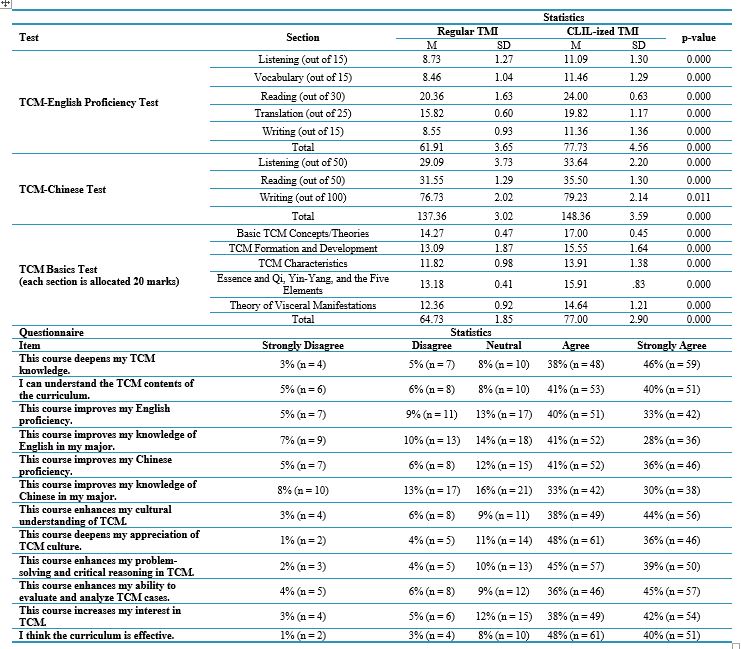
Table 1. Results of CLIL-ized TMI implementation
CLIL-ized TMI provides a practical solution for improving medical education for international students by addressing the dual challenge of mastering complex medical content while developing proficiency in the language of instruction. This approach facilitates students’ acquisition of specialized medical knowledge while improving their language skills, cultural understanding, and critical thinking—skills essential for effective global medical practice. However, scaling up the CLIL-ized TMI model necessitates careful planning and execution. Institutions must go beyond adding language support to content teaching and undertake a systematic redesign of their educational frameworks. Medical educators need specialized training to seamlessly integrate medical content with TL instruction, supported by institutional investments in resources such as bilingual glossaries and customized textbooks. Collaboration between medical and language experts is essential to ensure that instruction aligns with both the linguistic and professional needs of students. Implementing CLIL-ized TMI demands a shift in pedagogy to prepare students not just for academic achievement but for meaningful contributions to the global healthcare field.
Despite its promising outcomes, the implementation of CLIL-ized TMI presents certain limitations. The study was conducted at a single Chinese university, limiting the generalizability of findings to institutions with different student demographics, curricular structures, and teaching resources. Future research should examine its applicability across diverse educational settings, including those with varying levels of English and Chinese language support. Comparative studies across disciplines such as Western medicine, pharmacy, and nursing could further refine the model to better meet the needs of various professional fields. Additionally, while this study relied on quantitative assessments and student perceptions, it did not include direct classroom observations or qualitative insights from instructors. Future research should integrate classroom discourse analysis, instructor reflections, and case studies to achieve a deeper understanding of the teaching and learning dynamics within the CLIL-ized TMI model. Longitudinal studies evaluating the long-term impact on students’ professional and linguistic development would also yield valuable insights. Finally, effective implementation requires institutional support, including well-trained educators, sufficient teaching materials, and ongoing professional development. Establishing interdisciplinary collaboration between medical and language educators, developing standardized bilingual resources, and integrating CLIL methodologies into national education policies are essential for sustaining and scaling this approach in international TCM education.
Ethical considerations
Ethical approval was obtained from the Research Ethics Committee of Shandong Second Medical University (Ethics Code: SS2024REC-014), and informed consent was gathered from all participants in the study.
Artificial intelligence utilization for article writing
No generative artificial intelligence tools were utilized in the conceptualization, drafting, or editing of this manuscript. All content, including the analysis, interpretation, and writing, was exclusively created by the authors. Standard proofreading tools were used for grammar and formatting checks.
Acknowledgment
The research was funded by the Faculty of Education, Universiti Kebangsaan Malaysia, with the grant code GG-2024-030.
Conflict of interest statement
The authors declared no conflicts of interest.
Author contributions
Hu H conceptualized the study, designed the methodology, collected and analyzed the data, and drafted the initial manuscript. Hashim H provided critical revisions, supervised the study, and contributed to the refinement of the research framework. Li X assisted in data interpretation, literature review, and manuscript editing. All authors reviewed and approved the final version of the manuscript.
Funding & Supporting resources
This study received assistance from the Faculty of Education, Universiti Kebangsaan Malaysia, and the School of Traditional Chinese Medicine, Shandong Second Medical University. The funding body had no role in the study design, data collection, analysis, interpretation, or manuscript writing.
Data availability statement
The data used in the study are available from the corresponding author upon reasonable request.
Background & Objective: The increasing number of international students studying Traditional Chinese Medicine (TCM) in China has brought to light challenges related to the linguistic complexity and specialized terminology of TCM courses, which are primarily conducted in Chinese or English. This Short Communication paper presents an innovative teaching model that combines language instruction with subject-specific content to address these challenges.
Materials & Methods: The model was implemented with 128 international students at a Chinese university. Data collection involved tests assessing English and Chinese language skills, TCM knowledge, and student satisfaction through a questionnaire.
Results: Students showed significant improvements in language proficiency and TCM knowledge. Responses from the questionnaires indicated high levels of satisfaction, with participants noting advancements in their linguistic skills, mastery of content, and cultural understanding.
Conclusion: Integrating language support into subject-specific teaching effectively addresses challenges in international TCM education, offering a replicable model for similar contexts.
Introduction
The globalization of higher education has led to a notable increase in the enrollment of international students in Traditional Chinese Medicine (TCM) programs in China, primarily from Asia and Africa [1]. TCM is a medical discipline that encompasses herbal medicine, acupuncture, massage, and various traditional healing practices. Mastery of this field often requires specialized knowledge that differs from that of modern Western medicine [2]. In Chinese higher education, TCM courses are generally taught in either Chinese or English as the lingua franca. However, the medical terminology and discipline-specific language used in these courses can be complex and quite different from everyday Chinese or English. This presents significant challenges for students who are non-native speakers of either language, affecting their ability to comprehend specialized content, engage in critical thinking, and develop a nuanced cultural understanding of TCM [3, 4]. To address these linguistic and cognitive barriers, we developed and implemented a pedagogical model that integrates Content and Language Integrated Learning (CLIL) with Target-Language-Medium Instruction (TMI). This CLIL-based TMI model is specifically designed to improve international students’ understanding of TCM by simultaneously enhancing their medical knowledge and language proficiency within a structured and supportive learning environment.
Materials & Methods
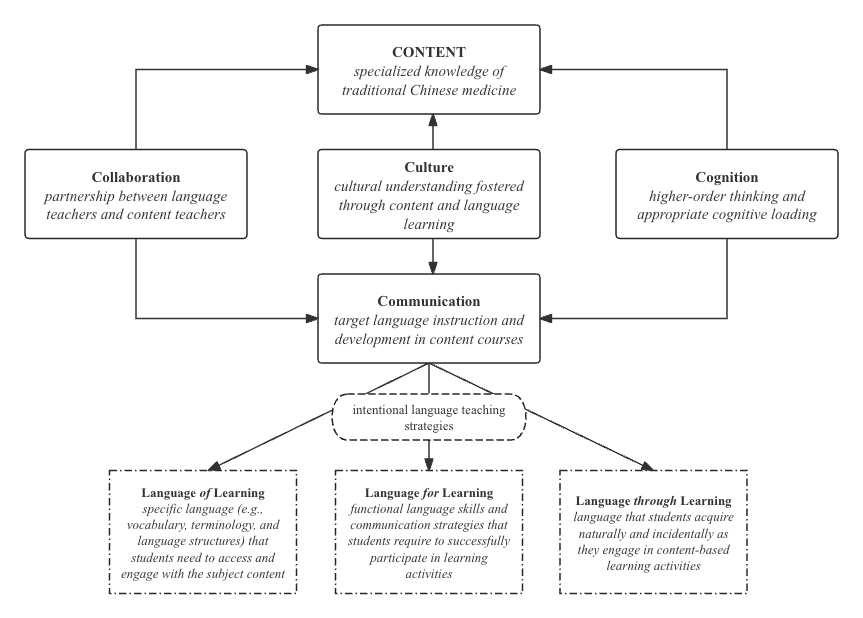
CLIL, or Content and Language Integrated Learning, is a pedagogical approach that combines content and language learning, allowing students to enhance their subject-specific knowledge and Foreign Language (L2) proficiency while also promoting cultural awareness and cognitive development. TMI, or Target Language Instruction, refers to using a target language (usually the students’ L2) to teach academic subjects other than the language itself [5]. In this context, we adopted a CLIL-ized TMI approach to enrich traditional TMI—which typically focuses exclusively on content learning in the students’ L2—by incorporating intentional language instruction. The CLIL-ized TMI model (Figure 1) is built upon five core principles in TCM learning:
Materials & Methods
CLIL, or Content and Language Integrated Learning, is a pedagogical approach that combines content and language learning, allowing students to enhance their subject-specific knowledge and Foreign Language (L2) proficiency while also promoting cultural awareness and cognitive development. TMI, or Target Language Instruction, refers to using a target language (usually the students’ L2) to teach academic subjects other than the language itself [5]. In this context, we adopted a CLIL-ized TMI approach to enrich traditional TMI—which typically focuses exclusively on content learning in the students’ L2—by incorporating intentional language instruction. The CLIL-ized TMI model (Figure 1) is built upon five core principles in TCM learning:
Figure 1. CLIL-ized EMI model for TCM teaching
Content
Content principle emphasizes delivering accurate and comprehensive subject knowledge in TCM, ensuring that students understand key medical concepts and practices. It reflects the subject-knowledge-oriented nature of CLIL-ized TMI, with content mastery remaining the primary focus [6]. Lessons are designed to systematically introduce foundational theories of TCM while gradually incorporating complex concepts, allowing students to develop a robust understanding of traditional medical practices
Communication
Communication suggests providing intentional L2 language support during TCM instruction to facilitate content learning. The “language of learning” refers to the
specialized medical vocabulary and structures necessary to comprehend TCM content, while the “language for learning” encompasses the functional language needed for discussions, report writing, and explaining medical concepts. Both aspects are explicitly addressed in the curriculum. By implementing vocabulary pre-teaching, scaffolding complex terminology, and modeling key Target Language (TL) structures, students enhance their linguistic accuracy and fluency in medical discourse. As a result, language through learning is fostered [7], meaning students naturally acquire linguistic competence as they interact with authentic TCM materials and apply medical concepts in real-world scenarios.
Collaboration
Collaboration emphasizes the partnership between TCM teachers and language instructors to address the linguistic needs of international students effectively. While TCM instructors are experts in their field, they may not always be prepared to teach language explicitly. As a result, language teachers play a crucial role in identifying the specific linguistic challenges that students encounter and in integrating appropriate language support within specialized courses [8]. This interdisciplinary collaboration strengthens instructional quality and ensures that both content and language objectives are met.
Culture
Culture highlights the importance of fostering students’ appreciation of the historical, philosophical, and cultural underpinnings of TCM. Given that TCM is deeply rooted in Chinese history and philosophy, understanding the cultural context is essential for grasping its principles [2]. This principle is operationalized by incorporating discussions about cultural traditions, historical evolution, and the philosophical foundations of TCM into the curriculum. By connecting TCM content with L2 communication, students not only enhance their linguistic competence but also cultivate a deeper appreciation for the sociocultural dimensions of traditional medicine.
Cognition
Cognition underlines the promotion of higher-order thinking skills while supporting students in managing the cognitive demands of learning both TCM content and L2(s). CLIL-ized TMI fosters critical thinking by encouraging students to analyze medical texts, compare different treatment philosophies, and engage in problem-solving activities. Given the dual challenge of acquiring medical knowledge while mastering an additional language, instructional scaffolding is implemented to help students manage cognitive load effectively [9, 10]. Lessons include structured discussions, case analyses, and inquiry-based learning tasks to enhance students' ability to apply theoretical knowledge to practical medical scenarios. By synthesizing these five principles, CLIL-ized TMI creates a comprehensive, interactive, and student-centered learning environment that enhances both subject-specific knowledge and language proficiency. This integrated approach equips students with linguistic and cognitive skills necessary for academic success, professional communication, and clinical practice in multicultural healthcare settings.
Implementation
We implemented CLIL-ized TMI at a Chinese university with 128 freshmen, aged 20–22, from diverse backgrounds, including Pakistan (n = 35), Kazakhstan (n = 22), Nigeria (n = 30), Ghana (n = 20), and Kenya (n = 21). They were enrolled in four TCM classes selected based on the following criteria: (1) enrollment in the university’s English-medium TCM program, (2) willingness to participate in the study with informed consent, (3) completion of a pre-assessment on language proficiency and prior knowledge of TCM, and (4) representation of diverse linguistic and cultural backgrounds to ensure a comprehensive understanding of varied learning needs. The implementation lasted one academic semester and focused on foundational knowledge of TCM. The learners’ English proficiency was assessed at the B1-B2 level according to the Common European Framework of Reference for Languages scale, an international standard for describing L2 ability. Their Chinese proficiency corresponded to Level 4 on the Chinese Proficiency Test (Hanyu Shuiping Kaoshi, HSK), China’s standardized assessment for non-native speakers of Standard Chinese, indicating a moderate level of TL proficiency. Additionally, we involved another cohort with a similar composition and comparable levels of TL and TCM content proficiency, which received regular TMI. The control group consisted of 123 freshmen from Pakistan (n = 30), Kazakhstan (n = 25), Nigeria (n = 25), Ghana (n = 24), and Kenya (n = 19), all of whom had the same level of English and Chinese proficiency and TCM content knowledge as the CLIL-ized TMI group. However, the instruction for this group followed a conventional TMI approach, in which content delivery prioritized subject matter without explicit language support. Unlike the CLIL-ized TMI group, students in this control group relied solely on traditional lectures and direct instruction and were expected to independently navigate the linguistic challenges associated with learning TCM in English or Chinese, without the benefit of structured scaffolding or language-focused interventions. Both groups were taught by the same instructor, who had extensive experience teaching TCM to international students. They followed the same curriculum and used identical teaching materials, including prescribed bilingual textbooks, teacher-prepared handouts, and supplementary multimedia resources. We administered the TCM-English Proficiency Test, the TCM-Chinese Test, and the TCM Basics Test after the implementation to both the target student cohort (treatment group) and the control group. These tests were adapted from authentic standardized test batteries in China [11-13], with modifications made to align them with the Teaching objectives. Notably, the TCM Basics Test was administered in either Chinese or English, based on the students’ preferred language of competence, to ensure an accurate assessment of their content learning outcomes. Additionally, we distributed a questionnaire adapted from Sinaga and Maisarah [14] to assess students’ perceptions of CLIL-ized TMI. All instruments were reviewed by experts to ensure face validity, and a pilot study was conducted to confirm the test-retest reliability of the assessments and the internal consistency of the questionnaire.
Results
The collected data were analyzed using the Statistical Package for the Social Sciences for both descriptive and inferential analyses, with particular emphasis on between-group comparisons. An independent samples t-test was conducted to determine whether CLIL-ized TMI demonstrated superior effectiveness compared to regular TMI. The results (Table 1) indicate that the CLIL-ized TMI model was significantly more effective in improving student learning outcomes than regular TMI. Specifically, students in the CLIL-ized TMI group outperformed those in the regular TMI group in English listening (p < 0.001), vocabulary (p < 0.001), reading (p < 0.001), translation (p < 0.001), writing (p < 0.001), and overall proficiency (p < 0.001), demonstrating statistically significant differences across these language domains. Similarly, students receiving CLIL-ized TMI achieved higher scores in Chinese listening (p < 0.001), reading (p < 0.001), writing (p = 0.011), and overall proficiency (p < 0.001), indicating that the model had a substantial impact on improving students’ TL proficiency in both English and Chinese. In addition to linguistic gains, the CLIL-ized TMI group also exhibited superior content learning outcomes. They not only achieved higher overall scores in TCM fundamentals (p across multiple dimensions, including basic TCM concepts and theories (p < 0.001), TCM formation and < 0.001) but also demonstrated deeper comprehension development (p < 0.001), TCM characteristics (p < 0.001), essence and Qi, Yin-Yang and the five elements (p < 0.001), and the theory of visceral manifestations (p < 0.001). These findings highlight the dual benefits of CLIL-ized TMI and reinforce its potential to improve both language proficiency and subject knowledge acquisition in international TCM education.
The questionnaire results indicate strongly positive student perceptions of the CLIL-ized TMI model. A majority of students agreed or strongly agreed that the course deepened their TCM knowledge (84%), with 81% reporting an improved understanding of the curriculum content. These findings suggest that integrating language support with subject-specific instruction enhances students' ability to grasp complex medical concepts. Similarly, the CLIL-ized TMI model was seen as advantageous for language development, with 73% of students acknowledging improvements in their English proficiency and 69% reporting gains in their English knowledge related to their major. Additionally, 77% of students indicated enhanced proficiency in Chinese, underscoring the dual-language benefits of the model. Beyond linguistic and content knowledge, students also noted improvements in cultural awareness and cognitive skills. Approximately 82% of respondents felt the course enriched their cultural understanding of TCM, while 84% expressed a deeper appreciation of TCM culture. These findings underscore the model’s effectiveness in fostering not only linguistic and disciplinary learning but also cultural competence, a crucial aspect of studying traditional medicine. Furthermore, 84% of students agreed that the course enhanced their problem-solving and critical reasoning abilities, and 81% reported an improved ability to evaluate and analyze TCM cases. Finally, the high percentage of students (80%) who reported increased interest in TCM, along with the overall effectiveness of the curriculum (88%), suggests that the CLIL-ized TMI model plays a crucial role in enhancing learning motivation. Together, these results confirm that the model successfully integrates content mastery, language development, cultural awareness, and cognitive skills, making it a highly effective approach for international TCM education.
Content principle emphasizes delivering accurate and comprehensive subject knowledge in TCM, ensuring that students understand key medical concepts and practices. It reflects the subject-knowledge-oriented nature of CLIL-ized TMI, with content mastery remaining the primary focus [6]. Lessons are designed to systematically introduce foundational theories of TCM while gradually incorporating complex concepts, allowing students to develop a robust understanding of traditional medical practices
Communication
Communication suggests providing intentional L2 language support during TCM instruction to facilitate content learning. The “language of learning” refers to the
specialized medical vocabulary and structures necessary to comprehend TCM content, while the “language for learning” encompasses the functional language needed for discussions, report writing, and explaining medical concepts. Both aspects are explicitly addressed in the curriculum. By implementing vocabulary pre-teaching, scaffolding complex terminology, and modeling key Target Language (TL) structures, students enhance their linguistic accuracy and fluency in medical discourse. As a result, language through learning is fostered [7], meaning students naturally acquire linguistic competence as they interact with authentic TCM materials and apply medical concepts in real-world scenarios.
Collaboration
Collaboration emphasizes the partnership between TCM teachers and language instructors to address the linguistic needs of international students effectively. While TCM instructors are experts in their field, they may not always be prepared to teach language explicitly. As a result, language teachers play a crucial role in identifying the specific linguistic challenges that students encounter and in integrating appropriate language support within specialized courses [8]. This interdisciplinary collaboration strengthens instructional quality and ensures that both content and language objectives are met.
Culture
Culture highlights the importance of fostering students’ appreciation of the historical, philosophical, and cultural underpinnings of TCM. Given that TCM is deeply rooted in Chinese history and philosophy, understanding the cultural context is essential for grasping its principles [2]. This principle is operationalized by incorporating discussions about cultural traditions, historical evolution, and the philosophical foundations of TCM into the curriculum. By connecting TCM content with L2 communication, students not only enhance their linguistic competence but also cultivate a deeper appreciation for the sociocultural dimensions of traditional medicine.
Cognition
Cognition underlines the promotion of higher-order thinking skills while supporting students in managing the cognitive demands of learning both TCM content and L2(s). CLIL-ized TMI fosters critical thinking by encouraging students to analyze medical texts, compare different treatment philosophies, and engage in problem-solving activities. Given the dual challenge of acquiring medical knowledge while mastering an additional language, instructional scaffolding is implemented to help students manage cognitive load effectively [9, 10]. Lessons include structured discussions, case analyses, and inquiry-based learning tasks to enhance students' ability to apply theoretical knowledge to practical medical scenarios. By synthesizing these five principles, CLIL-ized TMI creates a comprehensive, interactive, and student-centered learning environment that enhances both subject-specific knowledge and language proficiency. This integrated approach equips students with linguistic and cognitive skills necessary for academic success, professional communication, and clinical practice in multicultural healthcare settings.
Implementation
We implemented CLIL-ized TMI at a Chinese university with 128 freshmen, aged 20–22, from diverse backgrounds, including Pakistan (n = 35), Kazakhstan (n = 22), Nigeria (n = 30), Ghana (n = 20), and Kenya (n = 21). They were enrolled in four TCM classes selected based on the following criteria: (1) enrollment in the university’s English-medium TCM program, (2) willingness to participate in the study with informed consent, (3) completion of a pre-assessment on language proficiency and prior knowledge of TCM, and (4) representation of diverse linguistic and cultural backgrounds to ensure a comprehensive understanding of varied learning needs. The implementation lasted one academic semester and focused on foundational knowledge of TCM. The learners’ English proficiency was assessed at the B1-B2 level according to the Common European Framework of Reference for Languages scale, an international standard for describing L2 ability. Their Chinese proficiency corresponded to Level 4 on the Chinese Proficiency Test (Hanyu Shuiping Kaoshi, HSK), China’s standardized assessment for non-native speakers of Standard Chinese, indicating a moderate level of TL proficiency. Additionally, we involved another cohort with a similar composition and comparable levels of TL and TCM content proficiency, which received regular TMI. The control group consisted of 123 freshmen from Pakistan (n = 30), Kazakhstan (n = 25), Nigeria (n = 25), Ghana (n = 24), and Kenya (n = 19), all of whom had the same level of English and Chinese proficiency and TCM content knowledge as the CLIL-ized TMI group. However, the instruction for this group followed a conventional TMI approach, in which content delivery prioritized subject matter without explicit language support. Unlike the CLIL-ized TMI group, students in this control group relied solely on traditional lectures and direct instruction and were expected to independently navigate the linguistic challenges associated with learning TCM in English or Chinese, without the benefit of structured scaffolding or language-focused interventions. Both groups were taught by the same instructor, who had extensive experience teaching TCM to international students. They followed the same curriculum and used identical teaching materials, including prescribed bilingual textbooks, teacher-prepared handouts, and supplementary multimedia resources. We administered the TCM-English Proficiency Test, the TCM-Chinese Test, and the TCM Basics Test after the implementation to both the target student cohort (treatment group) and the control group. These tests were adapted from authentic standardized test batteries in China [11-13], with modifications made to align them with the Teaching objectives. Notably, the TCM Basics Test was administered in either Chinese or English, based on the students’ preferred language of competence, to ensure an accurate assessment of their content learning outcomes. Additionally, we distributed a questionnaire adapted from Sinaga and Maisarah [14] to assess students’ perceptions of CLIL-ized TMI. All instruments were reviewed by experts to ensure face validity, and a pilot study was conducted to confirm the test-retest reliability of the assessments and the internal consistency of the questionnaire.
Results
The collected data were analyzed using the Statistical Package for the Social Sciences for both descriptive and inferential analyses, with particular emphasis on between-group comparisons. An independent samples t-test was conducted to determine whether CLIL-ized TMI demonstrated superior effectiveness compared to regular TMI. The results (Table 1) indicate that the CLIL-ized TMI model was significantly more effective in improving student learning outcomes than regular TMI. Specifically, students in the CLIL-ized TMI group outperformed those in the regular TMI group in English listening (p < 0.001), vocabulary (p < 0.001), reading (p < 0.001), translation (p < 0.001), writing (p < 0.001), and overall proficiency (p < 0.001), demonstrating statistically significant differences across these language domains. Similarly, students receiving CLIL-ized TMI achieved higher scores in Chinese listening (p < 0.001), reading (p < 0.001), writing (p = 0.011), and overall proficiency (p < 0.001), indicating that the model had a substantial impact on improving students’ TL proficiency in both English and Chinese. In addition to linguistic gains, the CLIL-ized TMI group also exhibited superior content learning outcomes. They not only achieved higher overall scores in TCM fundamentals (p across multiple dimensions, including basic TCM concepts and theories (p < 0.001), TCM formation and < 0.001) but also demonstrated deeper comprehension development (p < 0.001), TCM characteristics (p < 0.001), essence and Qi, Yin-Yang and the five elements (p < 0.001), and the theory of visceral manifestations (p < 0.001). These findings highlight the dual benefits of CLIL-ized TMI and reinforce its potential to improve both language proficiency and subject knowledge acquisition in international TCM education.
The questionnaire results indicate strongly positive student perceptions of the CLIL-ized TMI model. A majority of students agreed or strongly agreed that the course deepened their TCM knowledge (84%), with 81% reporting an improved understanding of the curriculum content. These findings suggest that integrating language support with subject-specific instruction enhances students' ability to grasp complex medical concepts. Similarly, the CLIL-ized TMI model was seen as advantageous for language development, with 73% of students acknowledging improvements in their English proficiency and 69% reporting gains in their English knowledge related to their major. Additionally, 77% of students indicated enhanced proficiency in Chinese, underscoring the dual-language benefits of the model. Beyond linguistic and content knowledge, students also noted improvements in cultural awareness and cognitive skills. Approximately 82% of respondents felt the course enriched their cultural understanding of TCM, while 84% expressed a deeper appreciation of TCM culture. These findings underscore the model’s effectiveness in fostering not only linguistic and disciplinary learning but also cultural competence, a crucial aspect of studying traditional medicine. Furthermore, 84% of students agreed that the course enhanced their problem-solving and critical reasoning abilities, and 81% reported an improved ability to evaluate and analyze TCM cases. Finally, the high percentage of students (80%) who reported increased interest in TCM, along with the overall effectiveness of the curriculum (88%), suggests that the CLIL-ized TMI model plays a crucial role in enhancing learning motivation. Together, these results confirm that the model successfully integrates content mastery, language development, cultural awareness, and cognitive skills, making it a highly effective approach for international TCM education.
Table 1. Results of CLIL-ized TMI implementation
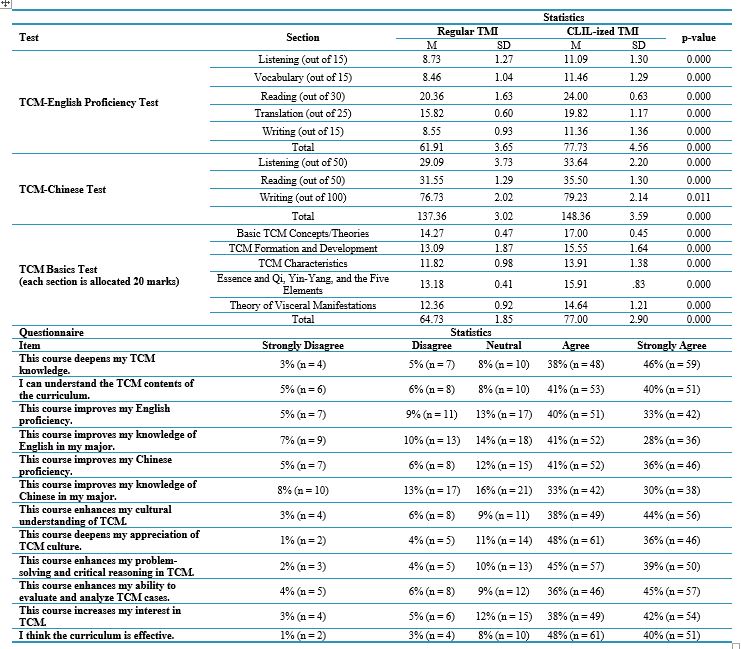
Note: Independent samples t-test was used to compare the effectiveness of CLIL-ized TMI and regular TMI across different test components.
Abbreviations: M, mean; SD, standard deviation; CLIL, content and language integrated learning; TMI, target-language-medium instruction; TCM, traditional Chinese medicine; p-value, Probability value; n, number of participants.
ConclusionAbbreviations: M, mean; SD, standard deviation; CLIL, content and language integrated learning; TMI, target-language-medium instruction; TCM, traditional Chinese medicine; p-value, Probability value; n, number of participants.
CLIL-ized TMI provides a practical solution for improving medical education for international students by addressing the dual challenge of mastering complex medical content while developing proficiency in the language of instruction. This approach facilitates students’ acquisition of specialized medical knowledge while improving their language skills, cultural understanding, and critical thinking—skills essential for effective global medical practice. However, scaling up the CLIL-ized TMI model necessitates careful planning and execution. Institutions must go beyond adding language support to content teaching and undertake a systematic redesign of their educational frameworks. Medical educators need specialized training to seamlessly integrate medical content with TL instruction, supported by institutional investments in resources such as bilingual glossaries and customized textbooks. Collaboration between medical and language experts is essential to ensure that instruction aligns with both the linguistic and professional needs of students. Implementing CLIL-ized TMI demands a shift in pedagogy to prepare students not just for academic achievement but for meaningful contributions to the global healthcare field.
Despite its promising outcomes, the implementation of CLIL-ized TMI presents certain limitations. The study was conducted at a single Chinese university, limiting the generalizability of findings to institutions with different student demographics, curricular structures, and teaching resources. Future research should examine its applicability across diverse educational settings, including those with varying levels of English and Chinese language support. Comparative studies across disciplines such as Western medicine, pharmacy, and nursing could further refine the model to better meet the needs of various professional fields. Additionally, while this study relied on quantitative assessments and student perceptions, it did not include direct classroom observations or qualitative insights from instructors. Future research should integrate classroom discourse analysis, instructor reflections, and case studies to achieve a deeper understanding of the teaching and learning dynamics within the CLIL-ized TMI model. Longitudinal studies evaluating the long-term impact on students’ professional and linguistic development would also yield valuable insights. Finally, effective implementation requires institutional support, including well-trained educators, sufficient teaching materials, and ongoing professional development. Establishing interdisciplinary collaboration between medical and language educators, developing standardized bilingual resources, and integrating CLIL methodologies into national education policies are essential for sustaining and scaling this approach in international TCM education.
Ethical considerations
Ethical approval was obtained from the Research Ethics Committee of Shandong Second Medical University (Ethics Code: SS2024REC-014), and informed consent was gathered from all participants in the study.
Artificial intelligence utilization for article writing
No generative artificial intelligence tools were utilized in the conceptualization, drafting, or editing of this manuscript. All content, including the analysis, interpretation, and writing, was exclusively created by the authors. Standard proofreading tools were used for grammar and formatting checks.
Acknowledgment
The research was funded by the Faculty of Education, Universiti Kebangsaan Malaysia, with the grant code GG-2024-030.
Conflict of interest statement
The authors declared no conflicts of interest.
Author contributions
Hu H conceptualized the study, designed the methodology, collected and analyzed the data, and drafted the initial manuscript. Hashim H provided critical revisions, supervised the study, and contributed to the refinement of the research framework. Li X assisted in data interpretation, literature review, and manuscript editing. All authors reviewed and approved the final version of the manuscript.
Funding & Supporting resources
This study received assistance from the Faculty of Education, Universiti Kebangsaan Malaysia, and the School of Traditional Chinese Medicine, Shandong Second Medical University. The funding body had no role in the study design, data collection, analysis, interpretation, or manuscript writing.
Data availability statement
The data used in the study are available from the corresponding author upon reasonable request.
Article Type : Orginal Research |
Subject:
Education
Received: 2024/12/11 | Accepted: 2025/04/5 | Published: 2025/04/14
Received: 2024/12/11 | Accepted: 2025/04/5 | Published: 2025/04/14
References
1. Zhang J, Zhou S, Pan H, Yan L, Rao Y, Liang S. Report on the preservation and innovation development of traditional Chinese medicine. 2023. [Online]. Available from: [Accessed on Oct. 23, 2024] [DOI]
2. Wang X, Ed. Chinese medicine. Beijing: People’s Medical Publishing House; 2021. [Online]. Available from: [Accessed on Oct. 15, 2024] [DOI]
3. . Xu J, Zhang T, Ge S, Zhang S. Research on the barriers and countermeasures in developing the international education of Chinese medicine. Curriculum and Teaching Methodology. 2021;4(1):32–37 [DOI]
4. Fan Y, Zhang S. Exploration on the construction of bilingual teacher development system for foreign students in university of traditional Chinese medicine based on the CLIL theory. Chinese Medicine Modern Distance Education of China. 2024;22(7):27-29 [DOI]
5. Vanisree M. New trends in English language teaching & learning. Bhopal: AGPH books; 2023
6. Hu H. Emerging from content and language integrated learning and English-medium instruction, is CLIL-ised EMI the next trend of education? Higher Learning Research Communications. 2023;13(2):1–8. [DOI]
7. Coyle D, Meyer O. Beyond CLIL: Pluriliteracies teaching for deeper learning. Cambridge: Cambridge University Press; 2021 [DOI]
8. Almushwat R, Elkout H. Language barriers in studying medicine in English: concerns and attitudes of clinical phase medical students at the University of Tripoli. AlQalam Journal of Medical and Applied Sciences. 2024;7(4):1022-1030 [DOI]
9. Zhou X. The exploration of CLIL teaching mode under the background of the reform of vocational education. Journal of Southern Vocational Education. 2020;10(5):84–89 [DOI]
10. Alimjanova LX, Nosirova UK. Content-based instruction in language teaching in relation with CLIL: implementation and outcome. Central Asian Research Journal for Interdisciplinary Studies. 2022;2(1):392-399 [DOI]
11. Ding N, Ed. TCM English proficiency test syllabus (trial) — with mock test papers. “Chinese Medicine English Proficiency Test” Project Preparatory Group. 2016. [Online]. Available from: [Accessed on Nov. 1, 2024] [DOI]
12. Center for Language Education and Cooperation, Chinese Testing International, Eds. The medical Chinese proficiency test (MCT). Beijing: Higher Education Press; 2020. [Online]. Available from: [Accessed on Nov. 2, 2024] [DOI]
13. Zheng H, Yang Z, Eds. Basic theory of traditional Chinese medicine exercises. Beijing: China Association of Chinese Medicine; 2022. [Online]. Available from: [Accessed on Oct. 28, 2024] [DOI]
14. Sinaga IRV, Maisarah I. EMI for international class: how do students perceive it? Journal of English for Specific Purposes in Indonesia. 2024;3(2):135–144. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |