Sun, Feb 22, 2026
[Archive]
Volume 18, Issue 2 (2025)
J Med Edu Dev 2025, 18(2): 20-29 |
Back to browse issues page
Ethics code: IR.BUMS.REC.1402.478
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Farahi F, Amouzeshi Z, Nazari H, Oudi D. The effect of blended role-playing and reflective training on nursing students’ communication skills with depressed patients. J Med Edu Dev 2025; 18 (2) :20-29
URL: http://edujournal.zums.ac.ir/article-1-2276-en.html
URL: http://edujournal.zums.ac.ir/article-1-2276-en.html
1- Department of Nursing, School of Nursing and Midwifery, Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 434 kb]
(574 Downloads)
| Abstract (HTML) (1661 Views)
Full-Text: (176 Views)
Abstract
Background & Objective: Communicating with depressed patients is a crucial professional skill for nursing students, which they must learn during their studies. This study aimed to assess the effectiveness of blended training—incorporating both role-playing and reflective practice—on nursing students' communication skills in their interactions with depressed patients.
Materials & Methods: The present semi-experimental study was conducted in 2023 with a before and after two-group design. All sixth-semester nursing students at Torbat Jam Faculty of Medical Sciences were randomly selected and divided into two groups: an experimental group and a control group. The intervention included therapeutic communication skill training sessions with the role-playing and reflection blended method. The control group received the standard training method. Therapeutic communication skills in dealing with depressed patients before and after the intervention were evaluated by a communication skills questionnaire. Data were analyzed using the statistical software SPSS version 20, descriptive statistical tests and inferential tests (t-test, analysis of variance, and paired-t) at a significance level 0.05.
Results: The average communication skills scores before the intervention showed no statistically significant difference between the intervention and control groups (p > 0.05). However, the mean score of communication skills after the intervention was significantly different in the two groups (p < 0.05). The results also indicated that the mean communication skill score after the intervention significantly improved in the experimental group compared to before the intervention (p < 0.05). However, there was no statistically significant change in the mean communication skill score in the control group before and after the intervention (p > 0.05).
Conclusion: Educational system managers and planners are suggested to use a blend of these two methods to train nursing students' communication skills, especially in the psychiatric department and when dealing with depressed patients.
Depression has serious consequences for people's health, and the treatment team faces many challenges when communicating with a depressed patient. These patients provide less feedback during communication and participate less than other patients.
Following the reduction of the participation of these patients during communication, their adherence to the treatment regimen may also be affected, which threatens their health [7]. Thus, in dealing with these patients, using effective communication techniques for the treatment team members is especially important [8]. Also, effective communication between nurses and nursing students with depressed patients plays an important role in reducing stress and creating relaxation for them. The professional patient-student relationship as a source of support can affect the progress and development of an original and patient-centred therapeutic approach for better care of people with a mental health condition among students [9].
Recognizing that effective verbal and non-verbal communication skills are vital for enhancing treatment outcomes, fostering relationships with colleagues, patients, and their families, and navigating complex treatment situations for nurses and nursing students as a potential workforce for the future [10], teaching communication skills has become a key component of nursing education in recent years. Nursing students should be able to provide appropriate communication in the patient-caring process [11, 12].
Studies indicated that nursing students are unable to communicate effectively with patients, and many students are afraid of encountering patients and relatives with different backgrounds and personalities in mental health [13]. Additionally, communication skills are a vital yet often overlooked educational need for students in nursing programs. The research results emphasize that inefficient training leads to a deficit in communication skills in healthcare providers [13, 15] and holding appropriate training courses to develop the communication skills of healthcare providers is an important step toward improving these skills [14, 13].
Role-playing is one of the effective methods of teaching communication and social skills [16]. Role-playing is a form of simulation in which participants interact with a patient without the apprehension of potential risks associated with their care methods. In this method, a purposeful show is performed, and by discussing it, people can discuss their feelings, attitudes, and problem-solving strategies regarding the situation [17]. The reduction of time and cost required for training, improvement of decision-making and critical thinking skills, and increase of comprehensive self-confidence are among the advantages of this training method [16]. Despite the benefits of this method, in our country, role-playing is rarely used in medical science education, and information on the effectiveness of this method in teaching nursing students in Iran is limited [18, 19]. Another way to improve learning is reflective thinking. Reflective thinking is a thorough, ongoing, and active examination of one's beliefs and knowledge, utilizing personal justifications and inferences that help reinforce and solidify those opinions or beliefs [20]. The process of reflective thinking allows people to recall and review the experience and encourages them to search for and evaluate solutions in complex situations [16]. Reflection can lead to improving clinical reasoning skills and deep learning; thus, it is considered an important educational tool in the nursing profession [21].
In addition to improving knowledge and skills, reflection teaches learners the habit of critical thinking and learning, and therefore, it is considered an effective education method [22]. Reflective thinking helps students to improve their learning experiences during and after performing clinical skills and to realize their learning deficiencies through self-criticism [24, 23]. The numerous beneficial effects of role-playing and reflective thinking educational methods have been demonstrated individually.
Some research has considered these two educational methods complementary and concluded that combining them in teaching skills results in synergistic learning in the individual [24-26]. Despite numerous studies on each of these educational models and their effects, very little research has been conducted on the effect of blended training with role-playing and reflection methods on the communication skills of nursing students in dealing with depressed patients.
Materials & Methods
Design and setting(s)
This semi-experimental research uses a two-group design (intervention and control) with pre-test and post-test assessments. It began on July 16, 2023, and concluded on September 20, 2024.
Participants and sampling
The research population consisted of all sixth-semester nursing students at Torbat Jam Faculty of Medical Sciences, who were included in the study through a convenience non-random sampling method based on specific inclusion and exclusion criteria. The inclusion criteria included being a sixth-semester nursing student, passing the relevant theoretical and practical units so far, and not passing the internship unit in psychology. The exclusion criteria included being transfer students to the faculty and participating in communication skills training workshops. A total of 44 students participated in the study (Figure 1).
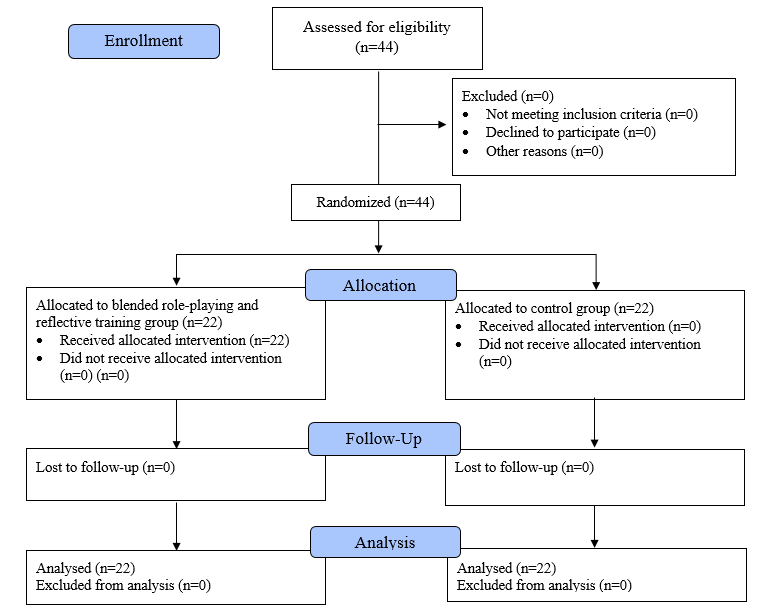
Figure 1. Flow chart of the study
Tools/Instruments
Data were collected using a demographic information questionnaire (age, gender, dormitory status, marital status, and nativeness) and a standard Interpersonal Communication Skills Scale (ASMA). This questionnaire was developed by Vakili et al. The initial questionnaire contains 43 items that fall into seven dimensions, including public communication skills, speaking skills, listening skills, interpretation and clarification skills, questioning skills, encouragement skills, and feedback skills. The options of this questionnaire are graded according to a 5-point Likert scale of 1 (very weak), 2 (weak), 3 (moderate), 4 (good) and 5 (very good). Vakili and his colleagues psychometrically evaluated this questionnaire in a study on the population of health workers in Zanjan. Based on the results of exploratory factor analysis, 30 items from this questionnaire were confirmed and placed in 7 areas of general communication skills (6 items), speaking skills (4), listening skills (4), interpretation and clarification skills (4), and questioning skills (4), encouragement and praise skill (4) and feedback skill (4). The reliability of the entire questionnaire in this study was reported using Cronbach's alpha 0.91 [27].
Data collection methods
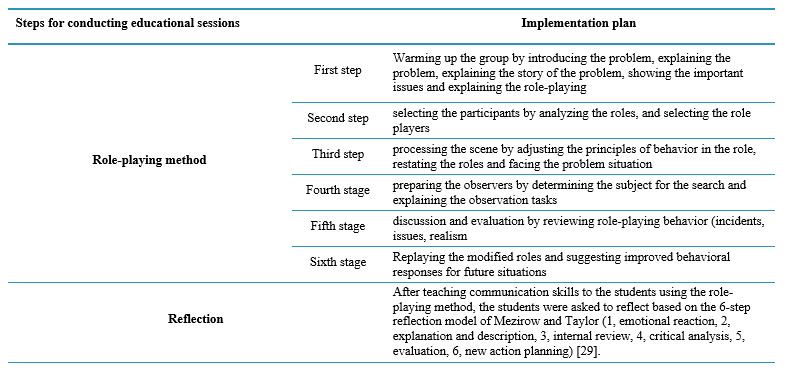
Sixth-semester nursing students with bachelor's degrees were assigned into two experimental and control groups using a simple random method to conduct the study. Communication skills were evaluated in both experimental and control groups before the intervention by completing a questionnaire. The control group received the usual theoretical and practical method of training communication skills with depressed patients. For the intervention group, the training was implemented in combination with role-playing and reflective thinking skills of communication skills with depressed patients. After the intervention, the communication skills of both the experimental and control groups were re-evaluated using the same measurement instrument. The intervention included training in the blended method of role-playing and reflective thinking. The role-playing training method was done in the form of a theoretical explanation of the problem, and then the roles and performing the role were determined by the students and feedback was provided to them. The method consisted of seven steps: the first step involved warming up the group by introducing the problem, explaining the situation, discussing the contextual story, highlighting key issues, and outlining the role-playing activities. The second step is selecting the participants by analyzing the roles and selecting the role players. The third step is processing the scene by adjusting the principles of behaviour in the role, restating the roles and facing the problem situation. The fourth stage prepares the observers by determining the subject for the search and explaining the observation tasks. The fifth stage is discussion and evaluation, which involves reviewing role-playing behaviour (incidents, issues, realism), discussing cases, and creating the next stage. sixth stage, re-playing by playing the modified roles and suggesting the following stages with more appropriate behaviours) [28]. After teaching communication skills to the students using the role-playing method, they were asked to reflect on their experiences based on the 6-step reflection model developed by Mezirow and Taylor (2009). The steps included: 1) emotional reaction, 2) explanation and description, 3) internal review, 4) critical analysis, 5) evaluation, and 6) new action planning. Students reflected on how to communicate with patients, the relevant information regarding patient interactions, their communication skills, and the outcomes of using these skills. They documented their reflections on a sheet organized according to Mezirow and Taylor's reflection model [29]. The researcher studied the students' writings, and appropriate feedback was provided to improve their learning (Table 1). All ethical considerations were considered when conducting the study. Obtaining permission from the University of Medical Sciences and the Institute of Medical Education to participate in the study, obtaining written informed consent from the research units to participate in the study, freedom to enter and exit the study, the anonymity of the questionnaires, and the emphasis on the confidentiality of information were taken into consideration.
Table 1. Mezirow and Taylor role play steps
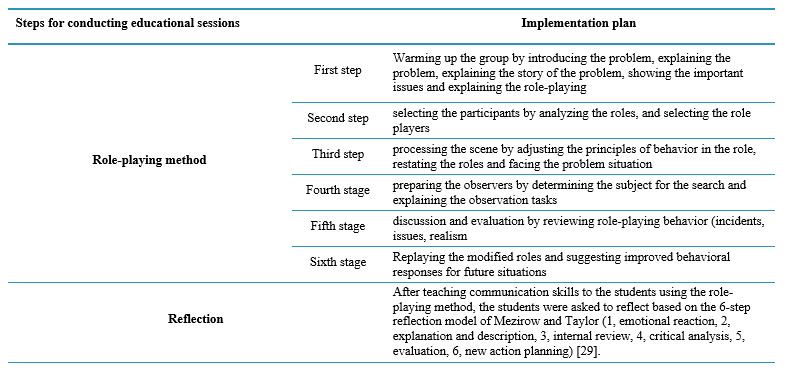
Table 2. Frequency, mean, and standard deviation of demographic characteristics of participants in the intervention and control groups
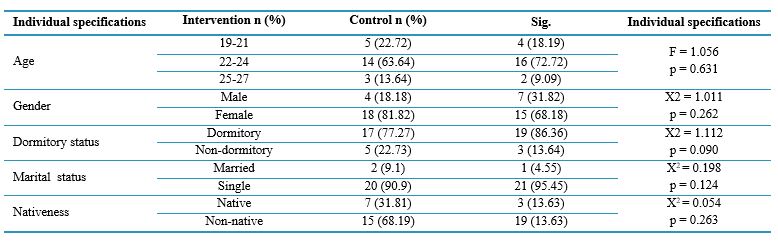
Note: ANOVA was used to compare quantitative demographic variables between groups, while the Chi-square test was used to compare qualitative variables.
Abbreviations: n, number of participants; SD, standard deviation; X2, Chi-square test; Sig., statistical significance; p, probability-value.
Table 3. Mean and standard deviation of students’ communication skills by demographic variables
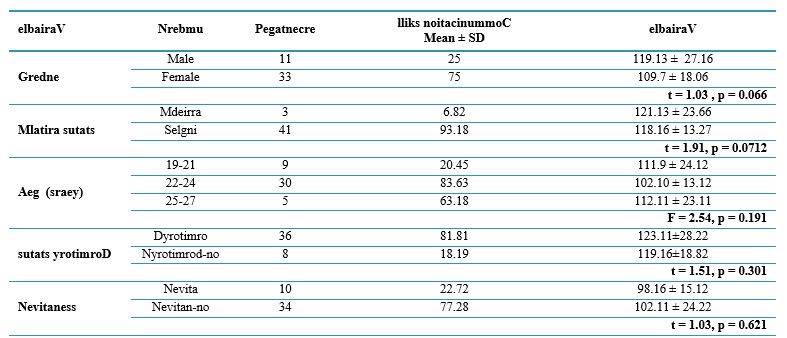
Note: ANOVA test was used to compare participants based on quantitative demographic variables of groups. t test was employed to compare participants based on qualitative variables
Abbreviations: n, number of participants; SD, standard deviation; F, analysis of variance test; Sig, statistical significance; p, probability-value.
Table 4. Comparison of mean communication skills between intervention and control groups before and after the intervention
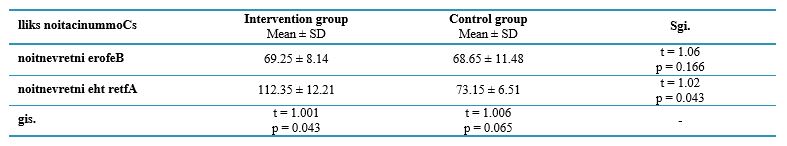
Note: Independent t-test was used to compare communication skills between groups, and paired t-test was used for within-group comparisons.
Abbreviations: SD, standard deviation; p, probability-value.
Discussion
The present study's results indicated that teaching nursing students communication skills by blending role-playing and reflection, compared to the usual method, improved their communication skills in dealing with depressed patients. Huang et al. conducted a study to determine the effect of recorded video role-playing and guided reflection on empathy, caring behavior and competence of 72 first-year nursing students of medical faculties in Taiwan. The control group received the traditional method of education. The results indicated that training based on recorded video role-playing and guided reflection improved students' empathy, caring behavior and competence [30]. The findings of this study are consistent with the results of the present study. Although the dependent variables, as well as the studied groups, are different in the current study and our study, in both studies, the blend of two methods of role-playing and reflection was able to create positive effects on the students' desired variables. In a study, Shorey et al. investigated the effectiveness of blended learning based on a communication module designed based on learning satisfaction, attitude toward communication skills, and self-efficacy of Bachelor nursing students in establishing communication. In designing the educational program of this study, in addition to using multimedia tools and virtual reality to increase students' participation in learning, role-playing and reflection exercises were used. The study's results indicated that all three variables of satisfaction with learning, attitude towards communication skills, and self-efficacy in communicating significantly differed after the study than before [31]. The results of this study were also consistent with our results. In both studies, role-playing and reflection interventions significantly increased students' communication skills. In their study, Chung et al. investigated the effectiveness of a blended training program consisting of an online module and a structured feedback system on senior nursing students' communication skills and self-efficacy in a local college in Hong Kong. The training program in the intervention group was in-person and as an online module. In the control group, only in-person training was done. The results of this study indicated the effectiveness of the blended learning approach in improving the competency of communication skills and self-efficacy of senior nursing students in clinical delivery [32]. The results of this study were also consistent with our study. Although the type of intervention in our study and this study was different, in both studies, the method of blending two educational methods was used, significantly improving nursing students' communication skills. In their study, Sadhuwong et al. explored the impact of a blended training model that combined multimedia tools with cognitive learning methods on the clinical reasoning skills of 56 junior nursing students at the Royal Thai Naval Academy. The participants engaged in this blended multimedia and cognitive approach over 10 days. In the controls, these two methods were presented without blending. The results indicated that a hybrid learning model by blending situational multimedia lessons and cognitive internship methods could enhance the clinical reasoning skills of nursing students. However, implementing the model should involve preparing learners in terms of their learning skills and self-directed thinking, as these are foundational to developing clinical reasoning skills [33]. The study's results, similar to ours, indicated that the blended approach can effectively enhance the skills of nursing students. In analyzing the results of this study with our study, both the type of blended training and the dependent variable were different in both studies. However, in the mentioned study, preparing students for communication skills was emphasized before starting the study. In their study, Hojjati et al. investigated the effectiveness of a blended clinical education model on nursing students' attitudes toward patients in the psychiatric department of Zare Hospital in Sari. Eighty-five students were included in the study, and the educational content for the intervention group and the mentioned items included film screening, group discussion, and patient education. Among cases, blended training was also given in addition to routine training. For controls, the usual clinical training such as drug therapy skills, participation in daily psychiatric visits and participation in daily rounds of the psychiatric department were implemented. The study's results indicated that blended training significantly improved students' attitudes toward homework in the mental department [34]. The results of this study are consistent with our study in terms of the effect of the blended method on nursing students in the psychological learning environment. However, the blended method used, as well as the dependent variable in the two studies, were different. In any case, regardless of the type of method, blended training can positively affect the attitude of nursing students in the psychiatric department and on homework in the psychiatric department. In a study, Shahsavari Esfahani investigated the effectiveness of the blended training method with the problem-solving method and role-playing on the satisfaction of learning the practical skill of patient education among first-year nursing students at Jahrom University. The findings indicated that students' satisfaction with the blended method increased significantly after the intervention. Also, the role-playing method increased students' emotional excitement by 85%, making them feel closer to the stage and use all their senses to observe (87%). In addition, the problem-based learning method leads to the improvement of students' skills (90%) and motivation management (92%), and the blended training method leads to high self-esteem (95%). Their practical learning increased by 89% [35]. The results of this study were consistent with that of our study in terms of the positive effects of the blended method. Although the dependent variables in this study differed from ours, the common point between these studies can be expressed as a significant increase in their practical learning. Also, the blended training method in this study was role-playing, which is the same as ours. In a study, Ilic et al. investigated the effectiveness of teaching the basics of evidence-based medicine in a blended method compared to lecture method education on competence, self-efficacy, attitude and behavior toward evidence-based medicine in medical students in their first year of clinical education. The content of the training with a blended approach, in addition to using the lecture method, included online and mobile phone-based learning, showing an educational video, communicating with the patient and providing him with the necessary training by the student. The findings showed no significant difference in the knowledge and skills of students between the two groups. However, the students' attitude in the blended training group was significantly higher [36]. Perhaps the lack of effectiveness of this method in students' knowledge and skills can be attributed to various reasons, including the first experience of students who are more focused on theoretical basis and methods such as lectures. However, this blended method significantly affected the students' attitudes. In a study, Parandavar et al. investigated the effect of designing a blended training program on the performance and clinical reasoning of midwifery students of Azad University, Jahrom Branch. The educational program implemented for the intervention group included film showing, group discussion about real scenarios, use of a simulation model and clinical decision-making exercise, and the control group received lecture-style training. According to the findings of the study, although in the intervention group, the average score of performance and clinical reasoning after the intervention was significantly higher than before, there was no statistically significant difference in the mean score of performance and clinical reasoning after the implementation of the intervention between the two groups [37]. Therefore, the results of this study contrast with those of the present study. There is a need for wider interventions for clinical reasoning. In this study, sufficient time was not allocated to provide blended training. Therefore, no significant difference was observed between the scores of the two groups after implementing the intervention. In a study, Choi et al. investigated the effectiveness of learning based on the problem-solving model compared to lecture-based teaching on critical thinking, problem-solving, and self-directed learning in first-year nursing students in Korea. Based on the study's findings, the two groups had no significant difference in critical thinking, problem-solving and self-directed learning [38]. The results of this study are inconsistent with the findings of the present research.
The small size of the sample and the lack of use of the blended approach in training based on the problem-solving model led to the absence of a significant difference between the two groups in this study. One limitation of our study was the use of a non-random sampling method, which restricts the generalizability of the findings to the broader population. Therefore, it is recommended that a study be conducted using a random sample. Another of the limitations of the present study is the individual characteristics and personality differences among students regarding their willingness to learn professional skills, which have influenced the research and are beyond the researcher's control.
Conclusion
Based on the results of the present study, it seems that blended training of role-playing and reflection is effective in improving the communication skills of nursing students in dealing with depressed patients. In light of the findings from the present study and the positive impact of the blended method compared to traditional approaches, it is recommended
that educational system managers consider incorporating this method into both theoretical and practical training courses for students.
Additionally, professors in the psychiatric nursing department should adopt this approach to enhance students' communication skills with various patients in the psychiatric unit and solicit feedback on its effectiveness from the students.
Nursing students are encouraged to share their experiences with new teaching methods, such as this blended approach, with educational administrators and faculty members. Sharing these experiences can help identify potential obstacles and weaknesses in implementing these methods. Furthermore, future studies should explore this skill across different academic programs to uncover the long-term effects of this method on students' communication skills.
Ethical considerations
The research proposal was approved by the Research Department of Birjand University of Medical Sciences under the identifier IR.BUMS.REC.1402.478. The study objectives were explained to participants, and informed consent was obtained. Participants were also assured that the data was confidential and that they could withdraw from the study at any time.
Artificial intelligence utilization for article writing
The authors confirm that generative artificial intelligence (AI) and AI-assisted technologies were not utilized in the writing process of this paper.
Acknowledgment
The authors thank the Vice Chancellor of Torbat Jam Faculty of Nursing and Midwifery and nursing students for their cooperation in this research.
Conflict of interest statement
The authors declare no conflict of interest.
Author contributions
DO designed the study, collected data, performed the statistical analysis, and drafted the manuscript. ZA conceived the initial idea for the study, assisted with the study design, and contributed to the final editing of the article. FF also collected data and conducted the statistical analysis while drafting the manuscript. HN contributed to the intervention design and helped draft the manuscript. All authors reviewed and approved the final version of the manuscript.
Funding
This research received no specific funding from public, commercial, or non-profit agencies.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Background & Objective: Communicating with depressed patients is a crucial professional skill for nursing students, which they must learn during their studies. This study aimed to assess the effectiveness of blended training—incorporating both role-playing and reflective practice—on nursing students' communication skills in their interactions with depressed patients.
Materials & Methods: The present semi-experimental study was conducted in 2023 with a before and after two-group design. All sixth-semester nursing students at Torbat Jam Faculty of Medical Sciences were randomly selected and divided into two groups: an experimental group and a control group. The intervention included therapeutic communication skill training sessions with the role-playing and reflection blended method. The control group received the standard training method. Therapeutic communication skills in dealing with depressed patients before and after the intervention were evaluated by a communication skills questionnaire. Data were analyzed using the statistical software SPSS version 20, descriptive statistical tests and inferential tests (t-test, analysis of variance, and paired-t) at a significance level 0.05.
Results: The average communication skills scores before the intervention showed no statistically significant difference between the intervention and control groups (p > 0.05). However, the mean score of communication skills after the intervention was significantly different in the two groups (p < 0.05). The results also indicated that the mean communication skill score after the intervention significantly improved in the experimental group compared to before the intervention (p < 0.05). However, there was no statistically significant change in the mean communication skill score in the control group before and after the intervention (p > 0.05).
Conclusion: Educational system managers and planners are suggested to use a blend of these two methods to train nursing students' communication skills, especially in the psychiatric department and when dealing with depressed patients.
Introduction
Effective communication is a vital element and an integral part of quality care in the nursing profession [1]. Communication is the process of transmitting messages in a planned and purposeful way to collect data, support the patient, create a collaborative space to develop a care plan and teach basic tips to improve the health level [2]. Given the unique nature of mental illnesses and the psychological symptoms experienced by these patients, establishing effective communication in the nursing care of individuals with mental health issues becomes particularly important [3]. Considering mental illnesses, using effective communication skills is a crucial tool for healthcare workers from diagnosis to treatment. In most cases, the signs and symptoms of mental illnesses can only be assessed through effective communication and the application of appropriate communication techniques and skills [4]. Communicating with a patient with mental disorders can be associated with challenges that are barely visible in other patients and needs enough skills [5]. The psychological aspects of these illnesses, along with the social stigma related to mental health diagnoses, necessitate the use of specific communication skills when informing individuals and their families about mental illnesses—particularly when they may lack sufficient understanding or literacy [6]. In other words, one of the most important dimensions of quality care in nursing is the ability to establish a proper relationship with the patient. This issue is particularly important and necessary in dealing with people with a mental health condition, such as depressed patients, who have a weaker ability to communicate than other patients [4].Depression has serious consequences for people's health, and the treatment team faces many challenges when communicating with a depressed patient. These patients provide less feedback during communication and participate less than other patients.
Following the reduction of the participation of these patients during communication, their adherence to the treatment regimen may also be affected, which threatens their health [7]. Thus, in dealing with these patients, using effective communication techniques for the treatment team members is especially important [8]. Also, effective communication between nurses and nursing students with depressed patients plays an important role in reducing stress and creating relaxation for them. The professional patient-student relationship as a source of support can affect the progress and development of an original and patient-centred therapeutic approach for better care of people with a mental health condition among students [9].
Recognizing that effective verbal and non-verbal communication skills are vital for enhancing treatment outcomes, fostering relationships with colleagues, patients, and their families, and navigating complex treatment situations for nurses and nursing students as a potential workforce for the future [10], teaching communication skills has become a key component of nursing education in recent years. Nursing students should be able to provide appropriate communication in the patient-caring process [11, 12].
Studies indicated that nursing students are unable to communicate effectively with patients, and many students are afraid of encountering patients and relatives with different backgrounds and personalities in mental health [13]. Additionally, communication skills are a vital yet often overlooked educational need for students in nursing programs. The research results emphasize that inefficient training leads to a deficit in communication skills in healthcare providers [13, 15] and holding appropriate training courses to develop the communication skills of healthcare providers is an important step toward improving these skills [14, 13].
Role-playing is one of the effective methods of teaching communication and social skills [16]. Role-playing is a form of simulation in which participants interact with a patient without the apprehension of potential risks associated with their care methods. In this method, a purposeful show is performed, and by discussing it, people can discuss their feelings, attitudes, and problem-solving strategies regarding the situation [17]. The reduction of time and cost required for training, improvement of decision-making and critical thinking skills, and increase of comprehensive self-confidence are among the advantages of this training method [16]. Despite the benefits of this method, in our country, role-playing is rarely used in medical science education, and information on the effectiveness of this method in teaching nursing students in Iran is limited [18, 19]. Another way to improve learning is reflective thinking. Reflective thinking is a thorough, ongoing, and active examination of one's beliefs and knowledge, utilizing personal justifications and inferences that help reinforce and solidify those opinions or beliefs [20]. The process of reflective thinking allows people to recall and review the experience and encourages them to search for and evaluate solutions in complex situations [16]. Reflection can lead to improving clinical reasoning skills and deep learning; thus, it is considered an important educational tool in the nursing profession [21].
In addition to improving knowledge and skills, reflection teaches learners the habit of critical thinking and learning, and therefore, it is considered an effective education method [22]. Reflective thinking helps students to improve their learning experiences during and after performing clinical skills and to realize their learning deficiencies through self-criticism [24, 23]. The numerous beneficial effects of role-playing and reflective thinking educational methods have been demonstrated individually.
Some research has considered these two educational methods complementary and concluded that combining them in teaching skills results in synergistic learning in the individual [24-26]. Despite numerous studies on each of these educational models and their effects, very little research has been conducted on the effect of blended training with role-playing and reflection methods on the communication skills of nursing students in dealing with depressed patients.
Materials & Methods
Design and setting(s)
This semi-experimental research uses a two-group design (intervention and control) with pre-test and post-test assessments. It began on July 16, 2023, and concluded on September 20, 2024.
Participants and sampling
The research population consisted of all sixth-semester nursing students at Torbat Jam Faculty of Medical Sciences, who were included in the study through a convenience non-random sampling method based on specific inclusion and exclusion criteria. The inclusion criteria included being a sixth-semester nursing student, passing the relevant theoretical and practical units so far, and not passing the internship unit in psychology. The exclusion criteria included being transfer students to the faculty and participating in communication skills training workshops. A total of 44 students participated in the study (Figure 1).
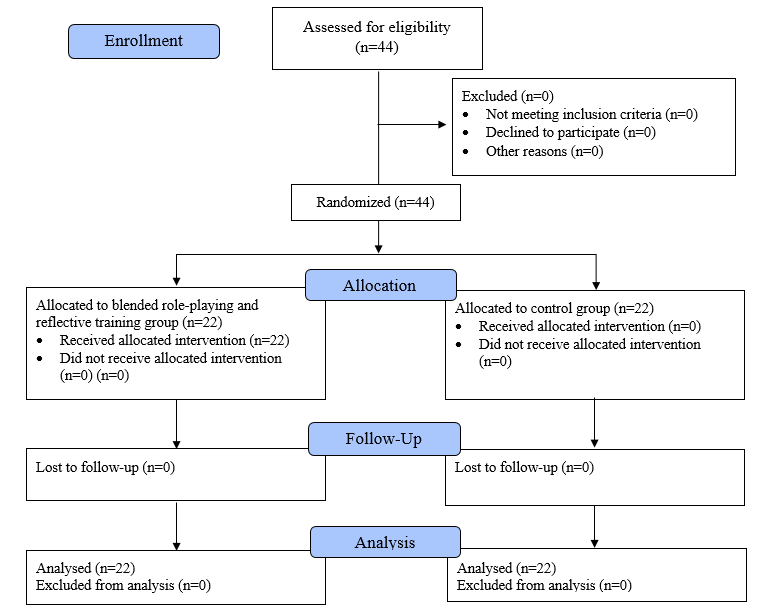
Figure 1. Flow chart of the study
Tools/Instruments
Data were collected using a demographic information questionnaire (age, gender, dormitory status, marital status, and nativeness) and a standard Interpersonal Communication Skills Scale (ASMA). This questionnaire was developed by Vakili et al. The initial questionnaire contains 43 items that fall into seven dimensions, including public communication skills, speaking skills, listening skills, interpretation and clarification skills, questioning skills, encouragement skills, and feedback skills. The options of this questionnaire are graded according to a 5-point Likert scale of 1 (very weak), 2 (weak), 3 (moderate), 4 (good) and 5 (very good). Vakili and his colleagues psychometrically evaluated this questionnaire in a study on the population of health workers in Zanjan. Based on the results of exploratory factor analysis, 30 items from this questionnaire were confirmed and placed in 7 areas of general communication skills (6 items), speaking skills (4), listening skills (4), interpretation and clarification skills (4), and questioning skills (4), encouragement and praise skill (4) and feedback skill (4). The reliability of the entire questionnaire in this study was reported using Cronbach's alpha 0.91 [27].
Data collection methods
Sixth-semester nursing students with bachelor's degrees were assigned into two experimental and control groups using a simple random method to conduct the study. Communication skills were evaluated in both experimental and control groups before the intervention by completing a questionnaire. The control group received the usual theoretical and practical method of training communication skills with depressed patients. For the intervention group, the training was implemented in combination with role-playing and reflective thinking skills of communication skills with depressed patients. After the intervention, the communication skills of both the experimental and control groups were re-evaluated using the same measurement instrument. The intervention included training in the blended method of role-playing and reflective thinking. The role-playing training method was done in the form of a theoretical explanation of the problem, and then the roles and performing the role were determined by the students and feedback was provided to them. The method consisted of seven steps: the first step involved warming up the group by introducing the problem, explaining the situation, discussing the contextual story, highlighting key issues, and outlining the role-playing activities. The second step is selecting the participants by analyzing the roles and selecting the role players. The third step is processing the scene by adjusting the principles of behaviour in the role, restating the roles and facing the problem situation. The fourth stage prepares the observers by determining the subject for the search and explaining the observation tasks. The fifth stage is discussion and evaluation, which involves reviewing role-playing behaviour (incidents, issues, realism), discussing cases, and creating the next stage. sixth stage, re-playing by playing the modified roles and suggesting the following stages with more appropriate behaviours) [28]. After teaching communication skills to the students using the role-playing method, they were asked to reflect on their experiences based on the 6-step reflection model developed by Mezirow and Taylor (2009). The steps included: 1) emotional reaction, 2) explanation and description, 3) internal review, 4) critical analysis, 5) evaluation, and 6) new action planning. Students reflected on how to communicate with patients, the relevant information regarding patient interactions, their communication skills, and the outcomes of using these skills. They documented their reflections on a sheet organized according to Mezirow and Taylor's reflection model [29]. The researcher studied the students' writings, and appropriate feedback was provided to improve their learning (Table 1). All ethical considerations were considered when conducting the study. Obtaining permission from the University of Medical Sciences and the Institute of Medical Education to participate in the study, obtaining written informed consent from the research units to participate in the study, freedom to enter and exit the study, the anonymity of the questionnaires, and the emphasis on the confidentiality of information were taken into consideration.
Table 1. Mezirow and Taylor role play steps
Data analysis
The data were analyzed using SPSS version 20 with descriptive statistics (frequency, percentage, mean, and standard deviation) and inferential tests (paired t-test, t-test, chi-square, and ANOVA).
Results
All students participated in the study, and there was no sample attrition. The Kolmogorov–Smirnov test results indicated that the study variables have a normal distribution (p > 0.05). Forty-eight percent of the participants in this study were male. The ages of the research subjects ranged from 23 to 51 years. The distribution of participants based on demographic variables is presented in Table 2. Additionally, the ANOVA and chi-square indicated no significant differences in demographic variables between the two groups (p > 0.05). The mean distribution of communication skills about demographic characteristics among the students also showed no significance (p > 0.05), as detailed in Table 3. Furthermore, there was no significant difference in the mean communication skills of students between the experimental and control groups before the intervention (p = 0.16). There was a significant difference between the cases and controls in the mean communication skills after the intervention (p = 0.04). There was a significant difference in the mean communication skills of students in the experimental group before and after the intervention (p = 0.04). In contrast, no significant difference was observed in the mean communication skills of the control group before and after the intervention (p = 0.065) (Table 4).
The data were analyzed using SPSS version 20 with descriptive statistics (frequency, percentage, mean, and standard deviation) and inferential tests (paired t-test, t-test, chi-square, and ANOVA).
Results
All students participated in the study, and there was no sample attrition. The Kolmogorov–Smirnov test results indicated that the study variables have a normal distribution (p > 0.05). Forty-eight percent of the participants in this study were male. The ages of the research subjects ranged from 23 to 51 years. The distribution of participants based on demographic variables is presented in Table 2. Additionally, the ANOVA and chi-square indicated no significant differences in demographic variables between the two groups (p > 0.05). The mean distribution of communication skills about demographic characteristics among the students also showed no significance (p > 0.05), as detailed in Table 3. Furthermore, there was no significant difference in the mean communication skills of students between the experimental and control groups before the intervention (p = 0.16). There was a significant difference between the cases and controls in the mean communication skills after the intervention (p = 0.04). There was a significant difference in the mean communication skills of students in the experimental group before and after the intervention (p = 0.04). In contrast, no significant difference was observed in the mean communication skills of the control group before and after the intervention (p = 0.065) (Table 4).
Table 2. Frequency, mean, and standard deviation of demographic characteristics of participants in the intervention and control groups
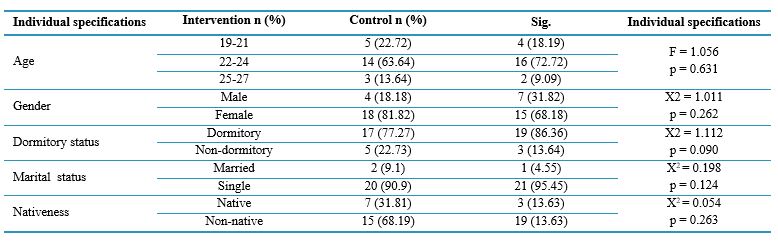
Note: ANOVA was used to compare quantitative demographic variables between groups, while the Chi-square test was used to compare qualitative variables.
Abbreviations: n, number of participants; SD, standard deviation; X2, Chi-square test; Sig., statistical significance; p, probability-value.
Table 3. Mean and standard deviation of students’ communication skills by demographic variables
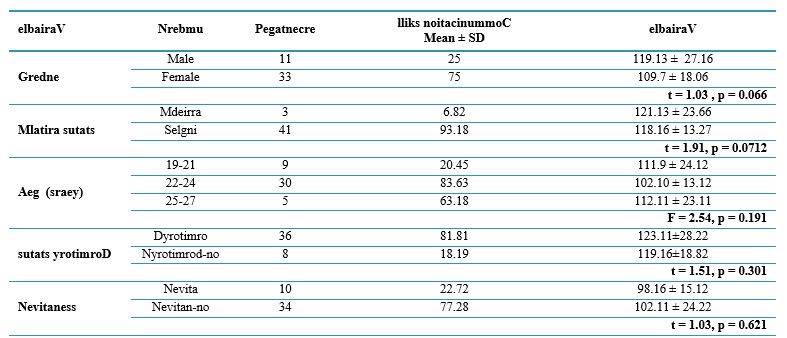
Note: ANOVA test was used to compare participants based on quantitative demographic variables of groups. t test was employed to compare participants based on qualitative variables
Abbreviations: n, number of participants; SD, standard deviation; F, analysis of variance test; Sig, statistical significance; p, probability-value.
Table 4. Comparison of mean communication skills between intervention and control groups before and after the intervention
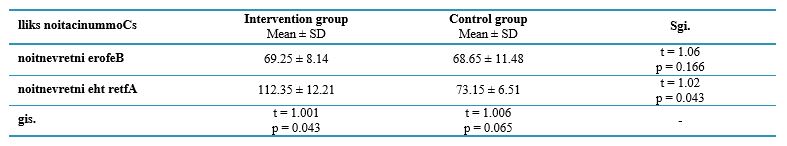
Note: Independent t-test was used to compare communication skills between groups, and paired t-test was used for within-group comparisons.
Abbreviations: SD, standard deviation; p, probability-value.
Discussion
The present study's results indicated that teaching nursing students communication skills by blending role-playing and reflection, compared to the usual method, improved their communication skills in dealing with depressed patients. Huang et al. conducted a study to determine the effect of recorded video role-playing and guided reflection on empathy, caring behavior and competence of 72 first-year nursing students of medical faculties in Taiwan. The control group received the traditional method of education. The results indicated that training based on recorded video role-playing and guided reflection improved students' empathy, caring behavior and competence [30]. The findings of this study are consistent with the results of the present study. Although the dependent variables, as well as the studied groups, are different in the current study and our study, in both studies, the blend of two methods of role-playing and reflection was able to create positive effects on the students' desired variables. In a study, Shorey et al. investigated the effectiveness of blended learning based on a communication module designed based on learning satisfaction, attitude toward communication skills, and self-efficacy of Bachelor nursing students in establishing communication. In designing the educational program of this study, in addition to using multimedia tools and virtual reality to increase students' participation in learning, role-playing and reflection exercises were used. The study's results indicated that all three variables of satisfaction with learning, attitude towards communication skills, and self-efficacy in communicating significantly differed after the study than before [31]. The results of this study were also consistent with our results. In both studies, role-playing and reflection interventions significantly increased students' communication skills. In their study, Chung et al. investigated the effectiveness of a blended training program consisting of an online module and a structured feedback system on senior nursing students' communication skills and self-efficacy in a local college in Hong Kong. The training program in the intervention group was in-person and as an online module. In the control group, only in-person training was done. The results of this study indicated the effectiveness of the blended learning approach in improving the competency of communication skills and self-efficacy of senior nursing students in clinical delivery [32]. The results of this study were also consistent with our study. Although the type of intervention in our study and this study was different, in both studies, the method of blending two educational methods was used, significantly improving nursing students' communication skills. In their study, Sadhuwong et al. explored the impact of a blended training model that combined multimedia tools with cognitive learning methods on the clinical reasoning skills of 56 junior nursing students at the Royal Thai Naval Academy. The participants engaged in this blended multimedia and cognitive approach over 10 days. In the controls, these two methods were presented without blending. The results indicated that a hybrid learning model by blending situational multimedia lessons and cognitive internship methods could enhance the clinical reasoning skills of nursing students. However, implementing the model should involve preparing learners in terms of their learning skills and self-directed thinking, as these are foundational to developing clinical reasoning skills [33]. The study's results, similar to ours, indicated that the blended approach can effectively enhance the skills of nursing students. In analyzing the results of this study with our study, both the type of blended training and the dependent variable were different in both studies. However, in the mentioned study, preparing students for communication skills was emphasized before starting the study. In their study, Hojjati et al. investigated the effectiveness of a blended clinical education model on nursing students' attitudes toward patients in the psychiatric department of Zare Hospital in Sari. Eighty-five students were included in the study, and the educational content for the intervention group and the mentioned items included film screening, group discussion, and patient education. Among cases, blended training was also given in addition to routine training. For controls, the usual clinical training such as drug therapy skills, participation in daily psychiatric visits and participation in daily rounds of the psychiatric department were implemented. The study's results indicated that blended training significantly improved students' attitudes toward homework in the mental department [34]. The results of this study are consistent with our study in terms of the effect of the blended method on nursing students in the psychological learning environment. However, the blended method used, as well as the dependent variable in the two studies, were different. In any case, regardless of the type of method, blended training can positively affect the attitude of nursing students in the psychiatric department and on homework in the psychiatric department. In a study, Shahsavari Esfahani investigated the effectiveness of the blended training method with the problem-solving method and role-playing on the satisfaction of learning the practical skill of patient education among first-year nursing students at Jahrom University. The findings indicated that students' satisfaction with the blended method increased significantly after the intervention. Also, the role-playing method increased students' emotional excitement by 85%, making them feel closer to the stage and use all their senses to observe (87%). In addition, the problem-based learning method leads to the improvement of students' skills (90%) and motivation management (92%), and the blended training method leads to high self-esteem (95%). Their practical learning increased by 89% [35]. The results of this study were consistent with that of our study in terms of the positive effects of the blended method. Although the dependent variables in this study differed from ours, the common point between these studies can be expressed as a significant increase in their practical learning. Also, the blended training method in this study was role-playing, which is the same as ours. In a study, Ilic et al. investigated the effectiveness of teaching the basics of evidence-based medicine in a blended method compared to lecture method education on competence, self-efficacy, attitude and behavior toward evidence-based medicine in medical students in their first year of clinical education. The content of the training with a blended approach, in addition to using the lecture method, included online and mobile phone-based learning, showing an educational video, communicating with the patient and providing him with the necessary training by the student. The findings showed no significant difference in the knowledge and skills of students between the two groups. However, the students' attitude in the blended training group was significantly higher [36]. Perhaps the lack of effectiveness of this method in students' knowledge and skills can be attributed to various reasons, including the first experience of students who are more focused on theoretical basis and methods such as lectures. However, this blended method significantly affected the students' attitudes. In a study, Parandavar et al. investigated the effect of designing a blended training program on the performance and clinical reasoning of midwifery students of Azad University, Jahrom Branch. The educational program implemented for the intervention group included film showing, group discussion about real scenarios, use of a simulation model and clinical decision-making exercise, and the control group received lecture-style training. According to the findings of the study, although in the intervention group, the average score of performance and clinical reasoning after the intervention was significantly higher than before, there was no statistically significant difference in the mean score of performance and clinical reasoning after the implementation of the intervention between the two groups [37]. Therefore, the results of this study contrast with those of the present study. There is a need for wider interventions for clinical reasoning. In this study, sufficient time was not allocated to provide blended training. Therefore, no significant difference was observed between the scores of the two groups after implementing the intervention. In a study, Choi et al. investigated the effectiveness of learning based on the problem-solving model compared to lecture-based teaching on critical thinking, problem-solving, and self-directed learning in first-year nursing students in Korea. Based on the study's findings, the two groups had no significant difference in critical thinking, problem-solving and self-directed learning [38]. The results of this study are inconsistent with the findings of the present research.
The small size of the sample and the lack of use of the blended approach in training based on the problem-solving model led to the absence of a significant difference between the two groups in this study. One limitation of our study was the use of a non-random sampling method, which restricts the generalizability of the findings to the broader population. Therefore, it is recommended that a study be conducted using a random sample. Another of the limitations of the present study is the individual characteristics and personality differences among students regarding their willingness to learn professional skills, which have influenced the research and are beyond the researcher's control.
Conclusion
Based on the results of the present study, it seems that blended training of role-playing and reflection is effective in improving the communication skills of nursing students in dealing with depressed patients. In light of the findings from the present study and the positive impact of the blended method compared to traditional approaches, it is recommended
that educational system managers consider incorporating this method into both theoretical and practical training courses for students.
Additionally, professors in the psychiatric nursing department should adopt this approach to enhance students' communication skills with various patients in the psychiatric unit and solicit feedback on its effectiveness from the students.
Nursing students are encouraged to share their experiences with new teaching methods, such as this blended approach, with educational administrators and faculty members. Sharing these experiences can help identify potential obstacles and weaknesses in implementing these methods. Furthermore, future studies should explore this skill across different academic programs to uncover the long-term effects of this method on students' communication skills.
Ethical considerations
The research proposal was approved by the Research Department of Birjand University of Medical Sciences under the identifier IR.BUMS.REC.1402.478. The study objectives were explained to participants, and informed consent was obtained. Participants were also assured that the data was confidential and that they could withdraw from the study at any time.
Artificial intelligence utilization for article writing
The authors confirm that generative artificial intelligence (AI) and AI-assisted technologies were not utilized in the writing process of this paper.
Acknowledgment
The authors thank the Vice Chancellor of Torbat Jam Faculty of Nursing and Midwifery and nursing students for their cooperation in this research.
Conflict of interest statement
The authors declare no conflict of interest.
Author contributions
DO designed the study, collected data, performed the statistical analysis, and drafted the manuscript. ZA conceived the initial idea for the study, assisted with the study design, and contributed to the final editing of the article. FF also collected data and conducted the statistical analysis while drafting the manuscript. HN contributed to the intervention design and helped draft the manuscript. All authors reviewed and approved the final version of the manuscript.
Funding
This research received no specific funding from public, commercial, or non-profit agencies.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2024/09/16 | Accepted: 2025/05/21 | Published: 2025/07/13
Received: 2024/09/16 | Accepted: 2025/05/21 | Published: 2025/07/13
References
1. Suikkala A, Koskinen S, Katajisto J, Leino-Kilpi H. Congruence between nursing students’ and patients’ views of student–patient relationships. Advances in Health Sciences Education. 2021;26:79-115. [DOI]
2. Gutiérrez-Puertas L, Márquez-Hernández VV, Gutiérrez-Puertas V, Granados-Gámez G, Aguilera-Manrique G. Educational interventions for nursing students to develop communication skills with patients: a systematic review. International Journal of Environmental Research and Public Health. 2020;17(7):2241 [DOI]
3. Furnes M, Kvaal KS, Høye S. Communication in mental health nursing-bachelor students' appraisal of a blended learning training programme-an exploratory study. BMC Nursing. 2018;17:1-0 [DOI]
4. Novais F, Gananca L, Barbosa M, Telles-Correia D. Communication skills in psychiatry for undergraduate students: A scoping review. Frontiers in Psychiatry. 2022;13:972703 [DOI]
5. Maulana R, Siswoyo M, Wihayati W. Therapeutic communication between psychiatrists and patients with mental health disorders (mental illness) at Waled Hospital, Cirebon Regency. Journal Socio Humanities Review. 2021;1(2):69-80.
6. Li Z, Ruan M, Chen J, Fang Y. Major depressive disorder: advances in neuroscience research and translational applications. Neuroscience Bulletin. 2021;37:863-80 [DOI]
7. Segrin C. Interpersonal communication problems associated with depression and loneliness. InHandbook of communication and emotion 1996 Jan 1 (pp. 215-242). Academic Press.
8. He P, Liu X, Wen J, Zhang Y. Major clinical advances of depression: now and future. InE3S Web of Conferences 2021 (Vol. 292, p. 03102). EDP Sciences [DOI]
9. Geisner IM, Mallett K, Varvil-Weld L, Ackerman S, Trager BM, Turrisi R. An examination of heavy drinking, depressed mood, drinking related constructs, and consequences among high-risk college students using a person-centered approach. Addictive Behaviors. 2018;78:22-9. [DOI]
10. Zaini S, Sulaiman AH, Huri HZ, Hui K, Gill JS. Patient-centred communication in the use of antidepressants among people with depression: a scoping review. Sains Malaysiana. 2021;50(1):161-70 [DOI]
11. Dewi S. Communication skills teaching and learning in undergraduate medical education: from classroom to bedside. Newcastle, NSW, Australia University of Newcastle. 2021 Mar. [Online]. Available from: [Accessed: Mar. 1, 2025]. [DOI]
12. Lee HJ, Park BM, Shin MJ, Kim DY. Therapeutic communication experiences of nurses caring for patients with hematology. InHealthcare 2022 Nov 30 (Vol. 10, No. 12, p. 2403). MDPI. [DOI]
13. Elahi N. The effect of family nursing education using reflection method with the help of situation simulation through video screening on learning and perspective of nursing students. Journal of Nursing Education. 2022;11(2):12-22. [DOI]
14. Banisi P, Khoshgoftar Z, Shahbazi S. The effect of communication skills training on the anxiety and stress of covid-19 among the university students. Iranian Journal of Rehabilitation Research in Nursing. 2023;9(2):32-40. [DOI]
15. Rosenbaum ME. Dis-integration of communication in healthcare education: workplace learning challenges and opportunities. Patient Education and Counseling. 2017;100(11):2054-61. [DOI]
16. Farahani MA, Maserat A, haghani H. Effect of role-play training on the knowledge of nursing students on patient education. Iran Journal of Nursing. 2018; 31(115):29-40. [DOI]
17. Moradi E, Didehban H. Requirements for the proper use of role-playing methods at medical universities. Medicine and Spiritual Cultivation. [Online]. Available from: [Accessed: Mar. 1, 2025]. [DOI]
18. Jasemi M, Mirzaie R, Cheragi R, Alinejad V. Journal M. The effect of role- playing therapeutic communication training in nurses on patients' anxiety before surgery: a quasi- experimental study. 2023;21(5):415-423. [DOI]
19. Latif R, Mumtaz S, Mumtaz R, Hussain A. A comparison of debate and role play in enhancing critical thinking and communication skills of medical students during problem based learning. Biochemistry and Molecular Biology Education. 2018;46(4):336-42 [DOI]
20. Engerer C, Berberat PO, Dinkel A, Rudolph B, Sattel H, Wuensch A. Specific feedback makes medical students better communicators. BMC Medical Education. 2019;19:1-8. [DOI]
21. Pangh B, Jouybari L, Vakili MA, Sanagoo A, Torik A. The effect of reflection on nurse-patient communication skills in emergency medical centers. Journal of Caring Sciences. 2019;8(2):75. [DOI]
22. Rahimi M, Haghani F. Reflection in medical education: a review of concepts, models, principles and methods of teaching reflection in medical education. Research in Medical Education. 2017;9(2):24-13. [DOI]
23. Fakouri E, Poorhakak F. Group Reflection Based on the Boud et al.'s Model.
Journal of Medical Education and Development. 2023; 18(2): 493-504 [DOI]
24. Phua GL, Owyong JL, Leong IT, et al. A systematic scoping review of group reflection in medical education. BMC Medical Education. 2024;24(1):398. [DOI]
25. Khan HS, Sheikh NS. Role-play: a simulated teaching technique in physiology. Pakistan Journal of Physiology. 2021;17(4):46-50. [Online]. Available from: [Accessed: Mar. 1, 2025]. [DOI]
26. Bharti RK. Contribution of medical education through role playing in community health promotion: a review. Iranian Journal of Public Health. 2023;52(6):1121 [DOI]
27. Vakili MM, Hidarnia AR, Niknami S. Development and psychometrics of an interpersonal communication skills scale (ASMA) among Zanjan health volunteers. Hayat. 2012;18(1):5-19. [Online]. Available from: [Accessed: Mar. 1, 2025]. [DOI]
28. Zahidova M. The role play methods in medical education. Pediatrics. 2023; 1(1): 277-280. [DOI]
29. Mezirow J, Taylor EW, editors. Transformative learning in practice: Insights from community, workplace, and higher education. John Wiley & Sons; 2009 Oct 26. [Online]. Available from: [Accessed: Mar. 1, 2025]. [DOI]
30. Huang SM, Fang SC, Lee SY, Yu PJ, Chen CJ, Lin YS. Effects of video-recorded role-play and guided reflection on nursing student empathy, caring behavior and competence: a two-group pretest-posttest study. Nurse Education in Practice. 2023;67:103560. [DOI]
31. Shorey S, Kowitlawakul Y, Devi MK, Chen HC, Soong SK, Ang E. Blended learning pedagogy designed for communication module among undergraduate nursing students: a quasi-experimental study. Nurse Education Today. 2018;61:120-6. [DOI]
32. Chung JY, Li WH, Cheung AT, Ho LL, Chung JO. Efficacy of a blended learning programme in enhancing the communication skill competence and self-efficacy of nursing students in conducting clinical handovers: a randomised controlled trial. BMC Medical Education. 2022;22(1):275 [DOI]
33. Sadhuwong K, Koraneekij P, Natakuatoong O. Effects of a blended learning model integrating situated multimedia lessons and cognitive apprenticeship method on the clinical reasoning skills of nursing students. Journal of Health Research. 2017;30(6):421-431. [DOI]
34. Hojjati H, Sharifinia H, Nazari R. The effect of blended clinical teaching on nursing students’ attitude toward psychiatric patients. Iranian Journal of Medical Education. 2011;11(3):238-44. [Online]. Available from: [Accessed: Mar. 1, 2025]. [DOI]
35. Shahsavari IS. Designing and implementing the integrated learning program in nursing education: the integration of problem-based learning and role playing methods in teaching the practical part of patient education. Teb va Tazkieh. 2017; 26(3): 219-227
36. Ilic D, Nordin RB, Glasziou P, Tilson JK, Villanueva E. A randomised controlled trial of a blended learning education intervention for teaching evidence-based medicine. BMC Medical Education. 2015;15:1-0. [DOI]
37. Parandavar N, Rezaee R, Mosallanejad L, Mosallanejad Z. Designing a blended training program and its effects on clinical practice and clinical reasoning in midwifery students. Journal of Education and Health Promotion. 2019;8(1):131 [DOI]
38. Choi E, Lindquist R, Song Y. Effects of problem-based learning vs. traditional lecture on Korean nursing students' critical thinking, problem-solving, and self-directed learning. Nurse Education Today. 2014;34(1):52-6. [DOI]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |