Tue, Feb 24, 2026
[Archive]
Volume 18, Issue 2 (2025)
J Med Edu Dev 2025, 18(2): 30-38 |
Back to browse issues page
Ethics code: IR.BUMS.REC.1402.445
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abbasi R, Ghafari F, Farrahi R, Ram M, Mokhtari Seghaleh M. Evaluating the effect of hospital information system simulation-based training on nursing students' informatics skills before internship: A quasi-experimental study. J Med Edu Dev 2025; 18 (2) :30-38
URL: http://edujournal.zums.ac.ir/article-1-2326-en.html
URL: http://edujournal.zums.ac.ir/article-1-2326-en.html
1- Department of Health Information Technology, School of Paramedical Sciences, Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran
2- Department of Health Information Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran
3- Department of Health Information Technology, Ferdows Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran ,Farrahir1@gmail.com
4- Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran
5- MSc in Community Health Nursing, Rasul-e-Akram Hospital of Ferdows, Birjand University of Medical Sciences, Birjand, Iran. Email: maryammoktari3ghale@gmail.com. Phone: +985632720117
2- Department of Health Information Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran
3- Department of Health Information Technology, Ferdows Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran ,
4- Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran
5- MSc in Community Health Nursing, Rasul-e-Akram Hospital of Ferdows, Birjand University of Medical Sciences, Birjand, Iran. Email: maryammoktari3ghale@gmail.com. Phone: +985632720117
Full-Text [PDF 505 kb]
(587 Downloads)
| Abstract (HTML) (1523 Views)
Full-Text: (223 Views)
Abstract
Background & Objective: Educational simulators have been proposed as effective tools for enhancing learning and improving students' skills when preparing for the workplace. This study aimed to determine the effect of simulation-based training in a hospital information system on nursing students' informatics skills before their internship.
Materials & Methods: This quasi-experimental study was conducted in the first semester of the academic year (2023-2024) with 26 third-semester undergraduate nursing students at the Ferdows Faculty of Medical Sciences. The students were randomly divided into control and intervention groups. The educational content featured a simulation of the inpatient module of a hospital information system. Students in the intervention group were given access to this module's developed training and practice sections over two weeks. After one month, the test section for this module was made available to both the intervention and control groups. Data analysis was conducted using SPSS version 26, where descriptive statistics were calculated, and the Mann-Whitney test was utilized.
Results: After the test, the mean scores of students in the intervention and control groups were 35.69 ± 3.9 and 29.85 ± 5.01 (out of 41), respectively. The difference between the mean scores of the two groups was significant (p = 0.003, Effect size = 0.59). Furthermore, there was no significant correlation between sex, age, or grade point average and the mean test scores in either group (P > 0.05).
Conclusion: Simulation-based training can potentially enhance nursing students' skills in utilizing hospital information systems. Considering the emphasis on the role of health information systems in the management of healthcare settings, it is recommended that simulated HIS training be included in the educational curriculum of nursing students.
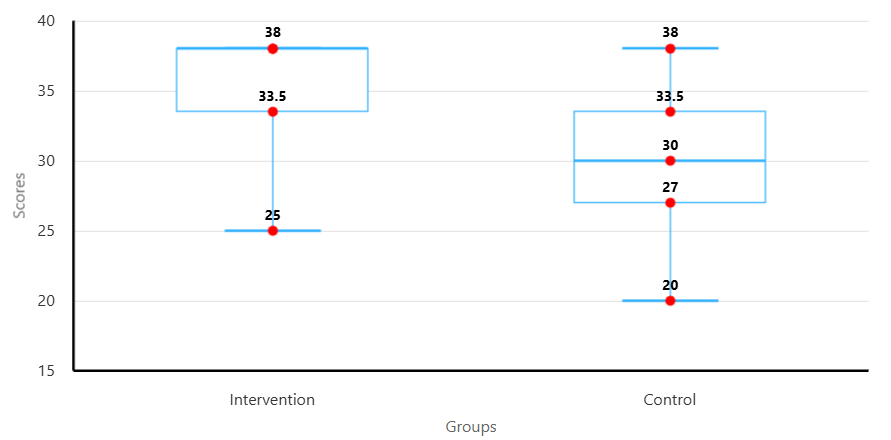
Figure 2. Comparison of students’ test scores between intervention and control groups
To assess the impact of demographic variables on students' test scores, analyses were conducted based on gender, age, and GPA within both the intervention and control groups. The Mann–Whitney U test results showed that the difference in mean scores between female and male students was not statistically significant in either group. In the intervention group, the test statistic was 15 with a p-value of 0.350; in the control group, the test statistic was 16.5 with a p-value of 0.518. These results indicate that gender did not significantly affect test scores (Table 2). Additionally, Spearman's correlation test was used to examine the relationship between age and GPA with test scores. The findings showed no significant correlation between GPA and test scores in the intervention group (r = 0.122, p = 0.693) and the control group (r = -0.343, p = 0.252). Similarly, no statistically significant correlation was found between age and test scores in the intervention group (r = -0.019, p = 0.952) or the control group (r = -0.177, p = 0.563) (Table 3).
Table 2. Comparison of test scores between males and females in each group using the Mann-Whitney U test
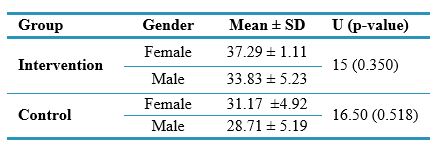
Table 3. Spearman's correlation test results for the effect of age and GPA on students' test scores
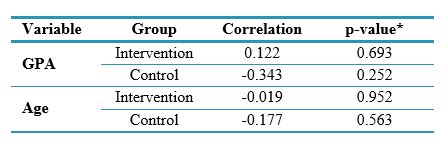
*Correlation is significant at the 0.05 level (2-tailed).
Abbreviations: p-value, probability value.
Discussion
This study evaluated the effect of simulation-based training of the HIS inpatient module on the informatics skills of nursing students before their internship.
The results showed that the HIS education simulator increased nursing students' skills working with the hospital information system's inpatient module. This study found that variables such as gender, age, and GPA did not impact students' informatics skills.
In the present study, students in the intervention group acquired more skills in performing tasks in the inpatient module of the HIS than those in the control group, indicating the usefulness of simulation-based education. In this regard, the results of a systematic review study by Nabovati et al. [17] showed the positive impact of simulators on various outcomes, such as users' skills in using health information systems. The results of a previous study [14] showed that training using an EHR simulator significantly improved the informatics skills of nursing students. A study by Repsha et al. [15] showed a significant increase in scores related to nursing students' informatics competency after using a simulated EHR. The results of another study also emphasized the enhancement of nursing students' informatics competency after simulation-based training in EHR in the first year [18].
In today's world, as HIS use becomes widespread to enhance hospital management, insufficient knowledge and skills among users—particularly nurses and physicians—can lead to several negative consequences. These include decreased efficiency and wasted time, an increased likelihood of errors (such as incorrect data entry) [19], reduced motivation and job satisfaction [20], underutilization of the system's full capabilities [21, 22], and challenges in identifying and resolving technical issues [23]. These issues, in turn, lead to a decline in the quality of care [24, 25], increased costs [23, 26], reduced information security [20], and reporting problems within the organization [26]. Therefore, using these systems without sufficient informatics and computer skills can result in serious problems for both the user and the organization. Therefore, proper training for users before they begin working with the system, especially those who are more familiar with clinical processes but may have less computer knowledge, is critical [27]. Training in a safe, low-risk environment for patients using interactive and active learning methods, such as direct system usage with immediate feedback, is essential compared to traditional teaching methods [28, 29]. This approach offers flexibility and accessibility [30], particularly for nurses working in different shifts or those with limited in-person training resources. Furthermore, standardization of training to ensure uniform learning, easy and effective performance assessment, precise and objective evaluation of nurses, repeatability of training sessions, and ultimately cost reduction provides greater control over the learning process [31]. This leads to reduced stress and anxiety [32], better preparedness for real-life situations [33], and a more effective improvement in informatics skills compared to other training methods [19]. Considering these positive outcomes, it is recommended that simulation-based HIS training be integrated into the curriculum for nursing students, who will be future users of these systems. Additionally, from the outset of their education, alongside practical nursing care skills, nursing students should be introduced to informatics competencies, recognizing the increasing prominence of new technologies in healthcare in the information age. To maximize the effectiveness of simulation-based training, it is advisable to complement it with other educational methods such as real-world exposure and observation of system use in practice.
To the best of our knowledge, this study is one of the first to explore the impact of an HIS education simulator on nursing students' skills in using the inpatient module to document nursing services as future system users. Furthermore, the interactive design of the system's user interface enabled students to record data resembling a real system, guided by the developed scenarios, and navigate through other related processes.
The limitations of this study include its implementation at a single academic center, the short duration of the intervention, and the lack of an assessment of nursing students' baseline informatics skills. Consequently, the generalizability and interpretation of these findings should be approached with caution.
Conclusion
The study demonstrated that a hospital information system training simulator significantly enhanced nursing students' skills in utilizing the HIS inpatient module before starting their internship course.
Preparing students as future end-users of these systems and increasing their skills and self-confidence can improve the quality of healthcare service delivery and patient health outcomes. Therefore, considering the emphasis on the role of systems in the management of healthcare settings, it is recommended that simulated training of the HIS be included in the educational curriculum of nursing students.
Ethical considerations
This study was approved by the ethics committee of Birjand University of Medical Sciences (IR.BUMS.REC.1402.445).
There is no patient in this study; all participants were students. The students' observation of the training and completion of tests were considered implicit consent for their participation in the study.
Artificial intelligence utilization for article writing
No.
Acknowledgment
The authors thank all the students who participated in the study.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author contributions
RF, RA, and FGH conceived and designed the study, acquired and interpreted the data, drafted the manuscript, and critically revised it. RF and RA arranged the logistics of this study. RF, MM, and MR. were responsible for collecting and analyzing the data. All five authors read and approved the final version of the submitted manuscript.
Funding
The research deputy at Birjand University of Medical Sciences funded this study with grant number 6420.
Data availability statement
The datasets used and analyzed during the current study are available in Persian from the corresponding author upon reasonable request.
Background & Objective: Educational simulators have been proposed as effective tools for enhancing learning and improving students' skills when preparing for the workplace. This study aimed to determine the effect of simulation-based training in a hospital information system on nursing students' informatics skills before their internship.
Materials & Methods: This quasi-experimental study was conducted in the first semester of the academic year (2023-2024) with 26 third-semester undergraduate nursing students at the Ferdows Faculty of Medical Sciences. The students were randomly divided into control and intervention groups. The educational content featured a simulation of the inpatient module of a hospital information system. Students in the intervention group were given access to this module's developed training and practice sections over two weeks. After one month, the test section for this module was made available to both the intervention and control groups. Data analysis was conducted using SPSS version 26, where descriptive statistics were calculated, and the Mann-Whitney test was utilized.
Results: After the test, the mean scores of students in the intervention and control groups were 35.69 ± 3.9 and 29.85 ± 5.01 (out of 41), respectively. The difference between the mean scores of the two groups was significant (p = 0.003, Effect size = 0.59). Furthermore, there was no significant correlation between sex, age, or grade point average and the mean test scores in either group (P > 0.05).
Conclusion: Simulation-based training can potentially enhance nursing students' skills in utilizing hospital information systems. Considering the emphasis on the role of health information systems in the management of healthcare settings, it is recommended that simulated HIS training be included in the educational curriculum of nursing students.
Introduction
Over the past two decades, healthcare Information Technology (IT) has developed significantly. Health information technology (HIT) includes a broad spectrum of information systems and tools that enable electronic storage, retrieval, sharing, and use of healthcare data, information, and knowledge for communication and decision-making [1]. These technologies include a variety of systems such as Electronic Health Records (EHR), disease registry systems, electronic prescribing, Hospital Information Systems (HIS), Clinical Decision Support Systems (CDSS), and more [2].
HISs play an important role in planning, implementing, organizing, and controlling the operations of hospital departments, such as laboratory, radiology, admission and discharge, inpatient, and operating room [3]. Successfully implementing HIS in healthcare settings
The mean test scores of students in the intervention and control groups were 35.69 ± 3.9 and 29.85 ± 5.01 (out of 41), respectively. A statistically significant difference was observed between the groups under investigation (U = 27, p = 0.003, Effect size = 0.59). This indicates that simulation-based education for the Inpatient module significantly impacts nursing students' skills (Figure 2).depends on users who rely on these systems to perform their duties [4, 5]. Therefore, comprehensive user training is a crucial element in system development, as it fosters acceptance and enhances users' speed and accuracy in completing tasks and utilizing the system effectively [6].
In Iran, following the implementation of the Health System Transformation Plan in 2013, HIS have received greater attention than other technological advancements in information technology [5]. These systems play a pivotal role in healthcare service delivery and are recognized as key tools for recording and managing patient data and healthcare services [7]. Nurses, as the largest user group of these systems, play a key role in ensuring accurate and comprehensive documentation of clinical data [8]. Despite this vital role, nursing students do not receive the necessary practical training to use HIS effectively during their studies. As a result, new professionals often lack familiarity with these systems upon entering the workforce, even though they must document medical interventions. This lack of experience can lead to challenges such as spending excessive time on data entry and an increased likelihood of documentation errors.
Due to concerns over patient information confidentiality, high work pressure, and the stressful environment of hospitals, clinical internships usually lack hands-on practice with HIS. In most cases, students primarily observe how healthcare staff operate these systems, missing the opportunity to engage directly with the actual HIS environment.
This lack of practical experience can lead to decreased self-confidence, low productivity, and errors in data entry [9].
Simulation has emerged as an innovative and effective educational approach in this context. Using HIS simulators, especially for students with limited experience working with information systems, offers an opportunity to practice in a safe environment without negative patient consequences. This method has numerous advantages over traditional educational methods by allowing repetition, trial and error, active learning, and immediate feedback [10].
While simulation is commonly employed in training for clinical activities such as cardiopulmonary resuscitation and wound care using mannequins and skill laboratories, and some studies [11-15] have utilized EHR simulation for nursing education, there has been less emphasis on comprehensive HIS training that mirrors real hospital workflows.
A research literature review reveals significant gaps in integrating HIS education into the nursing curriculum, particularly in simulated environments. For example, studies by Zhang et al. [16] and Whitt et al. [11] have identified significant limitations. In response to this educational need, a practical training module for the Tiraje HIS nursing system (inpatient module)—used in over 300 hospitals nationwide—was developed using a computer simulator. This study aims to evaluate the effectiveness of a simulation-based educational approach in enhancing nursing students' skills and readiness for using HIS.
Materials & Methods
Design and setting(s)
This quasi-experimental study was conducted at Ferdows Faculty of Medical Sciences during the first semester of the 2023–2024 academic year.
Participants and sampling
The study population comprised 26 third-semester undergraduate nursing students from the Ferdows Faculty of Medical Sciences. After obtaining ethical approval (code IR.BUMS.REC.1402.445) from Birjand University of Medical Sciences and receiving implicit consent from the students in the classroom to participate in the research, a briefing session was conducted for all participants. During this session, the researchers—who hold PhDs in health information management with a background in system design and application and a master's in nursing with experience working with HIS—introduced the scenario-based computer simulator. They clearly explained the study objectives, its significance, and how to use the training, practice, and testing sections in the simulator. Adequate time was provided to address any questions or concerns from students regarding the process.
After the briefing session, a census sampling approach was employed, including all students in the class. Subsequently, 26 sealed envelopes were prepared, with 13 labelled 'Intervention' and 13 labelled 'Control.' To ensure random allocation, each student blindly selected an envelope, determining their assignment to one of the study groups. Finally, students' demographic characteristics, including sex, age, and Grade Point Average (GPA), were recorded on a checklist (Figure 1).
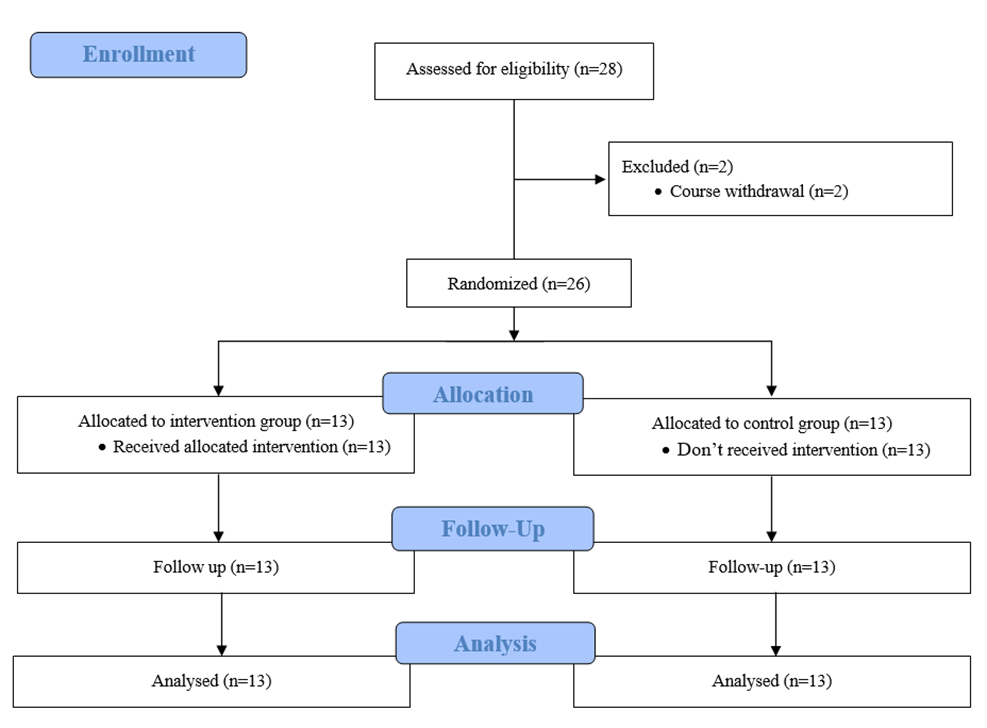
Figure 1. CONSORT Flow diagram of the quasi-experimental study
In Iran, following the implementation of the Health System Transformation Plan in 2013, HIS have received greater attention than other technological advancements in information technology [5]. These systems play a pivotal role in healthcare service delivery and are recognized as key tools for recording and managing patient data and healthcare services [7]. Nurses, as the largest user group of these systems, play a key role in ensuring accurate and comprehensive documentation of clinical data [8]. Despite this vital role, nursing students do not receive the necessary practical training to use HIS effectively during their studies. As a result, new professionals often lack familiarity with these systems upon entering the workforce, even though they must document medical interventions. This lack of experience can lead to challenges such as spending excessive time on data entry and an increased likelihood of documentation errors.
Due to concerns over patient information confidentiality, high work pressure, and the stressful environment of hospitals, clinical internships usually lack hands-on practice with HIS. In most cases, students primarily observe how healthcare staff operate these systems, missing the opportunity to engage directly with the actual HIS environment.
This lack of practical experience can lead to decreased self-confidence, low productivity, and errors in data entry [9].
Simulation has emerged as an innovative and effective educational approach in this context. Using HIS simulators, especially for students with limited experience working with information systems, offers an opportunity to practice in a safe environment without negative patient consequences. This method has numerous advantages over traditional educational methods by allowing repetition, trial and error, active learning, and immediate feedback [10].
While simulation is commonly employed in training for clinical activities such as cardiopulmonary resuscitation and wound care using mannequins and skill laboratories, and some studies [11-15] have utilized EHR simulation for nursing education, there has been less emphasis on comprehensive HIS training that mirrors real hospital workflows.
A research literature review reveals significant gaps in integrating HIS education into the nursing curriculum, particularly in simulated environments. For example, studies by Zhang et al. [16] and Whitt et al. [11] have identified significant limitations. In response to this educational need, a practical training module for the Tiraje HIS nursing system (inpatient module)—used in over 300 hospitals nationwide—was developed using a computer simulator. This study aims to evaluate the effectiveness of a simulation-based educational approach in enhancing nursing students' skills and readiness for using HIS.
Materials & Methods
Design and setting(s)
This quasi-experimental study was conducted at Ferdows Faculty of Medical Sciences during the first semester of the 2023–2024 academic year.
Participants and sampling
The study population comprised 26 third-semester undergraduate nursing students from the Ferdows Faculty of Medical Sciences. After obtaining ethical approval (code IR.BUMS.REC.1402.445) from Birjand University of Medical Sciences and receiving implicit consent from the students in the classroom to participate in the research, a briefing session was conducted for all participants. During this session, the researchers—who hold PhDs in health information management with a background in system design and application and a master's in nursing with experience working with HIS—introduced the scenario-based computer simulator. They clearly explained the study objectives, its significance, and how to use the training, practice, and testing sections in the simulator. Adequate time was provided to address any questions or concerns from students regarding the process.
After the briefing session, a census sampling approach was employed, including all students in the class. Subsequently, 26 sealed envelopes were prepared, with 13 labelled 'Intervention' and 13 labelled 'Control.' To ensure random allocation, each student blindly selected an envelope, determining their assignment to one of the study groups. Finally, students' demographic characteristics, including sex, age, and Grade Point Average (GPA), were recorded on a checklist (Figure 1).
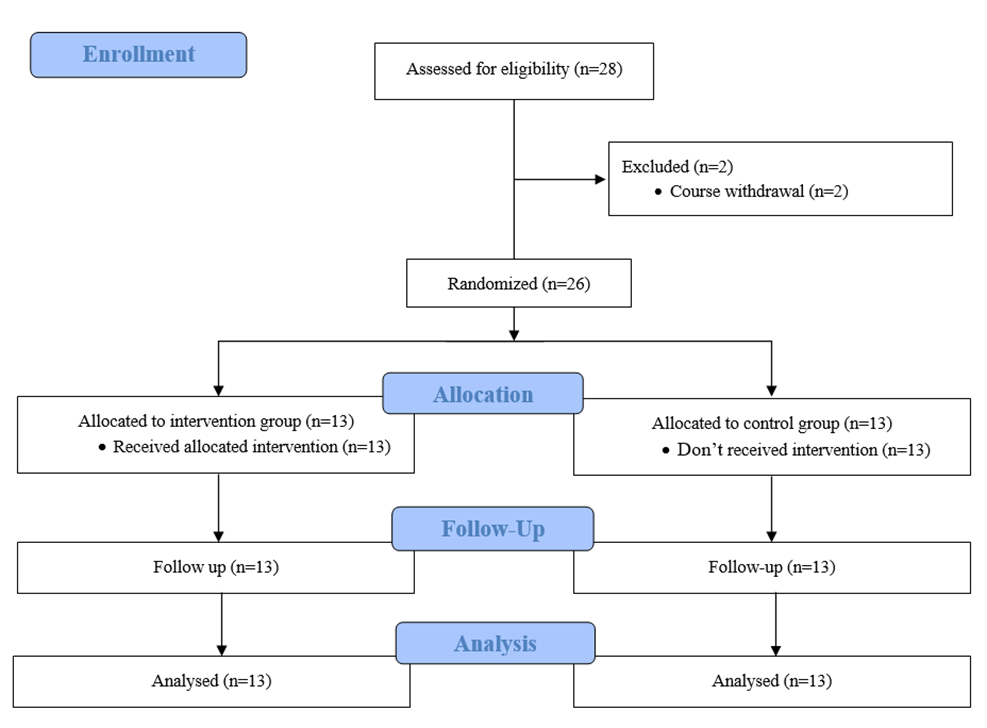
Figure 1. CONSORT Flow diagram of the quasi-experimental study
Tools/Instruments
The web-based simulator system for teaching HIS includes several key functional capabilities, such as interactive training courses, multimedia content, practical exercises, and assessments. Additionally, it provides help and feedback to users to address their potential errors. This system's administration, communication, and content management capabilities can extend the learning process beyond other educational simulators. Additional features, including information dashboards, reporting capabilities, question bank design, and messaging, have also been incorporated to create a fully integrated educational system.
Data collection methods
One of this system's simulated educational contents is the inpatient module training in the HIS. This module, one of the most widely used modules by nursing staff, was introduced to nursing students in the intervention group. In this module, students were taught how to log into the hospital information system, assign beds from different hospital departments to patients, register requests for
various services such as laboratory tests, medications, and patient imaging, cancel or delete orders, and view test results and medications assigned to the patient. Students were granted access to the training and, subsequently, the practice content for this module, allowing them to train and practice anytime, anywhere, and on any device—a mobile phone, tablet, laptop, or personal computer—over two weeks. To complete the process, students needed to select the "End of Training" option after finishing the training and the "End of Practice" option after completing the practice to finalize their progress. One month later, both the intervention and control groups completed the test section of the module to evaluate the training's impact on their skills in using the Tiraje Hospital Information System. Students were asked to complete the test, which was designed in a scenario-based format aligned with the educational content, and completed exercises. The validity and reliability of the test (Supplementary 1), created by nurses using this module based on real patients, were reviewed and approved by experts in Health Information Management (HIM) and Medical Informatics (MI), who are familiar with the design and use of this system. A scenario consisting of 16 steps was prepared, with each step scored according to weighted importance analysis. The importance of each scenario step was determined based on expert opinion, and each step was scored based on its importance. The students recorded their scores on the system after completing the test. The simulator calculated the module-specific test score with a maximum score of 41, and the scores obtained by both groups were compared.
Data analysis
After receiving demographic information and students' test scores through the simulator system, these data were entered into the SPSS software ver.26 for analysis. First, the data were described using descriptive statistics (frequency, percentage, mean, and SD). Because the dependent variable (test score) did not have a normal distribution, the Mann-Whitney U test was used to compare the scores of the intervention and control groups. Furthermore, Spearman's correlation coefficient test examined the association between the demographic and dependent variables.
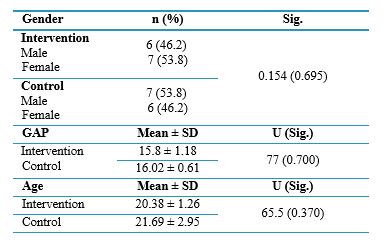
Results
Of the 26 participants, 13 (50%) were male. After sample allocation, seven females (54%) and six males (46%) were placed in the intervention group, and seven males (54%) and six females (46%) were placed in the control group. The distribution of the participants was not group. The distribution of the participants was not statistically significant (p = 0.695). The GPA of students in the intervention group was 15.80 ± 1.18, and in control, it was 16.02 ± 0.61, with no significant difference between the two groups (p = 0.700). Also, the mean age of students in the intervention group was 20.38 ± 1.26 years, and in control, it was 21.69 ± 2.95 years, and there was no statistically significant difference between the two study groups (p = 0.370) (Table 1).
Table 1. Demographic characteristics of intervention and control groups
Abbreviations: n, number of participants; SD, standard deviation; U, Mann-Whitney test; Sig, significance level. The web-based simulator system for teaching HIS includes several key functional capabilities, such as interactive training courses, multimedia content, practical exercises, and assessments. Additionally, it provides help and feedback to users to address their potential errors. This system's administration, communication, and content management capabilities can extend the learning process beyond other educational simulators. Additional features, including information dashboards, reporting capabilities, question bank design, and messaging, have also been incorporated to create a fully integrated educational system.
Data collection methods
One of this system's simulated educational contents is the inpatient module training in the HIS. This module, one of the most widely used modules by nursing staff, was introduced to nursing students in the intervention group. In this module, students were taught how to log into the hospital information system, assign beds from different hospital departments to patients, register requests for
various services such as laboratory tests, medications, and patient imaging, cancel or delete orders, and view test results and medications assigned to the patient. Students were granted access to the training and, subsequently, the practice content for this module, allowing them to train and practice anytime, anywhere, and on any device—a mobile phone, tablet, laptop, or personal computer—over two weeks. To complete the process, students needed to select the "End of Training" option after finishing the training and the "End of Practice" option after completing the practice to finalize their progress. One month later, both the intervention and control groups completed the test section of the module to evaluate the training's impact on their skills in using the Tiraje Hospital Information System. Students were asked to complete the test, which was designed in a scenario-based format aligned with the educational content, and completed exercises. The validity and reliability of the test (Supplementary 1), created by nurses using this module based on real patients, were reviewed and approved by experts in Health Information Management (HIM) and Medical Informatics (MI), who are familiar with the design and use of this system. A scenario consisting of 16 steps was prepared, with each step scored according to weighted importance analysis. The importance of each scenario step was determined based on expert opinion, and each step was scored based on its importance. The students recorded their scores on the system after completing the test. The simulator calculated the module-specific test score with a maximum score of 41, and the scores obtained by both groups were compared.
Data analysis
After receiving demographic information and students' test scores through the simulator system, these data were entered into the SPSS software ver.26 for analysis. First, the data were described using descriptive statistics (frequency, percentage, mean, and SD). Because the dependent variable (test score) did not have a normal distribution, the Mann-Whitney U test was used to compare the scores of the intervention and control groups. Furthermore, Spearman's correlation coefficient test examined the association between the demographic and dependent variables.
Results
Of the 26 participants, 13 (50%) were male. After sample allocation, seven females (54%) and six males (46%) were placed in the intervention group, and seven males (54%) and six females (46%) were placed in the control group. The distribution of the participants was not group. The distribution of the participants was not statistically significant (p = 0.695). The GPA of students in the intervention group was 15.80 ± 1.18, and in control, it was 16.02 ± 0.61, with no significant difference between the two groups (p = 0.700). Also, the mean age of students in the intervention group was 20.38 ± 1.26 years, and in control, it was 21.69 ± 2.95 years, and there was no statistically significant difference between the two study groups (p = 0.370) (Table 1).
Table 1. Demographic characteristics of intervention and control groups
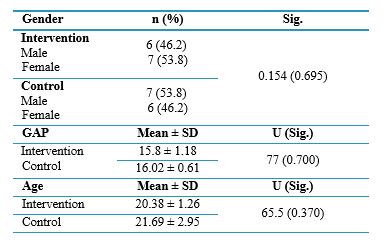
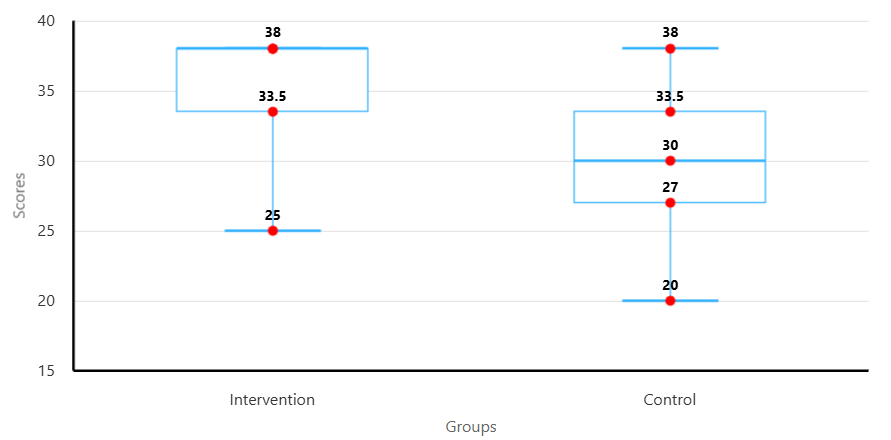
Figure 2. Comparison of students’ test scores between intervention and control groups
To assess the impact of demographic variables on students' test scores, analyses were conducted based on gender, age, and GPA within both the intervention and control groups. The Mann–Whitney U test results showed that the difference in mean scores between female and male students was not statistically significant in either group. In the intervention group, the test statistic was 15 with a p-value of 0.350; in the control group, the test statistic was 16.5 with a p-value of 0.518. These results indicate that gender did not significantly affect test scores (Table 2). Additionally, Spearman's correlation test was used to examine the relationship between age and GPA with test scores. The findings showed no significant correlation between GPA and test scores in the intervention group (r = 0.122, p = 0.693) and the control group (r = -0.343, p = 0.252). Similarly, no statistically significant correlation was found between age and test scores in the intervention group (r = -0.019, p = 0.952) or the control group (r = -0.177, p = 0.563) (Table 3).
Table 2. Comparison of test scores between males and females in each group using the Mann-Whitney U test
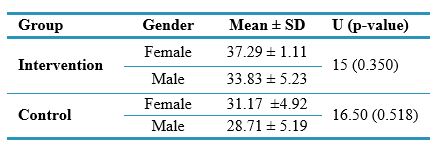
Table 3. Spearman's correlation test results for the effect of age and GPA on students' test scores
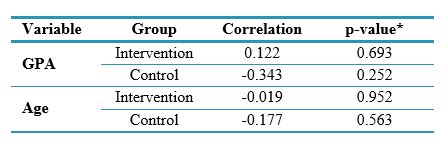
*Correlation is significant at the 0.05 level (2-tailed).
Abbreviations: p-value, probability value.
Discussion
This study evaluated the effect of simulation-based training of the HIS inpatient module on the informatics skills of nursing students before their internship.
The results showed that the HIS education simulator increased nursing students' skills working with the hospital information system's inpatient module. This study found that variables such as gender, age, and GPA did not impact students' informatics skills.
In the present study, students in the intervention group acquired more skills in performing tasks in the inpatient module of the HIS than those in the control group, indicating the usefulness of simulation-based education. In this regard, the results of a systematic review study by Nabovati et al. [17] showed the positive impact of simulators on various outcomes, such as users' skills in using health information systems. The results of a previous study [14] showed that training using an EHR simulator significantly improved the informatics skills of nursing students. A study by Repsha et al. [15] showed a significant increase in scores related to nursing students' informatics competency after using a simulated EHR. The results of another study also emphasized the enhancement of nursing students' informatics competency after simulation-based training in EHR in the first year [18].
In today's world, as HIS use becomes widespread to enhance hospital management, insufficient knowledge and skills among users—particularly nurses and physicians—can lead to several negative consequences. These include decreased efficiency and wasted time, an increased likelihood of errors (such as incorrect data entry) [19], reduced motivation and job satisfaction [20], underutilization of the system's full capabilities [21, 22], and challenges in identifying and resolving technical issues [23]. These issues, in turn, lead to a decline in the quality of care [24, 25], increased costs [23, 26], reduced information security [20], and reporting problems within the organization [26]. Therefore, using these systems without sufficient informatics and computer skills can result in serious problems for both the user and the organization. Therefore, proper training for users before they begin working with the system, especially those who are more familiar with clinical processes but may have less computer knowledge, is critical [27]. Training in a safe, low-risk environment for patients using interactive and active learning methods, such as direct system usage with immediate feedback, is essential compared to traditional teaching methods [28, 29]. This approach offers flexibility and accessibility [30], particularly for nurses working in different shifts or those with limited in-person training resources. Furthermore, standardization of training to ensure uniform learning, easy and effective performance assessment, precise and objective evaluation of nurses, repeatability of training sessions, and ultimately cost reduction provides greater control over the learning process [31]. This leads to reduced stress and anxiety [32], better preparedness for real-life situations [33], and a more effective improvement in informatics skills compared to other training methods [19]. Considering these positive outcomes, it is recommended that simulation-based HIS training be integrated into the curriculum for nursing students, who will be future users of these systems. Additionally, from the outset of their education, alongside practical nursing care skills, nursing students should be introduced to informatics competencies, recognizing the increasing prominence of new technologies in healthcare in the information age. To maximize the effectiveness of simulation-based training, it is advisable to complement it with other educational methods such as real-world exposure and observation of system use in practice.
To the best of our knowledge, this study is one of the first to explore the impact of an HIS education simulator on nursing students' skills in using the inpatient module to document nursing services as future system users. Furthermore, the interactive design of the system's user interface enabled students to record data resembling a real system, guided by the developed scenarios, and navigate through other related processes.
The limitations of this study include its implementation at a single academic center, the short duration of the intervention, and the lack of an assessment of nursing students' baseline informatics skills. Consequently, the generalizability and interpretation of these findings should be approached with caution.
Conclusion
The study demonstrated that a hospital information system training simulator significantly enhanced nursing students' skills in utilizing the HIS inpatient module before starting their internship course.
Preparing students as future end-users of these systems and increasing their skills and self-confidence can improve the quality of healthcare service delivery and patient health outcomes. Therefore, considering the emphasis on the role of systems in the management of healthcare settings, it is recommended that simulated training of the HIS be included in the educational curriculum of nursing students.
Ethical considerations
This study was approved by the ethics committee of Birjand University of Medical Sciences (IR.BUMS.REC.1402.445).
There is no patient in this study; all participants were students. The students' observation of the training and completion of tests were considered implicit consent for their participation in the study.
Artificial intelligence utilization for article writing
No.
Acknowledgment
The authors thank all the students who participated in the study.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author contributions
RF, RA, and FGH conceived and designed the study, acquired and interpreted the data, drafted the manuscript, and critically revised it. RF and RA arranged the logistics of this study. RF, MM, and MR. were responsible for collecting and analyzing the data. All five authors read and approved the final version of the submitted manuscript.
Funding
The research deputy at Birjand University of Medical Sciences funded this study with grant number 6420.
Data availability statement
The datasets used and analyzed during the current study are available in Persian from the corresponding author upon reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2024/11/4 | Accepted: 2025/05/12 | Published: 2025/07/13
Received: 2024/11/4 | Accepted: 2025/05/12 | Published: 2025/07/13
References
1. Manning SE, Wang H, Dwibedi N, et al. Association of multimorbidity with the use of health information technology. Digital Health. 2023;9:20552076231163797 [DOI]
2. Taneja D, Kulkarni SV, Sinha S, Dindigal RN. Digital technology in hospital administration: a strategic choice. The Journal of the Association of Physicians of India. 2023;71(10):83-8 [DOI]
3. Ismail A, Jamil AT, Rahman AFA, et al. The implementation of hospital information system (HIS) in tertiary hospitals in malaysia: a qualitative study. Malaysian Journal of Public Health Medicine. 2010;10(2):16-24 [DOI]
4. Theo L, Sauerborn R, Bodart C. Design and implementation of health information systems. Geneva: World Health Organization. 2000 [DOI]
5. Shojaei Baghini M, Naseri Boori Abadi T, Joodaki M, Mollaee S. Progress of hospital information systems in Kerman teaching general hospitals in 2012. Journal of Modern Medical Information Sciences. 2015;1(1):42-50. [DOI]
6. George NM, Drahnak DM, Schroeder DL, Katrancha ED. Enhancing prelicensure nursing students' use of an electronic health record. Clinical Simulation in Nursing. 2016;12(5):152-8. [DOI]
7. Pfob A, Griewing S, Seitz K, et al. Current landscape of hospital information systems in gynecology and obstetrics in Germany: a survey of the commission digital medicine of the German society for gynecology and obstetrics. Archives of Gynecology and Obstetrics. 2023;308(6):1823-30 [DOI]
8. Ahmed SS. The Relationship between nursing knowledge about documentation skills and auditing retrospective of patient's records. Helwan International Journal for Nursing Research and Practice. 2024;3(5):213-28. [DOI]
9. Zhang L, Wu J, Yang J, et al. Development and application evaluation of a nursing simulation teaching information system based on hospital information systems. International Journal of Clinical Practice. 2023;2023(1):6334967 [DOI]
10. Sivanjali M. The effectiveness of simulation-based learning in clinical education. Batticaloa Medical Journal. 2024;18(1). [DOI]
11. Whitt KJ, Allen CL, Hogg CW, et al. The use of electronic health records in advanced practice nursing education: a scoping review. Journal of Professional Nursing. 2024;50:83-94 [DOI]
12. McBride S, Thomas L, Decker S, et al. Validation of a tool to evaluate nursing students’ electronic health record competency in simulation. Nursing Education Perspectives. 2021;45(3):161. [DOI]
13. Kobeissi MM. Enhancing simulation: a roadmap for integrating the electronic health record into the nurse practitioner curriculum. Clinical Simulation in Nursing. 2023;85:101460. [DOI]
14. Choi J, Bove LA, Tarte V, Choi WJ. Impact of simulated electronic health records on informatics competency of students in informatics course. Healthcare Informatics Research. 2021;27(1):67-72. [DOI]
15. Repsha C, Morse B, Lee SE, Katz J, Burrows E, Teates J. Use of a simulated electronic health record to support nursing student informatics knowledge and skills. Computers, Informatics, Nursing. 2020;38(2):55-9. [DOI]
16. Zhang L, Wu J, Yang J, et al. Development and application evaluation of a nursing simulation teaching information system based on hospital information systems. International Journal of Clinical Practice. 2023;2023:6334967. [DOI]
17. Nabovati E, Jeddi FR, Ghaffari F, Mirhoseini F. The effects of simulation training on learning of health information systems: A scoping review. Journal of Education and Health Promotion. 2022;11:4. [DOI]
18. Gosa LK. Improving EMR Competency in First Year Nursing Students. 2022. [DOI]
19. Raghunathan K, McKenna L, Peddle M. Baseline evaluation of nursing students’ informatics competency for digital health practice: A descriptive exploratory study. Digital Health. 2023:20552076231179051. [DOI]
20. Alamro AA, Aljuma MS, Alateeq SS, et al. Challenges of health informatics systems in primary health care. Saudi Journal of Medical and Pharmaceutical Sciences. 2023;9(10):717-9 [DOI]
21. Choi J, Woo S, Tarte V. Informatics competencies of students in a doctor of nursing practice program: a descriptive study. Healthcare Informatics Research. 2024;30(2):147-53 [DOI]
22. Belchez CA. Informatics and faculty intraprofessional assessment and gap analysis of current integration of informatics competencies in a baccalaureate nursing program: University of Kansas; 2019. [DOI]
23. Chikware AB, Roman NV, Davids EL. Improving health informatics competencies: a scoping review of the components of health informatics academic programs. SAGE Open. 2024;14(4):21582440241293259. [DOI]
24. Al Najjar RI, Shafie ZM. Impact of nursing informatics on the quality of patient care. International Journal of Medical Science and Clinical Research Studies. 2022;2(5):418-21. [DOI]
25. Otokiti A. Using informatics to improve healthcare quality. International Journal of Health Care Quality Assurance. 2019;32(2):425-30. [DOI]
26. Coppersmith NA, Sarkar IN, Chen ES. Quality informatics: the convergence of healthcare data, analytics, and clinical excellence. Applied Clinical Informatics. 2019;10(02):272-7. [DOI]
27. Aurore N, Valens M, Lune NJ, Nyssen M. Assessment of health informatics competencies in undergraduate training of healthcare professionals in Rwanda. Rwanda Journal. 2016;3(1):36-41 [DOI]
28. Jeffery AD, Sengstack P. Teaching data science through an interactive, hands-on workshop with clinically relevant case studies. Applied Clinical Informatics. 2024;15(05):1074-9. [DOI]
29. Hare AJ, Soegaard Ballester JM, Gabriel PE, Adusumalli S, Hanson III CW. Training digital natives to transform healthcare: a 5-tiered approach for integrating clinical informatics into undergraduate medical education. Journal of the American Medical Informatics Association. 2023;30(1):139-43. [DOI]
30. Chang H. Recent movement on education and training in health informatics. Healthcare Informatics Research. 2014;20(2):79. [DOI]
31. Wu H, Patel MK, Tan CC. The current landscape of cybersecurity training in CAHIIM accredited programs. In2024 IEEE 12th International Conference on Healthcare Informatics (ICHI) 2024 Jun 3 (pp. 750-752). IEEE. [DOI]
32. Sapci AH, Sapci HA. Digital continuous healthcare and disruptive medical technologies: m-health and telemedicine skills training for data-driven healthcare. Journal of Telemedicine and Telecare. 2019;25(10):623-35. [DOI]
33. Kleib M, Nagle L. Factors associated with Canadian nurses' informatics competency. Computers, Informatics, Nursing. 2018;36(8):406-15. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |