Sun, Feb 22, 2026
[Archive]
Volume 18, Issue 3 (2025)
J Med Edu Dev 2025, 18(3): 99-108 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abushouk S, Hamad B, Arbab A. Perceptions of dental students regarding the practice and impact of the hidden curriculum at Al-neelain University, Sudan. J Med Edu Dev 2025; 18 (3) :99-108
URL: http://edujournal.zums.ac.ir/article-1-2278-en.html
URL: http://edujournal.zums.ac.ir/article-1-2278-en.html
1- Department of Restorative Dentistry, Khartoum Dental Teaching Hospital, Khartoum State, Sudan & Sudan Medical Specialization Board, Khartoum State, Sudan
2- Faculty of Medicine, International University of Africa, Khartoum, Sudan & Sudan Medical Specialization Board, Khartoum State, Sudan
3- Department of Pharmacognosy, Faculty of Pharmacy, University of Khartoum, Khartoum State, Sudan & Sudan Medical Specialization Board, Khartoum State, Sudan ,arbabssn@gmail.com
2- Faculty of Medicine, International University of Africa, Khartoum, Sudan & Sudan Medical Specialization Board, Khartoum State, Sudan
3- Department of Pharmacognosy, Faculty of Pharmacy, University of Khartoum, Khartoum State, Sudan & Sudan Medical Specialization Board, Khartoum State, Sudan ,
Full-Text [PDF 553 kb]
(447 Downloads)
| Abstract (HTML) (936 Views)
Full-Text: (38 Views)
Abstract
Background & Objective: The Hidden Curriculum (HC) represents the cultural process of medical training, where students acquire attitudes and values. Understanding the HC enables educators to develop more impactful learning experiences. Therefore, this study aims to assess the perceptions of Al-Neelain University dental students regarding the frequency and impact of positive and negative aspects of the HC.
Materials & Methods: A cross-sectional study was conducted among a randomly selected sample of fifth-year dental students at Al-Neelain University (Sudan). Data were collected using the self-administered Hidden Informal Curriculum Assessment Tool (HICAT). The data were analyzed using the Mann-Whitney U test, Kruskal-Wallis test, and McNemar test.
Results: The response rate was 100% (81 out of 81), with 70.3% of respondents identifying as female. Approximately 53% of the respondents were single, and 86.4% were citizens. The most commonly reported positive scenario was a satisfactory patient-doctor consultation, noted by 60% of participants. In contrast, the least frequently observed positive scenario was the presence of high professional standards in their learning environments, reported by only 25%. On the negative side, the most frequently cited issue was discriminatory attitudes in learning environments, affecting 52% of respondents. Conversely, ethnic discrimination and gender discrimination were the least frequently reported negative scenarios, at 7% and 9%, respectively. Data revealed a statistically significant association between perceptions of certain HC scenarios and gender (p = 0.047), Citizenship (p = 0.045), and social status (p = 0.003). The top two influential scenarios identified were having a positive role model doctor and developing strong patient-doctor skills.
Conclusion: Respondents frequently reported positive patient-doctor consultations, while discriminatory attitudes in learning environments were the most common negative scenario. Understanding students' perceptions of healthcare is essential, as it can help reinforce positive aspects and improve negative ones in the future.
Introduction
Materials & Methods
Design and setting(s)
A descriptive cross-sectional study was conducted at the Faculty of Dentistry at Al-Neelain University, which was established in 2005.It has a distinct curriculum with clear goals and vision towards society; it includes a total of 11 semesters. The faculty has 12 departments in various dental specialties. The faculty offers students advanced training in dentistry through clinics and industrial replacement laboratories. They participate in activities like therapeutic days and educational visits to achieve the college's vision. Students receive early clinical training along with comprehensive patient care. The study was conducted from September 2021 to June 2022.
Participants and sampling
The study focused on undergraduate fifth-year students at the Faculty of Dentistry at Al-Neelain University. It included both female and male fifth-year students who were registered in the bachelor's degree program in dentistry, as well as foreign students. Students who were not registered for courses during the study period were excluded. According to the records from the Al-Neelain University Faculty of Dentistry, there are 102 students enrolled in the fifth year. The minimum sample size required for the study was calculated to be 81, using the Open-Source Epidemiologic Statistics for Public Health Version 3.01 online calculator, with a confidence level of 95% [17]. For sampling, systematic random sampling was employed, utilizing the list of fifth-year students as the sampling frame. The sampling interval was determined by dividing the total population size (N = 102) by the desired sample size [18]. The first participant was selected by simple random sampling.
Tools/Instruments
The data were collected online using a self-administered questionnaire as a data collection tool. The questionnaire consisted of two sections. The first section examined the sociodemographic characteristics of the participating students. The second section contained the Hidden Curriculum Assessment Tool (HICAT) [18]. The questionnaire consisted of four sections and comprised 27 items. The first section consisted of four questions to explore the socio-demographic characteristics of the participants.
The second section outlines ten positive HC scenarios that students may have experienced during their studies. The third section features ten negative HC scenarios.
The fourth section, titled "Impact Rating," requests students to identify the three scenarios that had the most significant impact on them during their clinical rotations, selecting from the previously mentioned 20 scenarios. This section emphasizes the depth of the impact rather than the frequency with which the scenarios were encountered. In the first and second sections of the questionnaire (comprising ten positive and ten negative HC scenarios), participants' responses were rated using a modified 4-point Likert scale: 1. Usually/Always, 2. Half the time, 3. Never/Occasionally, 4. Not applicable. Permission to use HICAT was obtained via email correspondence from Prof. Paul McGurgan, the originator of the questionnaire at the University of Western Australia. HICAT is used to quantify both the frequency of positive and negative aspects of the HC and the impact of these experiences on dental students. It was developed in two main steps. Initially, the authors developed a range of educational scenarios related to the HC based on a literature review, intending to capture both positive and negative aspects. Subsequently, a focus group of medical students reviewed and refined these scenarios, selecting the most relevant ones based on their individual experiences. The most common scenarios (ten negative and ten positive) served as the foundation for the instrument. After that, the instrument was piloted on a second rotation of medical students to ensure its user-friendliness and internal validity [18]. To ensure validity within our context, the questionnaire was reviewed by a panel of four experts who critically evaluated its content and relevance. The instrument demonstrated acceptable reliability, with a Cronbach’s Alpha of 0.682.
Data collection methods
Before administering the HICAT questionnaire, fifth-year dental students were provided with information about the study. This included a definition of the HC, assurances of confidentiality, and a statement indicating that participation was voluntary and would not affect their academic outcomes. The online HICAT questionnaire was created using Google Forms and was subsequently hosted online via a unique URL. Pre-selected study participants were invited individually to participate through their contact information. Participants’ responses were automatically collected and stored in a Google Drive.
Data analysis
The Statistical Package for Social Sciences (SPSS) version 17 was utilized for coding, entering, and analyzing participants' responses. Descriptive analysis was conducted to summarize the data, with frequency and percentages calculated for categorical variables, and mean and standard deviation employed for continuous variables. Non-parametric statistics were used to identify significant differences or associations between independent and dependent variables. The non-parametric tests applied included the Mann-Whitney U test, Kruskal-Wallis test, and McNemar test. A p-value of 0.05 or less was considered statistically significant.
Results
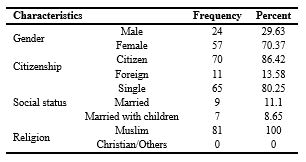
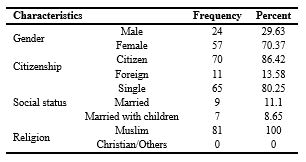
The response rate was 100% (81 out of 81 participants). As shown in Table 1, the majority of respondents were females (70.3%). More than half (53%) of the respondents were single, and a significant proportion (86.4%) were citizens. Additionally, all respondents identified as Muslims (100%).
Table 1. Sociodemographic characteristics of participants (n = 81)
As shown in Table 2, the most highly valued positive scenarios reported by respondents included observing positive patient-doctor consultations (60%), followed by witnessing health professionals educating patients about their conditions (56%), encountering health professionals regarded as positive role models (49%), and observing staff acknowledging their limitations (49%). The least frequent items observed were observing high professional standards in their learning environments (25%) and observing patients being treated as unique individuals (28%). Regarding the negative HC scenarios (Table 3), the most frequent scenario was discriminatory attitudes in learning environments (52%). The least frequent negative scenarios were discrimination due to ethnic background (7%) or gender (9%), followed by feeling humiliated by a supervisor (21%). Participants' responses were analyzed in relation to their demographic data to identify potential associations between demographic factors and perceptions of HC scenarios. Among positive and negative scenarios, only those demonstrating a significant association between demographic factors and student responses were discussed. Females were more often asked to undertake unsupervised tasks whilst feeling unconfident (p = 0.047) and were more troubled by the experiences encountered than their male counterparts (p = 0.015). On the other hand, males reported feeling disadvantaged due to their ethnic background more often than females (p = 0.047) and felt more supported during their placements (p = 0.045). Additionally, data analysis revealed a statistically significant association between citizenship and three HC scenarios. Citizens were more frequently asked to undertake unsupervised tasks while feeling unconfident
(p = 0.045) and were observed to develop doctor-patient skills more often than foreign students (p = 0.018). In contrast, foreign students felt disadvantaged because of their ethnic background (p = 0.001).
Table 2. Responses of the participants to the positive hidden curriculum scenarios

Abbreviations: n, number of participants; %, percentage.
Table 3. Responses of the participants to the negative hidden curriculum scenarios

Abbreviations: n, number of participants; %, percentage.
The social status of the respondents was significantly associated only with doctor-patient consultations (p = 0.035) (Table 4). Respondents reported two positive scenarios and one negative scenario as their three most influential HC scenarios. The most impactful positive scenarios identified were “I have encountered health professionals I consider to be positive role models” and “I was inspired to develop my doctor-patient skills.” In contrast, the most frequently reported negative scenario was “I needed to compete with other dental students” (Table 5).
Furthermore, data analysis showed a significant difference between the most impactful negative scenario and each of the two most frequently cited positive scenarios, with p-values of 0.046 and 0.040, respectively (Table 6).
Table 4. Association between sociodemographic characteristics of the participants and the hidden curriculum scenarios

Notes: *Mann-Whitney U test was used to compare assocation between gender, citizinship and the hidden curriculum scenarios, **Kruskal-Wallis test was used to compare the association between social status and and the hidden curriculum scenarios.
Abbreviations: N, frequency ;Sig, statistical significance; p, probability -value; Z, z-score (standardized Mann-Whitney U test test statistic); H, Kruskal-Wallis test statistic
Table 5. The participants' rankings of hidden curriculum scenarios

Note: Times selected, the frequency with which a specific scenario was chosen by the participants; Percent (%), the proportion of times a given experience was selected based on n = 243; percent of respondents(%), the proportion of respondents who selected each experience based on n = 81, acknowledging that each respondent could select more than one experience.
Table 6. Comparison between the three most impactful scenarios

Discussion
This study aimed to identify positive aspects of the HC that can be reinforced, while also identifying negative aspects that should be avoided or reshaped. The ultimate goal is to improve the cultures of both the health professions and education. The HICAT was utilized to measure both the frequency of dental students' experiences with HC scenarios and the impact of these experiences.This tool is useful for evaluating medical students in clinical and educational settings to determine their strengths and weaknesses [18]. Among the ten positive scenarios, the majority of students in this study observed a positive attitude during patient-doctor consultations. Patients expressed a desire to be informed about their condition and to receive support from their doctors. These findings align with results from a study conducted at the University of Western Australia, where 93% of students agreed on the same scenarios [18]. Additionally, our findings are partially in line with the findings of a study conducted in Pakistan, where medical students highly valued the demonstration of high professional standards, the exhibition of positive role modeling, and positive doctor-patient relationships [19]. Moreover, a qualitative study among dental students in Iran demonstrated the importance of considering a professor's professional behavior and their role as a role model [20]. The least frequently observed positive scenarios were “observing patients being treated as unique individuals” and “observing high professional standards in the learning environments.” Our findings contrast with a study conducted in Pakistan, where the least valued items were observing staff admitting their limitations and witnessing health professionals effectively managing complex cases in a positive manner [19]. These differences could be attributed to differences in participants' social culture. Professionalism is a culture‑dependent ability and training for all professional responsibilities is a difficult task that comes with many obstacles as stated in many studies [21, 22]. The gap between knowledge and practice, a lack of emphasis on continuous professional education, the normalization of certain behaviors, and the neglect of the importance of being observed as a role model were identified as justifications for these findings, which can also be relevant to the Sudanese context [23]. Regarding negative scenarios, the most common experience reported was witnessing discriminatory attitudes in learning environments (52%). This finding aligns with a survey conducted among internal medicine trainees in the United States, where nearly two-thirds of respondents reported observing unequal treatment of patients from various backgrounds [24]. Discriminatory attitudes in the learning environment can negatively affect students' educational outcomes. Efforts should be directed to address and implement strategies to eliminate such attitudes and maintain health equity. Furthermore, there is a need to train dental students and educators on how to effectively respond to any form of prejudiced attitudes. Conversely, the least frequently observed negative scenarios included disadvantages faced by students due to their gender (9%) or ethnic background (7%). This latter finding is somewhat unexpected, given the ethnic diversity in the country and the reported discrimination claims and conflicts between tribes. Additionally, the issue of gender equity within the educational environment is noteworthy. Education for women in Sudan began as early as 1903 [25], and since then, women have made significant strides in education and have become major contributors to society. Data analysis showed a statistically significant association between gender and confidence to perform unsupervised tasks. Females were more often asked to undertake unsupervised tasks whilst feeling unconfident. Similarly, females were observed to be troubled half of the time by the new experiences they encounter (p = 0.015) than their male counterparts. The majority of them never had that feeling and were able to deal with the new experiences in their workplace easily despite their feeling unsupported. The transition from medical student to practicing physician in real-world clinical settings is a significant challenge. They often experience significant stress during their clinical practice. This period of clinical training usually is case-based hands-on learning with real patients. This can lead to significant stress for graduating students, as they often feel unprepared for the multitasking responsibilities and heavy workload they face [26]. Other studies suggest that the cause of unpreparedness is due to lack of hands-on practice [27, 28]. Fortunately, new clinically oriented assessment tools, such as the Objective Structured Clinical Examination (OSCE), Direct Observation of Procedural Skills (DOPS), and Mini Clinical Evaluation Exercise (Mini-CEX) have been adopted by most of medical schools [29-31]. On the other hand, males reported feeling disadvantaged due to their ethnic background and felt more supported during their placements compared to females. In contrast, a paper published in England indicates that racism remains a significant issue in British schools, with progress in that area being the exception rather than the norm [32]. Furthermore, a longitudinal study conducted in the United States from 2010 to 2014 revealed that racism in American medical schools manifested at multiple levels, highlighting the need for strategies to eliminate structural racism within these institutions [33]. The study showed a statistically significant association between citizenship and feeling disadvantaged because of ethnic background. Foreign students were feeling disadvantaged because of their ethnic background.
The difficulty in feeling integrated can be attributed to the mixed Arab-African Sudanese ethnic background, which may prevent some individuals from fully integrating into Sudanese society. Additionally, foreign students may find it challenging to develop communication with patients due to factors in the host environment, such as cultural differences, social behaviors, and language barriers. This issue is not unique to Sudan; discriminatory treatment has also been reported among international students enrolled in American colleges and universities [34]. Given that the presence of dental students from diverse ethnic backgrounds can significantly enrich classroom cultural diversity and the overall academic environment, it is essential to foster integration among students through social support services and cultural events [35]. In recent years, global interconnectedness through trade, technology, and education has increased significantly. Moreover, the Arab Spring uprisings in some countries have led to widespread migration within the region, contributing to a substantial growth in the international student population at Sudanese universities. While international students present challenges, they also offer valuable opportunities.
Regarding the most impactful HC scenarios, having a positive role model doctor and the aspiration to develop strong patient-doctor skills were identified as the top two influential scenarios. Our finding aligns with previous research indicating the crucial role of medical teachers and staff in fostering the professional identity of medical students and preparing them for future medical careers. Students' perception of their clinical tutor's behavior, interactions, work ethics, and skills can significantly influence their choice of clinical field for residency training [36-38]. Role models are often used by medical teaching staff to impart professional values, attitudes, and behaviors to their students as part of the informal medical training curriculum [36, 39]. In our culture, a role model doctor is perceived as one who establishes a strong connection with their patients and their families, demonstrating thoughtfulness and fostering extended social relationships. This area needs further studies to elaborate differences between cultures. The second impactful scenario was inspiration to develop a patient-doctor relationship. The doctor-patient relationship is a consensual agreement where the patient seeks the physician's help, the physician accepts them as a patient, respects their autonomy, maintains confidentiality, explains treatment options, obtains informed consent, and provides the best care [40]. Doctor-patient skills are fundamental elements for high-quality healthcare. A systematic review including qualitative and quantitative studies concluded that various aspects of the doctor-patient relationship including communication, significantly impact both objective and subjective health outcomes [41]. In a recent study among dental students at Babol University of Medical Sciences (Iran), Students considered interaction and communication between the professors, students, and staff as crucial themes within the HC (20). Acknowledging the complexity of the doctor-patient relationship and its variations across cultures and backgrounds, educators have developed a range of curricula to teach students how to effectively interact with diverse patient populations [42]. The final most impactful scenario noted was the need to compete with other medical students, which aligns with findings from a study conducted among medical students in Pakistan [19]. While competition can be a powerful motivator, encouraging individuals to reach their highest potential, it can also have unfavorable effects if it goes too far. Kusnoor et al. highlights the negative impact of student competition on medical education and patient care [43]. Students facing time pressure and high competition may neglect some physical exams and pertinent historical information, potentially leading to costly mistakes.
Moreover, competition can negatively affect medical students' empathy toward patients due to burnout and stress, as they tend to prioritize task completion over patient care [44]. To foster intrinsic motivation among students, learning programs should emphasize collaborative and multifaceted teaching and learning strategies rather than competitive and simplistic approaches [45]. One potential limitation of this study is that it was conducted at a single governmental university in Sudan, which may restrict the generalizability of the findings, as they may not be representative of dental education as a whole. Additionally, this was a cross-sectional study administered to students all at once; however, as students’ encounter various experiences, their perceptions may evolve.
Conclusion
The study revealed that the most frequently observed positive scenario among students was a positive patient-doctor consultation (60%), while the least observed scenario was related to high professional standards in their learning environments (25%). In terms of negative scenarios, the most commonly reported issue was discriminatory attitudes in learning environments (52%), whereas ethnic and gender discrimination were the least frequent at 7% and 9%, respectively. This study provides a foundational understanding of the perceptions of Al-Neelain dental students regarding the HC. Further research is needed to explore the characteristics of a positive role model in accordance with cultural values in order to enhance the HC. Additionally, essential concepts of the hidden curriculum should be incorporated into the written curriculum, along with effective faculty training.
Ethical considerations
Approval for the research proposal and ethical clearance were obtained from the Sudan Medical Specialization Board Ethical Committee (SMSB-REC-13.9.2021). Participant agreement was secured through informed consent, which involved explaining the research title and purpose in clear and simple terms.
Only data relevant to the study's purpose was collected, and confidentiality was maintained throughout the research process.
Artificial intelligence utilization for article writing
Artificial intelligence was not used to write the article
Acknowledgment
We gratefully acknowledge all the faculty and members of the Educational Development Center (EDC) at Sudan Medical Speciation Board (SMSB) for being a great help throughout our study period. The authors would also like to thank The faculty of Dentistry (Al-Nileen University) and students who participated in the study.
Conflict of interest statement
The authors report no conflicts of interest in this work.
Author contributions
Conceptualization and Planning: SAA, BH, AHA, Data Collection: SAA, BH, Data Analysis: SAA, BH, Project Administration: SAA, BH, Resources: SAA, BH, Writing - Original Draft: SAA, BH, AHA, Writing - Review & Editing: SAA, BH, AHA
Funding
The work was conducted as a part of the health professional education program at the Sudan Medical Speciation Board (SMSB), and no grants or financial support were received.
Data availability statement
All data collected for this study will be available upon request.
Background & Objective: The Hidden Curriculum (HC) represents the cultural process of medical training, where students acquire attitudes and values. Understanding the HC enables educators to develop more impactful learning experiences. Therefore, this study aims to assess the perceptions of Al-Neelain University dental students regarding the frequency and impact of positive and negative aspects of the HC.
Materials & Methods: A cross-sectional study was conducted among a randomly selected sample of fifth-year dental students at Al-Neelain University (Sudan). Data were collected using the self-administered Hidden Informal Curriculum Assessment Tool (HICAT). The data were analyzed using the Mann-Whitney U test, Kruskal-Wallis test, and McNemar test.
Results: The response rate was 100% (81 out of 81), with 70.3% of respondents identifying as female. Approximately 53% of the respondents were single, and 86.4% were citizens. The most commonly reported positive scenario was a satisfactory patient-doctor consultation, noted by 60% of participants. In contrast, the least frequently observed positive scenario was the presence of high professional standards in their learning environments, reported by only 25%. On the negative side, the most frequently cited issue was discriminatory attitudes in learning environments, affecting 52% of respondents. Conversely, ethnic discrimination and gender discrimination were the least frequently reported negative scenarios, at 7% and 9%, respectively. Data revealed a statistically significant association between perceptions of certain HC scenarios and gender (p = 0.047), Citizenship (p = 0.045), and social status (p = 0.003). The top two influential scenarios identified were having a positive role model doctor and developing strong patient-doctor skills.
Conclusion: Respondents frequently reported positive patient-doctor consultations, while discriminatory attitudes in learning environments were the most common negative scenario. Understanding students' perceptions of healthcare is essential, as it can help reinforce positive aspects and improve negative ones in the future.
Introduction
The curriculum is the practical application of all educational concepts [1], including null, social, and received curricula [2]. The Hidden Curriculum (HC) refers to the unwritten, implicit, unofficial, and unintended lessons, values, and perspectives students acquire during their undergraduate studies, alongside the formal aspects of education [3, 4]. According to its focus, HC can be classified into two types: A cold curriculum, which emphasizes redundancy and offers low reward value, and a hot curriculum, which prioritizes high-reward elements such as behaviors, norms, values, gender roles, and political preferences. The hot curriculum is primarily learned through direct reinforcement and identification [5-7]. Bloom's redundancy theory posits that the HC, when consistently presented over time, has a greater impact on students' memory than the manifest curriculum [8]. Furthermore, the effectiveness of learning through redundant information largely depends on how compatible that information is with the learner's cognitive structures and its high reward value [5]. Furthermore, previous research has identified a positive and significant correlation between elements of the HC and the level of academic achievement attained by students [9]. In the medical field, including medicine and dentistry, the HC plays a crucial role in the development of physicians. As opposed to the formal curriculum that occurs in the classroom through lectures, the HC exemplifies the ‘‘cultural process’’ of medical training through the socialization of physicians, as they internalize the behaviors, attitudes, and values that are modeled to them in the ‘‘moral community’’ of medical school. This process starts early in the first year of training and continues throughout residency [10]. The elements of HC include providing role models to emulate, establishing medical ethical standards, implementing rules and regulations, introducing medical terminology and jargon, fostering professionalism, and understanding the power hierarchy within medicine. The effectiveness of these elements can be positively or negatively influenced by the manner in which the HC is communicated [11-13]. Medical schools prepare students for careers in medicine by integrating cognitive knowledge, role modeling, organizational culture, stereotyping, and professional attire, all of which contribute to the development of professionalism and professional identity [14]. The HC is a subject of ongoing debate, with some advocating for its positive aspects while others point out its potential negative effects [15]. Understanding the HC significantly enhances the teaching staff's attitudes toward students and trainees, as they become more aware of its influence and importance. Without this awareness, they may send harmful social beliefs and ideas, hindering social change [16]. This study aims to assess the perceptions of fifth-year dental students at Al-Neelain University regarding the practice and impact of the HC. The findings from this study will be instrumental in identifying gaps that need to be addressed in the HC from the students' perspectives.
Materials & Methods
Design and setting(s)
A descriptive cross-sectional study was conducted at the Faculty of Dentistry at Al-Neelain University, which was established in 2005.It has a distinct curriculum with clear goals and vision towards society; it includes a total of 11 semesters. The faculty has 12 departments in various dental specialties. The faculty offers students advanced training in dentistry through clinics and industrial replacement laboratories. They participate in activities like therapeutic days and educational visits to achieve the college's vision. Students receive early clinical training along with comprehensive patient care. The study was conducted from September 2021 to June 2022.
Participants and sampling
The study focused on undergraduate fifth-year students at the Faculty of Dentistry at Al-Neelain University. It included both female and male fifth-year students who were registered in the bachelor's degree program in dentistry, as well as foreign students. Students who were not registered for courses during the study period were excluded. According to the records from the Al-Neelain University Faculty of Dentistry, there are 102 students enrolled in the fifth year. The minimum sample size required for the study was calculated to be 81, using the Open-Source Epidemiologic Statistics for Public Health Version 3.01 online calculator, with a confidence level of 95% [17]. For sampling, systematic random sampling was employed, utilizing the list of fifth-year students as the sampling frame. The sampling interval was determined by dividing the total population size (N = 102) by the desired sample size [18]. The first participant was selected by simple random sampling.
Tools/Instruments
The data were collected online using a self-administered questionnaire as a data collection tool. The questionnaire consisted of two sections. The first section examined the sociodemographic characteristics of the participating students. The second section contained the Hidden Curriculum Assessment Tool (HICAT) [18]. The questionnaire consisted of four sections and comprised 27 items. The first section consisted of four questions to explore the socio-demographic characteristics of the participants.
The second section outlines ten positive HC scenarios that students may have experienced during their studies. The third section features ten negative HC scenarios.
The fourth section, titled "Impact Rating," requests students to identify the three scenarios that had the most significant impact on them during their clinical rotations, selecting from the previously mentioned 20 scenarios. This section emphasizes the depth of the impact rather than the frequency with which the scenarios were encountered. In the first and second sections of the questionnaire (comprising ten positive and ten negative HC scenarios), participants' responses were rated using a modified 4-point Likert scale: 1. Usually/Always, 2. Half the time, 3. Never/Occasionally, 4. Not applicable. Permission to use HICAT was obtained via email correspondence from Prof. Paul McGurgan, the originator of the questionnaire at the University of Western Australia. HICAT is used to quantify both the frequency of positive and negative aspects of the HC and the impact of these experiences on dental students. It was developed in two main steps. Initially, the authors developed a range of educational scenarios related to the HC based on a literature review, intending to capture both positive and negative aspects. Subsequently, a focus group of medical students reviewed and refined these scenarios, selecting the most relevant ones based on their individual experiences. The most common scenarios (ten negative and ten positive) served as the foundation for the instrument. After that, the instrument was piloted on a second rotation of medical students to ensure its user-friendliness and internal validity [18]. To ensure validity within our context, the questionnaire was reviewed by a panel of four experts who critically evaluated its content and relevance. The instrument demonstrated acceptable reliability, with a Cronbach’s Alpha of 0.682.
Data collection methods
Before administering the HICAT questionnaire, fifth-year dental students were provided with information about the study. This included a definition of the HC, assurances of confidentiality, and a statement indicating that participation was voluntary and would not affect their academic outcomes. The online HICAT questionnaire was created using Google Forms and was subsequently hosted online via a unique URL. Pre-selected study participants were invited individually to participate through their contact information. Participants’ responses were automatically collected and stored in a Google Drive.
Data analysis
The Statistical Package for Social Sciences (SPSS) version 17 was utilized for coding, entering, and analyzing participants' responses. Descriptive analysis was conducted to summarize the data, with frequency and percentages calculated for categorical variables, and mean and standard deviation employed for continuous variables. Non-parametric statistics were used to identify significant differences or associations between independent and dependent variables. The non-parametric tests applied included the Mann-Whitney U test, Kruskal-Wallis test, and McNemar test. A p-value of 0.05 or less was considered statistically significant.
Results
The response rate was 100% (81 out of 81 participants). As shown in Table 1, the majority of respondents were females (70.3%). More than half (53%) of the respondents were single, and a significant proportion (86.4%) were citizens. Additionally, all respondents identified as Muslims (100%).
Table 1. Sociodemographic characteristics of participants (n = 81)
As shown in Table 2, the most highly valued positive scenarios reported by respondents included observing positive patient-doctor consultations (60%), followed by witnessing health professionals educating patients about their conditions (56%), encountering health professionals regarded as positive role models (49%), and observing staff acknowledging their limitations (49%). The least frequent items observed were observing high professional standards in their learning environments (25%) and observing patients being treated as unique individuals (28%). Regarding the negative HC scenarios (Table 3), the most frequent scenario was discriminatory attitudes in learning environments (52%). The least frequent negative scenarios were discrimination due to ethnic background (7%) or gender (9%), followed by feeling humiliated by a supervisor (21%). Participants' responses were analyzed in relation to their demographic data to identify potential associations between demographic factors and perceptions of HC scenarios. Among positive and negative scenarios, only those demonstrating a significant association between demographic factors and student responses were discussed. Females were more often asked to undertake unsupervised tasks whilst feeling unconfident (p = 0.047) and were more troubled by the experiences encountered than their male counterparts (p = 0.015). On the other hand, males reported feeling disadvantaged due to their ethnic background more often than females (p = 0.047) and felt more supported during their placements (p = 0.045). Additionally, data analysis revealed a statistically significant association between citizenship and three HC scenarios. Citizens were more frequently asked to undertake unsupervised tasks while feeling unconfident
(p = 0.045) and were observed to develop doctor-patient skills more often than foreign students (p = 0.018). In contrast, foreign students felt disadvantaged because of their ethnic background (p = 0.001).
Table 2. Responses of the participants to the positive hidden curriculum scenarios

Abbreviations: n, number of participants; %, percentage.
Table 3. Responses of the participants to the negative hidden curriculum scenarios

Abbreviations: n, number of participants; %, percentage.
The social status of the respondents was significantly associated only with doctor-patient consultations (p = 0.035) (Table 4). Respondents reported two positive scenarios and one negative scenario as their three most influential HC scenarios. The most impactful positive scenarios identified were “I have encountered health professionals I consider to be positive role models” and “I was inspired to develop my doctor-patient skills.” In contrast, the most frequently reported negative scenario was “I needed to compete with other dental students” (Table 5).
Furthermore, data analysis showed a significant difference between the most impactful negative scenario and each of the two most frequently cited positive scenarios, with p-values of 0.046 and 0.040, respectively (Table 6).
Table 4. Association between sociodemographic characteristics of the participants and the hidden curriculum scenarios

Notes: *Mann-Whitney U test was used to compare assocation between gender, citizinship and the hidden curriculum scenarios, **Kruskal-Wallis test was used to compare the association between social status and and the hidden curriculum scenarios.
Abbreviations: N, frequency ;Sig, statistical significance; p, probability -value; Z, z-score (standardized Mann-Whitney U test test statistic); H, Kruskal-Wallis test statistic
Table 5. The participants' rankings of hidden curriculum scenarios

Note: Times selected, the frequency with which a specific scenario was chosen by the participants; Percent (%), the proportion of times a given experience was selected based on n = 243; percent of respondents(%), the proportion of respondents who selected each experience based on n = 81, acknowledging that each respondent could select more than one experience.
Table 6. Comparison between the three most impactful scenarios

Note: McNemar test used to compare between the most impactful scenarios, the three most impactful senarios are having a positive role model doctor, the aspiration to develop strong patient-doctor skills and the need to compete with other medical students; Times selected, the number of times each experience was reported across all responses.
Abbreviations: Sig, statistical significance; p, probability -value; χ² , Chi -square statistic.
Abbreviations: Sig, statistical significance; p, probability -value; χ² , Chi -square statistic.
Discussion
This study aimed to identify positive aspects of the HC that can be reinforced, while also identifying negative aspects that should be avoided or reshaped. The ultimate goal is to improve the cultures of both the health professions and education. The HICAT was utilized to measure both the frequency of dental students' experiences with HC scenarios and the impact of these experiences.This tool is useful for evaluating medical students in clinical and educational settings to determine their strengths and weaknesses [18]. Among the ten positive scenarios, the majority of students in this study observed a positive attitude during patient-doctor consultations. Patients expressed a desire to be informed about their condition and to receive support from their doctors. These findings align with results from a study conducted at the University of Western Australia, where 93% of students agreed on the same scenarios [18]. Additionally, our findings are partially in line with the findings of a study conducted in Pakistan, where medical students highly valued the demonstration of high professional standards, the exhibition of positive role modeling, and positive doctor-patient relationships [19]. Moreover, a qualitative study among dental students in Iran demonstrated the importance of considering a professor's professional behavior and their role as a role model [20]. The least frequently observed positive scenarios were “observing patients being treated as unique individuals” and “observing high professional standards in the learning environments.” Our findings contrast with a study conducted in Pakistan, where the least valued items were observing staff admitting their limitations and witnessing health professionals effectively managing complex cases in a positive manner [19]. These differences could be attributed to differences in participants' social culture. Professionalism is a culture‑dependent ability and training for all professional responsibilities is a difficult task that comes with many obstacles as stated in many studies [21, 22]. The gap between knowledge and practice, a lack of emphasis on continuous professional education, the normalization of certain behaviors, and the neglect of the importance of being observed as a role model were identified as justifications for these findings, which can also be relevant to the Sudanese context [23]. Regarding negative scenarios, the most common experience reported was witnessing discriminatory attitudes in learning environments (52%). This finding aligns with a survey conducted among internal medicine trainees in the United States, where nearly two-thirds of respondents reported observing unequal treatment of patients from various backgrounds [24]. Discriminatory attitudes in the learning environment can negatively affect students' educational outcomes. Efforts should be directed to address and implement strategies to eliminate such attitudes and maintain health equity. Furthermore, there is a need to train dental students and educators on how to effectively respond to any form of prejudiced attitudes. Conversely, the least frequently observed negative scenarios included disadvantages faced by students due to their gender (9%) or ethnic background (7%). This latter finding is somewhat unexpected, given the ethnic diversity in the country and the reported discrimination claims and conflicts between tribes. Additionally, the issue of gender equity within the educational environment is noteworthy. Education for women in Sudan began as early as 1903 [25], and since then, women have made significant strides in education and have become major contributors to society. Data analysis showed a statistically significant association between gender and confidence to perform unsupervised tasks. Females were more often asked to undertake unsupervised tasks whilst feeling unconfident. Similarly, females were observed to be troubled half of the time by the new experiences they encounter (p = 0.015) than their male counterparts. The majority of them never had that feeling and were able to deal with the new experiences in their workplace easily despite their feeling unsupported. The transition from medical student to practicing physician in real-world clinical settings is a significant challenge. They often experience significant stress during their clinical practice. This period of clinical training usually is case-based hands-on learning with real patients. This can lead to significant stress for graduating students, as they often feel unprepared for the multitasking responsibilities and heavy workload they face [26]. Other studies suggest that the cause of unpreparedness is due to lack of hands-on practice [27, 28]. Fortunately, new clinically oriented assessment tools, such as the Objective Structured Clinical Examination (OSCE), Direct Observation of Procedural Skills (DOPS), and Mini Clinical Evaluation Exercise (Mini-CEX) have been adopted by most of medical schools [29-31]. On the other hand, males reported feeling disadvantaged due to their ethnic background and felt more supported during their placements compared to females. In contrast, a paper published in England indicates that racism remains a significant issue in British schools, with progress in that area being the exception rather than the norm [32]. Furthermore, a longitudinal study conducted in the United States from 2010 to 2014 revealed that racism in American medical schools manifested at multiple levels, highlighting the need for strategies to eliminate structural racism within these institutions [33]. The study showed a statistically significant association between citizenship and feeling disadvantaged because of ethnic background. Foreign students were feeling disadvantaged because of their ethnic background.
The difficulty in feeling integrated can be attributed to the mixed Arab-African Sudanese ethnic background, which may prevent some individuals from fully integrating into Sudanese society. Additionally, foreign students may find it challenging to develop communication with patients due to factors in the host environment, such as cultural differences, social behaviors, and language barriers. This issue is not unique to Sudan; discriminatory treatment has also been reported among international students enrolled in American colleges and universities [34]. Given that the presence of dental students from diverse ethnic backgrounds can significantly enrich classroom cultural diversity and the overall academic environment, it is essential to foster integration among students through social support services and cultural events [35]. In recent years, global interconnectedness through trade, technology, and education has increased significantly. Moreover, the Arab Spring uprisings in some countries have led to widespread migration within the region, contributing to a substantial growth in the international student population at Sudanese universities. While international students present challenges, they also offer valuable opportunities.
Regarding the most impactful HC scenarios, having a positive role model doctor and the aspiration to develop strong patient-doctor skills were identified as the top two influential scenarios. Our finding aligns with previous research indicating the crucial role of medical teachers and staff in fostering the professional identity of medical students and preparing them for future medical careers. Students' perception of their clinical tutor's behavior, interactions, work ethics, and skills can significantly influence their choice of clinical field for residency training [36-38]. Role models are often used by medical teaching staff to impart professional values, attitudes, and behaviors to their students as part of the informal medical training curriculum [36, 39]. In our culture, a role model doctor is perceived as one who establishes a strong connection with their patients and their families, demonstrating thoughtfulness and fostering extended social relationships. This area needs further studies to elaborate differences between cultures. The second impactful scenario was inspiration to develop a patient-doctor relationship. The doctor-patient relationship is a consensual agreement where the patient seeks the physician's help, the physician accepts them as a patient, respects their autonomy, maintains confidentiality, explains treatment options, obtains informed consent, and provides the best care [40]. Doctor-patient skills are fundamental elements for high-quality healthcare. A systematic review including qualitative and quantitative studies concluded that various aspects of the doctor-patient relationship including communication, significantly impact both objective and subjective health outcomes [41]. In a recent study among dental students at Babol University of Medical Sciences (Iran), Students considered interaction and communication between the professors, students, and staff as crucial themes within the HC (20). Acknowledging the complexity of the doctor-patient relationship and its variations across cultures and backgrounds, educators have developed a range of curricula to teach students how to effectively interact with diverse patient populations [42]. The final most impactful scenario noted was the need to compete with other medical students, which aligns with findings from a study conducted among medical students in Pakistan [19]. While competition can be a powerful motivator, encouraging individuals to reach their highest potential, it can also have unfavorable effects if it goes too far. Kusnoor et al. highlights the negative impact of student competition on medical education and patient care [43]. Students facing time pressure and high competition may neglect some physical exams and pertinent historical information, potentially leading to costly mistakes.
Moreover, competition can negatively affect medical students' empathy toward patients due to burnout and stress, as they tend to prioritize task completion over patient care [44]. To foster intrinsic motivation among students, learning programs should emphasize collaborative and multifaceted teaching and learning strategies rather than competitive and simplistic approaches [45]. One potential limitation of this study is that it was conducted at a single governmental university in Sudan, which may restrict the generalizability of the findings, as they may not be representative of dental education as a whole. Additionally, this was a cross-sectional study administered to students all at once; however, as students’ encounter various experiences, their perceptions may evolve.
Conclusion
The study revealed that the most frequently observed positive scenario among students was a positive patient-doctor consultation (60%), while the least observed scenario was related to high professional standards in their learning environments (25%). In terms of negative scenarios, the most commonly reported issue was discriminatory attitudes in learning environments (52%), whereas ethnic and gender discrimination were the least frequent at 7% and 9%, respectively. This study provides a foundational understanding of the perceptions of Al-Neelain dental students regarding the HC. Further research is needed to explore the characteristics of a positive role model in accordance with cultural values in order to enhance the HC. Additionally, essential concepts of the hidden curriculum should be incorporated into the written curriculum, along with effective faculty training.
Ethical considerations
Approval for the research proposal and ethical clearance were obtained from the Sudan Medical Specialization Board Ethical Committee (SMSB-REC-13.9.2021). Participant agreement was secured through informed consent, which involved explaining the research title and purpose in clear and simple terms.
Only data relevant to the study's purpose was collected, and confidentiality was maintained throughout the research process.
Artificial intelligence utilization for article writing
Artificial intelligence was not used to write the article
Acknowledgment
We gratefully acknowledge all the faculty and members of the Educational Development Center (EDC) at Sudan Medical Speciation Board (SMSB) for being a great help throughout our study period. The authors would also like to thank The faculty of Dentistry (Al-Nileen University) and students who participated in the study.
Conflict of interest statement
The authors report no conflicts of interest in this work.
Author contributions
Conceptualization and Planning: SAA, BH, AHA, Data Collection: SAA, BH, Data Analysis: SAA, BH, Project Administration: SAA, BH, Resources: SAA, BH, Writing - Original Draft: SAA, BH, AHA, Writing - Review & Editing: SAA, BH, AHA
Funding
The work was conducted as a part of the health professional education program at the Sudan Medical Speciation Board (SMSB), and no grants or financial support were received.
Data availability statement
All data collected for this study will be available upon request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2024/09/17 | Accepted: 2025/08/31 | Published: 2025/10/1
Received: 2024/09/17 | Accepted: 2025/08/31 | Published: 2025/10/1
References
1. Prideaux D. ABC of learning and teaching in medicine: Curriculum design. BMJ. 2003;326(7383):268-70. [DOI:10.1136/bmj.326.7383.268] [PMID] []
2. Wilson LO. Types of curriculum-detailed explanations of the multiple types of curriculum [Internet]. The Second Principle; 2015. Available from: [cited 2021 Aug 2].
3. Mossop L, Dennick R, Hammond R, Robbé I. Analysing the hidden curriculum: use of a cultural web. Med Educ. 2013;47(2):134-43. [DOI:10.1111/medu.12072] [PMID] []
4. Lawrence C, Mhlaba T, Stewart KA, Moletsane R, Gaede B, Moshabela M. The hidden curricula of medical education: a scoping review. Acad Med. 2018;93(4):648-56. [DOI:10.1097/ACM.0000000000002004] [PMID] []
5. Assor A, Gordon D. The implicit learning theory of hidden‐curriculum research. J Curric Stud. 1987;19(4):329-39. [DOI:10.1080/0022027870190404]
6. Boldizar JP. Assessing sex typing and androgyny in children: the children's sex role inventory. Dev Psychol. 1991;27(3):505. [DOI:10.1037/0012-1649.27.3.505]
7. Maccoby EE. Social development: psychological growth and the parent-child relationship. New York: Harcourt Brace Jovanovich; 1980.
8. Bloom BS. Bloom, Benjamin S., "Innocence in Education," School Review, 80 (May, 1972), 333-352 [Internet]. 1972. Available from: [cited 2021 Sep 10]. [DOI:10.1086/443036]
9. Nami Y, Marsooli H, Ashouri M. Hidden curriculum effects on university students' achievement. Procedia Soc Behav Sci. 2014;114:798-801. [DOI:10.1016/j.sbspro.2013.12.788]
10. Bandini J, Mitchell C, Epstein-Peterson ZD, Amobi A, Cahill J, Peteet J, et al. Student and faculty reflections of the hidden curriculum: how does the hidden curriculum shape students' medical training and professionalization? Am J Hosp Palliat Care. 2017;34(1):57-63. [DOI:10.1177/1049909115616359] [PMID]
11. Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students' perceptions of teaching. BMJ. 2004;329(7469):770-3. [DOI:10.1136/bmj.329.7469.770] [PMID] []
12. Hendelman W, Byszewski A. Formation of medical student professional identity: categorizing lapses of professionalism, and the learning environment. BMC Med Educ. 2014;14:1-10. [DOI:10.1186/1472-6920-14-139] [PMID] []
13. Witman Y. What do we transfer in case discussions? The hidden curriculum in medicine. Perspect Med Educ. 2014;3(2):113-23. [DOI:10.1007/S40037-013-0101-0] [PMID] []
14. Brown MEL, Coker O, Heybourne A, Finn GM. Exploring the hidden curriculum's impact on medical students: professionalism, identity formation and the need for transparency. Med Sci Educ. 2020;30(3):1107-21. [DOI:10.1007/s40670-020-01021-z] [PMID] []
15. Monrouxe LV. Identity, identification and medical education: why should we care? Med Educ. 2010;44(1):40-9. [DOI:10.1111/j.1365-2923.2009.03440.x] [PMID]
16. Jerald CD. School culture [Internet]. Center for Comprehensive School Reform and Improvement; 2006 Dec. Available from: [cited 2024 Sep 3].
17. Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version [Internet]. 2013. Available from: [cited 2024 Aug 19].
18. McGurgan P, Carmody D, Tregonning A. Measuring the "iceberg"-quantifying the hidden and informal curriculum in clinical rotations using the hidden informal curriculum assessment tool (HICAT). MedEdPublish. 2015;5(2):1-9. [DOI:10.15694/mep.2015.005.0002]
19. Afridi A, Sethi A, Ahmed F, Kashif L. Assessment of hidden curriculum during clinical rotations of year 4 mbbs students using hidden informal curriculum assessment tool (HICAT). J Med Sci. 2020;28(4):352-5. [DOI:10.52764/jms.20.28.4.10]
20. Shakerinejad M, Gholamnia-Shirvani Z, Khodadadi E, Nikpour M. Dental students' experience of hidden curriculum: a qualitative study. J Med Educ Dev. 2024;17(54):31-43. [DOI:10.61186/edcj.17.54.31]
21. Iramaneerat C. Instruction and assessment of professionalism for surgery residents. J Surg Educ. 2009;66(3):158-62. [DOI:10.1016/j.jsurg.2009.03.031] [PMID]
22. Kirk LM. Professionalism in medicine: definitions and considerations for teaching. In: Proceedings of Baylor University Medical Center; 2007 Jan 1; 20(1):13-16. Dallas: Baylor University Medical Center. [DOI:10.1080/08998280.2007.11928225] [PMID] []
23. Alipour F, Shahvari Z, Asghari F, Samadi S, Amini H. Educational system defects and observing professional behavior: a qualitative study. J Educ Health Promot. 2019;8:162. [DOI:10.4103/jehp.jehp_22_19] [PMID] []
24. Sotto-Santiago S, Mac J, Slaven J, Maldonado M. A survey of internal medicine residents: their learning environments, bias and discrimination experiences, and their support structures. Adv Med Educ Pract. 2021;23:697-703. [DOI:10.2147/AMEP.S311543] [PMID] []
25. Bedri AM. Reflections on the struggle for girls' education in Sudan. In: Karlsson J, Msibi T, editors. Gendered voices: reflections on gender and education in South Africa and Sudan. Rotterdam: SensePublishers; 2013. p. 25-40. [DOI:10.1007/978-94-6209-137-5_3]
26. Monrouxe LV, Grundy L, Mann M, John Z, Panagoulas E, Bullock A, et al. How prepared are UK medical graduates for practice? A rapid review of the literature 2009-2014. BMJ Open. 2017;7(1):e013656. [DOI:10.1136/bmjopen-2016-013656] [PMID] []
27. Yu SR, Cheng YC, Tseng HM, Chang YC, Ma SD, Huang CD, et al. Undergraduates' preparedness for practice is associated with professional identity and perception of educational environment: a validation study. Biomed J. 2021;44(4):495-503. [DOI:10.1016/j.bj.2020.04.009] [PMID] []
28. Goldacre MJ, Taylor K, Lambert TW. Views of junior doctors about whether their medical school prepared them well for work: questionnaire surveys. BMC Med Educ. 2010;10(1):78. [DOI:10.1186/1472-6920-10-78] [PMID] []
29. Chou JY, Chiu CH, Lai E, Tsai D, Tzeng CR. Medical education in Taiwan. Med Teach. 2012;34(3):187-91. [DOI:10.3109/0142159X.2012.652238] [PMID]
30. Nikendei C, Weyrich P, Jünger J, Schrauth M. Medical education in Germany. Med Teach. 2009;31(7):591-600. [DOI:10.1080/01421590902833010] [PMID]
31. Dezee KJ, Artino AR, Elnicki DM, Hemmer PA, Durning SJ. Medical education in the United States of America. Med Teach. 2012;34(7):521-5. [DOI:10.3109/0142159X.2012.668248] [PMID]
32. Gillborn D. Citizenship, 'Race' and the hidden curriculum. Int Stud Sociol Educ. 1992;2(1):57-73. [DOI:10.1080/0962021920020104]
33. Phelan SM, Burke SE, Cunningham BA, Perry SP, Hardeman RR, Dovidio JF, et al. The effects of racism in medical education on students' decisions to practice in underserved or minority communities. Acad Med. 2019;94(8):1178-89. [DOI:10.1097/ACM.0000000000002719] [PMID]
34. de Araujo AA. Adjustment issues of international students enrolled in American colleges and universities: a review of the literature. High Educ Stud. 2011;1(1):2-8. [DOI:10.5539/hes.v1n1p2]
35. Martirosyan NM, Bustamante RM, Saxon DP. Academic and social support services for international students: current practices. J Int Stud. 2019;9(1):172-91. [DOI:10.32674/jis.v9i1.275]
36. Swick HM, Szenas P, Danoff D, Whitcomb ME. Teaching professionalism in undergraduate medical education. JAMA. 1999;282(9):830-2. [DOI:10.1001/jama.282.9.830] [PMID]
37. Wright S. Examining what residents look for in their role models. Acad Med. 1996;71(3):290-2. [DOI:10.1097/00001888-199603000-00024] [PMID]
38. Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12:53-6.
https://doi.org/10.1007/s11606-006-0007-1 [DOI:10.1046/j.1525-1497.1997.12109.x] [PMID] []
39. Paice E, Heard S, Moss F. How important are role models in making good doctors? BMJ. 2002;325(7366):707-10. [DOI:10.1136/bmj.325.7366.707] [PMID] []
40. Chipidza FE, Wallwork RS, Stern TA. Impact of the doctor-patient relationship. Prim Care Companion CNS Disord. 2015;17(5):27354.
https://doi.org/10.4088/PCC.15m01840 [DOI:10.4088/PCC.15f01840]
41. Riedl D, Schüßler G. The influence of doctor-patient communication on health outcomes: a systematic review. Z Psychosom Med Psychother. 2017;63(2):131-50. [DOI:10.13109/zptm.2017.63.2.131] [PMID]
42. Wright SM, Carrese JA. Serving as a physician role model for a diverse population of medical learners. Acad Med. 2003;78(6):623-8. [DOI:10.1097/00001888-200306000-00013] [PMID]
43. Kusnoor AV. Cheating in medical school: the unacknowledged ailment. South Med J. 2013;106(8):479-83. [DOI:10.1097/SMJ.0b013e3182a14388] [PMID]
44. Osmosis. The negative effects of competition amongst medical students and 5 tips to overcome them [Internet]. 2022. Available from: [cited 2025 Jan 10].
45. Kirsch J, Spreckelsen C. Caution with competitive gamification in medical education: unexpected results of a randomised cross-over study. BMC Med Educ. 2023;23(1):259. [DOI:10.1186/s12909-023-04258-5] [PMID] []
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




