Tue, Feb 24, 2026
[Archive]
Volume 18, Issue 2 (2025)
J Med Edu Dev 2025, 18(2): 11-19 |
Back to browse issues page
Ethics code: IR.JUMS.REC.1401.098
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Badiyepeymaiejahromi Z, Faselehjahromi M, Rahmanian S, Hojat M. The effect of near-peer-assisted learning on self-efficacy and clinical performance of undergraduate nursing students during clinical internship: A quasi-experimental study. J Med Edu Dev 2025; 18 (2) :11-19
URL: http://edujournal.zums.ac.ir/article-1-2242-en.html
URL: http://edujournal.zums.ac.ir/article-1-2242-en.html
1- Department of Medical-Surgical Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran
2- Department of Community Health Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran
3- Department of Psychiatric Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran
4- Department of Medical-Surgical Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran ,mohsenhojat.mh@gmail.com
2- Department of Community Health Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran
3- Department of Psychiatric Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran
4- Department of Medical-Surgical Nursing, School of Nursing, Jahrom University of Medical Sciences, Jahrom, Iran ,
Keywords: clinical education, peer-assisted learning, self-efficacy, cinical performance, nursing students
Full-Text [PDF 474 kb]
(1316 Downloads)
| Abstract (HTML) (1968 Views)
Abstract
Background & Objective: Traditional clinical education methods have not been effective in improving students' clinical performance. Implementing near-peer assisted learning could help address many of the challenges nursing students encounter in their pursuit of effective learning.This study aims to determine the effect of near-peer-assisted learning on self-efficacy and clinical performance of nursing students during clinical internships.
Materials & Methods: This study utilized a quasi-experimental design with a post-test control group. The statistical population included all nursing students participating in clinical internships at Jahrom University of Medical Sciences from 2021 to 2023, totaling 93 students selected through a census method. The intervention group, comprised of 52 students, participated in near-peer assisted learning, while the control group of 41 students received traditional instruction from university instructors. Students' self-efficacy was evaluated using the standard self-efficacy in the clinical performance questionnaire; thus, clinical performance was assessed using the Objective Structured Clinical Examination (OSCE) scores at the end of each period. Data analysis was performed using SPSS 22, the t-test for mean score comparisons, and Chi-square test for qualitative data.
Results: The mean self-efficacy scores were 139.16 ± 0.57 and 109.65 ± 0.89 for the intervention and control groups in post-test, respectively. The mean OSCE scores were 5.09 ± 0.29 and 4.85 ± 0.76 for the intervention and control in post-test. The independent t-test revealed a statistically significant difference in the mean self-efficacy scores between the two groups (p < 0.001, Effect Size = 0.95). However, no significant difference was found in the mean OSCE scores between the groups (p = 0.061, Effect Size = 0.43).
Conclusion: The near-peer assisted learning method has a more significant impact on the self-efficacy of nursing students during clinical internships compared to traditional teaching methods. Furthermore, this approach can be as effective as instructor-led training in enhancing students' clinical performance. Therefore, it is recommended to integrate this method with other educational approaches to further improve clinical performance among nursing students.
Peer-assisted teaching has been used in theoretical instruction, laboratory settings, clinical skills centers, and internships [12-15]. The advantages of this method include enhancing students' time management, communication, and teaching skills. It deepens learning and promotes an active, collaborative learning style, improves test scores, and prepares students for higher-level exams. Additionally, it boosts self-confidence, reduces stress during questioning or exams, reinforces time management skills, provides continuous access to educational activities, and generally increases cost-effectiveness and efficiency [16]. In PAL, since students are more familiar with each other's educational needs and can better understand each other's learning processes compared to any instructor, they help each other more effectively during the learning process [11]. Each clinical education experience not only involves acquiring specific knowledge or practical skills but also enhances students' confidence in their professional abilities, a concept known as self-efficacy. The primary goal is to elevate students to the highest level of learning, which is professional competence. Self-efficacy affects many important aspects of motivation, such as activity choice, effort level, persistence, and emotional reactions, and can be a factor in students' academic success [17].
Given that the goal of medical education is to enhance students' clinical self-efficacy, and in light of current challenges in medical faculties—such as increased student admissions, a shortage of available instructors, and limited instructor presence in educational settings—there is an urgent need for guidance and support for students by leveraging the capabilities of senior students. Employing this method appears to be a viable solution to address some of these challenges. However, despite the benefits of PAL, existing studies present conflicting results regarding its impact on students' learning [11, 13, 23, 25] and self-efficacy [4, 17, 21], indicating a need for further research. This study aims to determine the effect of near-Peer-Assisted Learning (near-PAL) on the self-efficacy and clinical performance of nursing students during their internships at Jahrom University of Medical Sciences.
Materials & Methods
Design and setting(s)
This study was a quasi-experimental study with a post-test control group design conducted at Jahrom University of Medical Sciences.
Participants and sampling
The statistical population consisted of all nursing internship students at Jahrom University of Medical Sciences during the first semesters of the academic years 2021-2022 (52 students in the intervention group) and 2022-2023 (41 students in the control group), totaling 93 participants selected through a census method. Given the limited number of students, the census method was appropriate. The students completed clinical internship courses in adult/elderly nursing, nursing care in Intensive Care Units (ICUs), and Cardiac Care Units (CCUs). To mitigate the risk of information leakage, the study focused on two groups of first-semester students due to the small size of internship students in each year. The inclusion criteria were undergraduate nursing students enrolled in clinical internships during the academic years 2021 and 2023, informed consent to participate in the study, first-time enrollment in the internship course, and no previous education or employment in other medical sciences fields. Exclusion criteria were withdrawal from the study, academic leave, student transfer, and excessive absenteeism from the course. All students participated in the study, and none were excluded.
Tools/Instruments
The clinical performance self-efficacy questionnaire consisted of 37 questions divided into four domains: "patient assessment" (12 questions), "nursing diagnoses and planning" (9 questions), "implementation of the care plan" (10 questions), and "evaluation of the care plan" (6 questions). Responses were measured using a five-point Likert scale, ranging from "strongly disagree" to "strongly agree." Each question was scored from 1 to 5, with the total score ranging from 37 to 148, where a higher score indicated better self-efficacy. The Clinical Performance Self-Efficacy Questionnaire was developed by Cheraghi et al. This questionnaire was compiled based on a qualitative research and content analysis of individual and group interviews, as well as a review of available sources. Content validity, face validity and factor analysis of the data obtained in the research were confirmed. The concurrent validity of the "clinical performance self-efficacy" tool with the "general self-efficacy" tool was confirmed (p < 0.01, r = 0.73) along with a Cronbach's alpha coefficient of 0.96 [17].
The OSCE was designed by course instructors proficient in the OSCE methodology, involving several sessions to develop the exam blueprint, checklists, passing scores, and implementation and supervision procedures. To prepare a blueprint for the test, the various dimensions were outlined to address the learning needs and capabilities of internship students. Instructors were requested to submit their questions based on these dimensions to the group manager, aligned with the designated stations. All the scenarios were discussed and reviewed in the group of professors and the final approval was given. The exam comprised six stations, which included the following procedures: inserting a nasogastric tube, urinary catheterization, endotracheal tube suctioning, intramuscular injection, administering intravenous medication, and changing dressings. Each station was allotted five minutes, with scenarios developed by clinical internship instructors and reviewed by the faculty group. Scenarios involved performing a procedure. Evaluation checklists were derived from nursing principles and techniques textbooks, with each item scored as 0 (not performed), 0.5 (partially performed), or 1 (fully performed). The total score ranging from 0 to 6, where a higher score indicated better clinical performance. The exam was conducted in one day, and scoring was done using the checklists. One instructor related to the subject was used to evaluate the students at each station. After completing all the stations, students rested in a quarantine station, where they were supervised by a monitor to control any interactions. The OSCE exam for both groups was held with the same instructors at each station, and for blinding, instructors other than the clinical instructors of the clinical internship were used.
Data collection methods
Near-PAL was implemented for the intervention group after the research proposal was approved, the ethical code was received, and consent from the Nursing School's educational council was obtained. Students in the intervention group were informed that if they chose not to participate in the research, they could express their concerns and complete the relevant training course at another hospital. students were also reassured about the lack of effect of their decision to participate/not participate in the research on the internship grade. All students expressed their satisfaction and interest in participating in the project. Near-PAL was used for the intervention group, with senior nursing students from the Master's program in medical-surgical nursing serving as near peers. Theoretical and practical educational tasks were given to the senior nursing students with the agreement of the group manager and professors of the nursing department. The competence of the senior students in the intervention group was assessed based on their work experience in clinical departments and through observations of their clinical performance by professors during the relevant internships. The clinical competence of the selected near peers was confirmed by the Nursing School's Graduate Studies Council. Near-Peer Assisted Learning (Near-PAL) was conducted under the supervision of experienced instructors who served as resident educational supervisors at the teaching hospitals. Before starting the Near-PAL, the details of the implementation, such as tasks related to near-peers, how to evaluate and supervise, were explained in detail by the research team to the educational supervisors. Also, the senior nursing students were taught how to treat, train and supervise internship students in a 2-hour session. Internship students were randomly divided into groups of 3 people by lottery. The students participated in internship course in rotation in the medical, surgical, ICUs and CCUs of Peymaniyeh and Motahari hospitals affiliated to Jahrom University of Medical Sciences. These senior students visited the clinical wards, provided instruction and training, and conducted evaluations. The educational supervisors also monitored this process and solved it if there was a problem. The control group received traditional education from nursing school instructors. For the control group, traditional education was performed by instructors; visiting clinical wards where students were during morning and evening shifts, providing instruction and conducting evaluations. At the end of the educational course, students' clinical self-efficacy was assessed using a self-evaluation questionnaire, and their clinical performance was evaluated through an OSCE Student participation in the study is shown in Figure 1.
Data analysis
Data analysis was performed using SPSS version 22. The normality of OSCE and self-efficacy scores in the post-tests was checked using skewness and kurtosis tests. Independent t-tests were used to compare quantitative data (OSCE, self-efficacy scores, age, and GPA) and Chi-square tests were performed for performed for qualitative (marital status and sex). A significance level of 0.05 was considered.
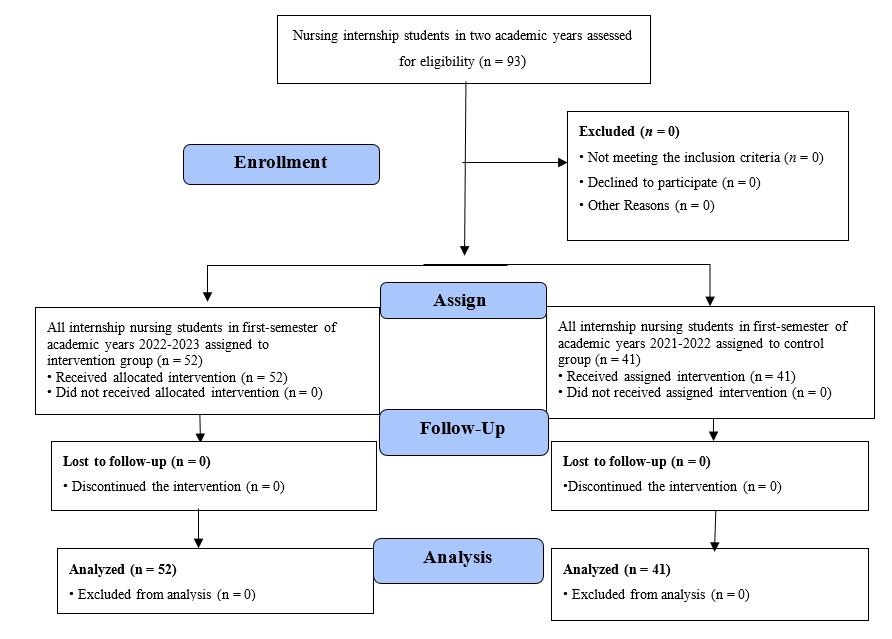
Figure1. Flow chart of the study
Results
The mean age of the students was 20.38 ± 0.029 years, and the mean grade point average was 16.64 ± 0.94. Among the participants, 76.34% were female, while 22.3% were married. There was no statistically significant difference between the two groups in terms
of demographic characteristics (Table 1). The skewness test indicated that the skewness values for the OSCE and self-efficacy scores were 0.66 and 0.71, respectively, both falling within the normal range.
Table 1. Comparison of demographic characteristics between intervention and control groups
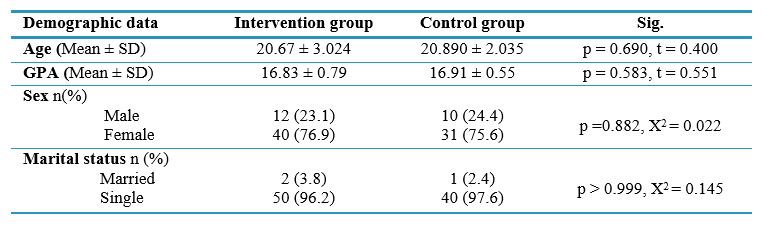
Note: Independent t-test was used to compare participants based on quantitative demographic variables of two groups. Chi-square test was used to compare qualitative demographic variables between groups.
Abbreviations: n, number of participants; SD, standard deviation; GPA, grade point average; X2, Chi-square test; t, independent t-test; Sig, statistical significance; p, probability-value.
The mean OSCE scores were 5.09 ± 0.29 and 4.85 ± 0.76 out of 6 for the intervention and control groups, respectively. Although the intervention group (PAL) had higher mean scores, the independent t-test revealed no statistically significant difference between the intervention and control groups regarding OSCE scores (p = 0.061, Effect Size = 0.43). However, the independent t-test did show a statistically significant difference between the two groups in overall self-efficacy scores (p < 0.001, Effect Size = 0.95). Additionally, the results indicated significant differences between the two groups in all dimensions of self-efficacy, including patient assessment, nursing diagnoses and planning, implementation of the care plan, and evaluation of the care plan (p < 0.05) (Table 2, Figure 2 and 3).
Table 2. Comparison of self-efficacy and OSCE mean scores between intervention and control groups after the intervention
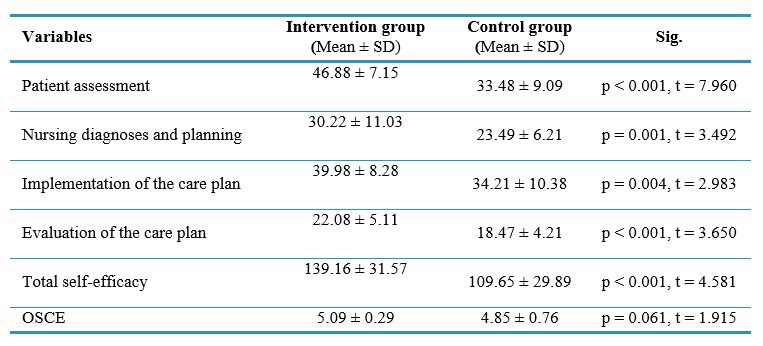
Note: An independent t-test was used to compare quantitative variables between the two groups.
Abbreviations: SD, standard deviation; t, independent t-test; Sig, statistical significance; p, probability-value.
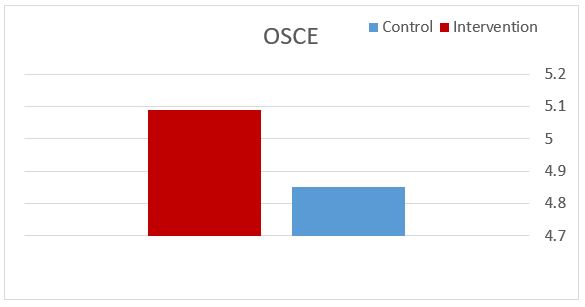
Figure 2. Comparison of the mean score of OSCE in the intervention and control groups after the intervention.
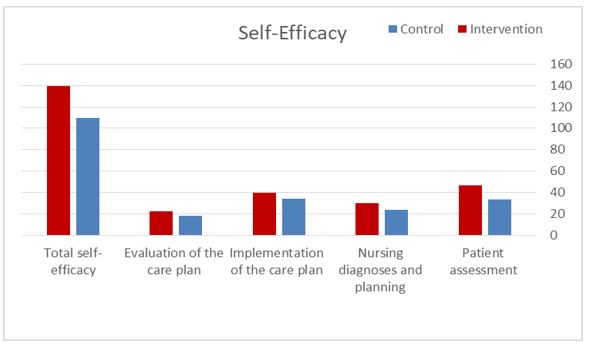
Figure 3. Comparison of the mean score of self-efficacy in the intervention and control groups after the intervention.
Discussion
This study aimed to determine the effect of near-PAL on the self-efficacy and clinical performance of nursing internship students. The results indicated a statistically significant difference in self-efficacy scores between the PAL group and the traditional instructor-led group. Due to the advantages of PAL, this method has been widely used for education and evaluation in various studies. However, there have been few studies on self-efficacy using this method, which we will discuss. The results of a study by Parchebafieh et al. showed that PAL positively affected the clinical self-efficacy of nursing students [4].
Plasson et al. conducted a quasi-experimental study in Sweden to investigate the effect of PAL on nursing students' clinical skills education. In this study, the intervention group received training through PAL for two weeks, while the control group received traditional training under the supervision of an instructor. The results also indicated that PAL was more effective in enhancing the self-efficacy of nursing students than traditional methods [18].
Studies by Austria et al. and Hellström-Hyson et al. also support the findings of the present study, identifying PAL as a factor that enhances nursing students' self-efficacy [19, 20]. According to Bandura, social support—such as that provided through peer learning—is a primary source of self-efficacy [21]. It appears that when students receive educational content from peers who are similar to them but possess slightly more knowledge, they experience less anxiety and stress. This environment provides more opportunities for practice and questions during skill acquisition, which can positively impact their self-efficacy.
In the study conducted by Brannagan et al., which aimed to investigate the effect of PAL experiences on nursing students in a clinical laboratory setting, no differences were observed between the intervention and control groups regarding improvements in self-efficacy [22]. While the differing results compared to the present study may be attributed to the differences between clinical education and laboratory education, the author also cited implementation challenges of the peer method and the insufficient preparation of peer instructors as reasons for the lack of difference between the control and intervention groups. Therefore, it should be noted that the key to successful peer education lies in having sufficient knowledge, accurate observation, providing feedback, emotional support, and collaboration among peers. Additionally, the results showed no statistically significant difference in OSCE scores between the PAL group and the traditional teaching group. This finding was consistent with Haji Hosseini's study, which demonstrated that the practical skill scores of students who used PAL were similar to those of the control group [12]. Similarly, the effect of PAL on dental students' practical skills in the clinic was investigated in Kimyai's study, and the results indicated that the practical skills of students who used PAL were comparable to those of the control group [23]. Hackman et al. found no significant difference between students' scores on written tests and the OSCE when comparing PAL to instructor-led teaching during their neurology clerkship [24]. These results suggest that this method can be as effective as clinical instructor-led teaching. Contrary to these findings, Williams's review study indicated that peer learning improved OSCE scores [25]. Goldsmith et al. conducted a study to determine the effect of peer teaching on the practical skills of third-year nursing students at the University of Sydney. Their results showed significant improvement in practical skills in the PAL group of third-year nursing students [26]. Other studies comparing the effect of peer and non-peer learning methods on students' clinical skills have also shown that peer learning is effective [13, 16, 27]. Differences in study design, peer groups, intervention implementation, academic disciplines, academic years of the peers, and the complexity of the educational content relative to the peers' abilities may explain the varied results across studies. PAL can be successfully integrated into educational curricula, with feedback highlighting significant benefits of this teaching method [11]. However, fully replacing formal academic instructors with near peers would be premature. Therefore, it is crucial to provide appropriate training for peer educators, monitor the quality of education they deliver, and utilize near peers as a complement to academic instructors [28]. Additionally, this method may help address the shortage of instructors at universities, increase student satisfaction, and reduce the time and cost of education [11]. Nonetheless, it is crucial to consider that students generally perceive formal instructors as having better knowledge, explanatory skills, and communication abilities. Furthermore, in most studies, the results have been attributed to the intervention without much consideration of potential influences from participants' development or other environmental and educational factors. Given these limitations, it is essential to cautiously attribute outcomes to the intervention. In addition among the limitations of this research are its single-center design, small sample size, lack of a pre-test, and the unexamined long-term effects of the intervention on students. Additionally, this study did not account for potential confounding variables, such as student motivation or external support systems, which could influence self-efficacy and clinical performance.
The findings of this research can be applied in educational settings by incorporating this teaching method, in clinical practice to enhance the quality of care provided by students and nurses, and in management for planning clinical internships and practicum courses using this educational approach.
Conclusion
The near-PAL method has a more significant impact on the self-efficacy of nursing students during clinical internships compared to traditional teaching methods. Furthermore, it can be equally effective as instructor-led teaching in enhancing students' clinical performance. Therefore, it is recommended to use this approach in conjunction with other teaching methods that can further improve clinical performance among students. Given the limited number of studies in this area, future research is suggested to explore the use of near-PAL across various nursing specialties, with a focus on incorporating randomization. Additionally, investigating the long-term effects of near-PAL on clinical performance and self-efficacy in nursing students is essential. Further research combining both quantitative and qualitative methods is needed to enhance data reliability and to understand other aspects of implementing this student-centered educational approach. Adopting the PAL method as a student-centered educational strategy could better prepare students to take on educational roles in clinical settings.
Ethical considerations
This research was conducted with the ethical code IR.JUMS.REC.1401.098. Ethical principles, such as obtaining informed consent, voluntary participation, explaining the research objectives, and ensuring the confidentiality of participants' information, were observed.
Artificial intelligence utilization for article writing
The authors declare that no AI-based tools were used in conducting the research or preparing this manuscript.
Acknowledgment
We are grateful to all the students and instructors who assisted us in conducting this study, as well as the Research Deputy of Jahrom University of Medical Sciences for supporting this research project.
Conflict of interest statement
The authors declare no potential conflicts of interest.
Author contributions
Z.B and M.H conceptualized the study. Z.B and S.R drafted the manuscript, while M.H and M.F provided revisions and critical feedback. All authors approved the final version of the manuscript for publication.
Funding
This study was financially supported by the Research Deputy of Jahrom University of Medical Sciences.
Data availability statement
The datasets used and analyzed in this study are available from the corresponding author upon reasonable request.
Full-Text: (218 Views)
Abstract
Background & Objective: Traditional clinical education methods have not been effective in improving students' clinical performance. Implementing near-peer assisted learning could help address many of the challenges nursing students encounter in their pursuit of effective learning.This study aims to determine the effect of near-peer-assisted learning on self-efficacy and clinical performance of nursing students during clinical internships.
Materials & Methods: This study utilized a quasi-experimental design with a post-test control group. The statistical population included all nursing students participating in clinical internships at Jahrom University of Medical Sciences from 2021 to 2023, totaling 93 students selected through a census method. The intervention group, comprised of 52 students, participated in near-peer assisted learning, while the control group of 41 students received traditional instruction from university instructors. Students' self-efficacy was evaluated using the standard self-efficacy in the clinical performance questionnaire; thus, clinical performance was assessed using the Objective Structured Clinical Examination (OSCE) scores at the end of each period. Data analysis was performed using SPSS 22, the t-test for mean score comparisons, and Chi-square test for qualitative data.
Results: The mean self-efficacy scores were 139.16 ± 0.57 and 109.65 ± 0.89 for the intervention and control groups in post-test, respectively. The mean OSCE scores were 5.09 ± 0.29 and 4.85 ± 0.76 for the intervention and control in post-test. The independent t-test revealed a statistically significant difference in the mean self-efficacy scores between the two groups (p < 0.001, Effect Size = 0.95). However, no significant difference was found in the mean OSCE scores between the groups (p = 0.061, Effect Size = 0.43).
Conclusion: The near-peer assisted learning method has a more significant impact on the self-efficacy of nursing students during clinical internships compared to traditional teaching methods. Furthermore, this approach can be as effective as instructor-led training in enhancing students' clinical performance. Therefore, it is recommended to integrate this method with other educational approaches to further improve clinical performance among nursing students.
Introduction
Nursing education serves as the foundation for developing a skilled workforce capable of meeting public health needs; therefore, any shortcomings in this education can significantly impact the quality of patient care [1]. A substantial portion of nursing students' training occurs in clinical settings. The primary goal of this clinical education is to prepare students for their essential professional responsibilities, enhance their accountability, and foster their ability to work independently [2, 3]. Self-efficacy in clinical performance plays a crucial role in a student's ability to provide independent patient care. For nursing students, self-efficacy encompasses their confidence in executing routine nursing tasks, while clinical performance self-efficacy specifically refers to their belief in their capability to perform various clinical skills. The importance of self-efficacy in clinical settings is linked to its impact on future performance [4]. Despite the importance of the subject, studies indicate that nursing students trained through traditional clinical education methods often lack the necessary practical skills and efficiency in real work environments, leading to challenges in performing their job duties. In this model, students engage with instructors in small groups during an 8-hour clinical shift [5]. Effective learning requires the support and collaboration of instructors, mentors, peers, and other resources, each providing unique opportunities to address students' learning needs. Given that teaching is an activity focused on creating and facilitating learning for students, it is evident that selecting effective teaching methods plays a critical role in enhancing the learning process [6, 7]. There are various types of modern training of nursing skills using educational models; such as exploratory education model, bedside teaching and need-based education, problem-solving-based education, cooperative education and peer-assisted learning [8]. Numerous studies have been conducted to improve the quality of education, and some have identified Peer-Assisted Learning (PAL) as an effective strategy for addressing challenges and enhancing learning outcomes [9]. PAL is rooted in social learning theories, which assert that experiences, understanding, and knowledge are developed through interactions among individuals [10]. PAL follows the constructivist learning approach and is one of the teaching-learning methods used in various academic programs and age groups [9]. This method includes two models: using near peers or partner peers in education. Near peers are students who are always at a higher level, academically or in clinical experience, by at least one year compared to the students they are teaching. The distinction between near-peer-assisted learning and partner peer-assisted learning lies in the fact that partner peers are at the same academic level as the student [11].Peer-assisted teaching has been used in theoretical instruction, laboratory settings, clinical skills centers, and internships [12-15]. The advantages of this method include enhancing students' time management, communication, and teaching skills. It deepens learning and promotes an active, collaborative learning style, improves test scores, and prepares students for higher-level exams. Additionally, it boosts self-confidence, reduces stress during questioning or exams, reinforces time management skills, provides continuous access to educational activities, and generally increases cost-effectiveness and efficiency [16]. In PAL, since students are more familiar with each other's educational needs and can better understand each other's learning processes compared to any instructor, they help each other more effectively during the learning process [11]. Each clinical education experience not only involves acquiring specific knowledge or practical skills but also enhances students' confidence in their professional abilities, a concept known as self-efficacy. The primary goal is to elevate students to the highest level of learning, which is professional competence. Self-efficacy affects many important aspects of motivation, such as activity choice, effort level, persistence, and emotional reactions, and can be a factor in students' academic success [17].
Given that the goal of medical education is to enhance students' clinical self-efficacy, and in light of current challenges in medical faculties—such as increased student admissions, a shortage of available instructors, and limited instructor presence in educational settings—there is an urgent need for guidance and support for students by leveraging the capabilities of senior students. Employing this method appears to be a viable solution to address some of these challenges. However, despite the benefits of PAL, existing studies present conflicting results regarding its impact on students' learning [11, 13, 23, 25] and self-efficacy [4, 17, 21], indicating a need for further research. This study aims to determine the effect of near-Peer-Assisted Learning (near-PAL) on the self-efficacy and clinical performance of nursing students during their internships at Jahrom University of Medical Sciences.
Materials & Methods
Design and setting(s)
This study was a quasi-experimental study with a post-test control group design conducted at Jahrom University of Medical Sciences.
Participants and sampling
The statistical population consisted of all nursing internship students at Jahrom University of Medical Sciences during the first semesters of the academic years 2021-2022 (52 students in the intervention group) and 2022-2023 (41 students in the control group), totaling 93 participants selected through a census method. Given the limited number of students, the census method was appropriate. The students completed clinical internship courses in adult/elderly nursing, nursing care in Intensive Care Units (ICUs), and Cardiac Care Units (CCUs). To mitigate the risk of information leakage, the study focused on two groups of first-semester students due to the small size of internship students in each year. The inclusion criteria were undergraduate nursing students enrolled in clinical internships during the academic years 2021 and 2023, informed consent to participate in the study, first-time enrollment in the internship course, and no previous education or employment in other medical sciences fields. Exclusion criteria were withdrawal from the study, academic leave, student transfer, and excessive absenteeism from the course. All students participated in the study, and none were excluded.
Tools/Instruments
The clinical performance self-efficacy questionnaire consisted of 37 questions divided into four domains: "patient assessment" (12 questions), "nursing diagnoses and planning" (9 questions), "implementation of the care plan" (10 questions), and "evaluation of the care plan" (6 questions). Responses were measured using a five-point Likert scale, ranging from "strongly disagree" to "strongly agree." Each question was scored from 1 to 5, with the total score ranging from 37 to 148, where a higher score indicated better self-efficacy. The Clinical Performance Self-Efficacy Questionnaire was developed by Cheraghi et al. This questionnaire was compiled based on a qualitative research and content analysis of individual and group interviews, as well as a review of available sources. Content validity, face validity and factor analysis of the data obtained in the research were confirmed. The concurrent validity of the "clinical performance self-efficacy" tool with the "general self-efficacy" tool was confirmed (p < 0.01, r = 0.73) along with a Cronbach's alpha coefficient of 0.96 [17].
The OSCE was designed by course instructors proficient in the OSCE methodology, involving several sessions to develop the exam blueprint, checklists, passing scores, and implementation and supervision procedures. To prepare a blueprint for the test, the various dimensions were outlined to address the learning needs and capabilities of internship students. Instructors were requested to submit their questions based on these dimensions to the group manager, aligned with the designated stations. All the scenarios were discussed and reviewed in the group of professors and the final approval was given. The exam comprised six stations, which included the following procedures: inserting a nasogastric tube, urinary catheterization, endotracheal tube suctioning, intramuscular injection, administering intravenous medication, and changing dressings. Each station was allotted five minutes, with scenarios developed by clinical internship instructors and reviewed by the faculty group. Scenarios involved performing a procedure. Evaluation checklists were derived from nursing principles and techniques textbooks, with each item scored as 0 (not performed), 0.5 (partially performed), or 1 (fully performed). The total score ranging from 0 to 6, where a higher score indicated better clinical performance. The exam was conducted in one day, and scoring was done using the checklists. One instructor related to the subject was used to evaluate the students at each station. After completing all the stations, students rested in a quarantine station, where they were supervised by a monitor to control any interactions. The OSCE exam for both groups was held with the same instructors at each station, and for blinding, instructors other than the clinical instructors of the clinical internship were used.
Data collection methods
Near-PAL was implemented for the intervention group after the research proposal was approved, the ethical code was received, and consent from the Nursing School's educational council was obtained. Students in the intervention group were informed that if they chose not to participate in the research, they could express their concerns and complete the relevant training course at another hospital. students were also reassured about the lack of effect of their decision to participate/not participate in the research on the internship grade. All students expressed their satisfaction and interest in participating in the project. Near-PAL was used for the intervention group, with senior nursing students from the Master's program in medical-surgical nursing serving as near peers. Theoretical and practical educational tasks were given to the senior nursing students with the agreement of the group manager and professors of the nursing department. The competence of the senior students in the intervention group was assessed based on their work experience in clinical departments and through observations of their clinical performance by professors during the relevant internships. The clinical competence of the selected near peers was confirmed by the Nursing School's Graduate Studies Council. Near-Peer Assisted Learning (Near-PAL) was conducted under the supervision of experienced instructors who served as resident educational supervisors at the teaching hospitals. Before starting the Near-PAL, the details of the implementation, such as tasks related to near-peers, how to evaluate and supervise, were explained in detail by the research team to the educational supervisors. Also, the senior nursing students were taught how to treat, train and supervise internship students in a 2-hour session. Internship students were randomly divided into groups of 3 people by lottery. The students participated in internship course in rotation in the medical, surgical, ICUs and CCUs of Peymaniyeh and Motahari hospitals affiliated to Jahrom University of Medical Sciences. These senior students visited the clinical wards, provided instruction and training, and conducted evaluations. The educational supervisors also monitored this process and solved it if there was a problem. The control group received traditional education from nursing school instructors. For the control group, traditional education was performed by instructors; visiting clinical wards where students were during morning and evening shifts, providing instruction and conducting evaluations. At the end of the educational course, students' clinical self-efficacy was assessed using a self-evaluation questionnaire, and their clinical performance was evaluated through an OSCE Student participation in the study is shown in Figure 1.
Data analysis
Data analysis was performed using SPSS version 22. The normality of OSCE and self-efficacy scores in the post-tests was checked using skewness and kurtosis tests. Independent t-tests were used to compare quantitative data (OSCE, self-efficacy scores, age, and GPA) and Chi-square tests were performed for performed for qualitative (marital status and sex). A significance level of 0.05 was considered.
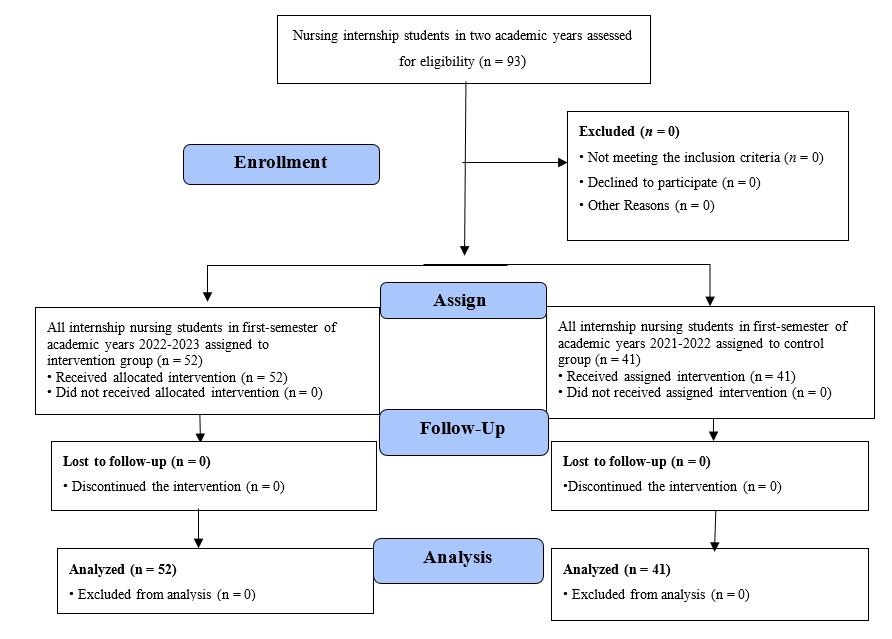
Figure1. Flow chart of the study
Results
The mean age of the students was 20.38 ± 0.029 years, and the mean grade point average was 16.64 ± 0.94. Among the participants, 76.34% were female, while 22.3% were married. There was no statistically significant difference between the two groups in terms
of demographic characteristics (Table 1). The skewness test indicated that the skewness values for the OSCE and self-efficacy scores were 0.66 and 0.71, respectively, both falling within the normal range.
Table 1. Comparison of demographic characteristics between intervention and control groups
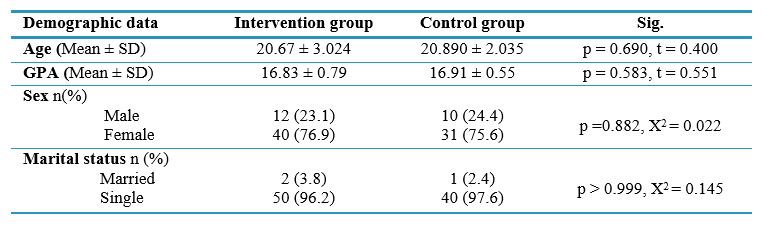
Note: Independent t-test was used to compare participants based on quantitative demographic variables of two groups. Chi-square test was used to compare qualitative demographic variables between groups.
Abbreviations: n, number of participants; SD, standard deviation; GPA, grade point average; X2, Chi-square test; t, independent t-test; Sig, statistical significance; p, probability-value.
The mean OSCE scores were 5.09 ± 0.29 and 4.85 ± 0.76 out of 6 for the intervention and control groups, respectively. Although the intervention group (PAL) had higher mean scores, the independent t-test revealed no statistically significant difference between the intervention and control groups regarding OSCE scores (p = 0.061, Effect Size = 0.43). However, the independent t-test did show a statistically significant difference between the two groups in overall self-efficacy scores (p < 0.001, Effect Size = 0.95). Additionally, the results indicated significant differences between the two groups in all dimensions of self-efficacy, including patient assessment, nursing diagnoses and planning, implementation of the care plan, and evaluation of the care plan (p < 0.05) (Table 2, Figure 2 and 3).
Table 2. Comparison of self-efficacy and OSCE mean scores between intervention and control groups after the intervention
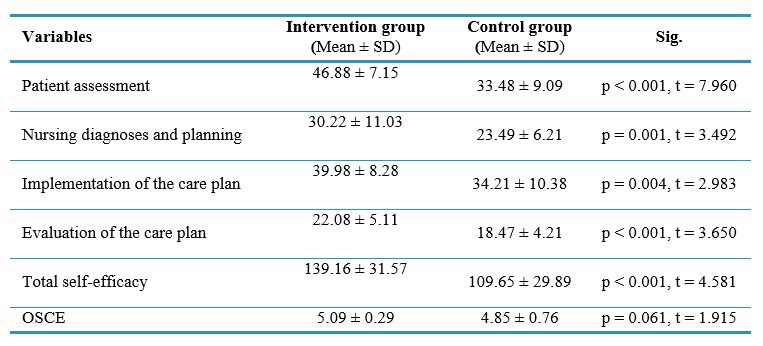
Note: An independent t-test was used to compare quantitative variables between the two groups.
Abbreviations: SD, standard deviation; t, independent t-test; Sig, statistical significance; p, probability-value.
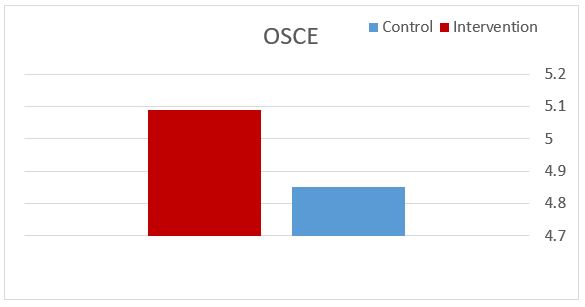
Figure 2. Comparison of the mean score of OSCE in the intervention and control groups after the intervention.
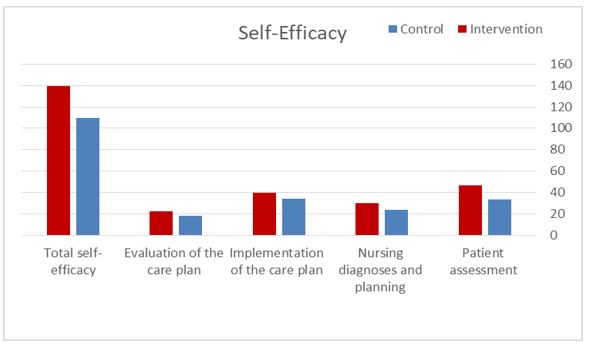
Figure 3. Comparison of the mean score of self-efficacy in the intervention and control groups after the intervention.
Discussion
This study aimed to determine the effect of near-PAL on the self-efficacy and clinical performance of nursing internship students. The results indicated a statistically significant difference in self-efficacy scores between the PAL group and the traditional instructor-led group. Due to the advantages of PAL, this method has been widely used for education and evaluation in various studies. However, there have been few studies on self-efficacy using this method, which we will discuss. The results of a study by Parchebafieh et al. showed that PAL positively affected the clinical self-efficacy of nursing students [4].
Plasson et al. conducted a quasi-experimental study in Sweden to investigate the effect of PAL on nursing students' clinical skills education. In this study, the intervention group received training through PAL for two weeks, while the control group received traditional training under the supervision of an instructor. The results also indicated that PAL was more effective in enhancing the self-efficacy of nursing students than traditional methods [18].
Studies by Austria et al. and Hellström-Hyson et al. also support the findings of the present study, identifying PAL as a factor that enhances nursing students' self-efficacy [19, 20]. According to Bandura, social support—such as that provided through peer learning—is a primary source of self-efficacy [21]. It appears that when students receive educational content from peers who are similar to them but possess slightly more knowledge, they experience less anxiety and stress. This environment provides more opportunities for practice and questions during skill acquisition, which can positively impact their self-efficacy.
In the study conducted by Brannagan et al., which aimed to investigate the effect of PAL experiences on nursing students in a clinical laboratory setting, no differences were observed between the intervention and control groups regarding improvements in self-efficacy [22]. While the differing results compared to the present study may be attributed to the differences between clinical education and laboratory education, the author also cited implementation challenges of the peer method and the insufficient preparation of peer instructors as reasons for the lack of difference between the control and intervention groups. Therefore, it should be noted that the key to successful peer education lies in having sufficient knowledge, accurate observation, providing feedback, emotional support, and collaboration among peers. Additionally, the results showed no statistically significant difference in OSCE scores between the PAL group and the traditional teaching group. This finding was consistent with Haji Hosseini's study, which demonstrated that the practical skill scores of students who used PAL were similar to those of the control group [12]. Similarly, the effect of PAL on dental students' practical skills in the clinic was investigated in Kimyai's study, and the results indicated that the practical skills of students who used PAL were comparable to those of the control group [23]. Hackman et al. found no significant difference between students' scores on written tests and the OSCE when comparing PAL to instructor-led teaching during their neurology clerkship [24]. These results suggest that this method can be as effective as clinical instructor-led teaching. Contrary to these findings, Williams's review study indicated that peer learning improved OSCE scores [25]. Goldsmith et al. conducted a study to determine the effect of peer teaching on the practical skills of third-year nursing students at the University of Sydney. Their results showed significant improvement in practical skills in the PAL group of third-year nursing students [26]. Other studies comparing the effect of peer and non-peer learning methods on students' clinical skills have also shown that peer learning is effective [13, 16, 27]. Differences in study design, peer groups, intervention implementation, academic disciplines, academic years of the peers, and the complexity of the educational content relative to the peers' abilities may explain the varied results across studies. PAL can be successfully integrated into educational curricula, with feedback highlighting significant benefits of this teaching method [11]. However, fully replacing formal academic instructors with near peers would be premature. Therefore, it is crucial to provide appropriate training for peer educators, monitor the quality of education they deliver, and utilize near peers as a complement to academic instructors [28]. Additionally, this method may help address the shortage of instructors at universities, increase student satisfaction, and reduce the time and cost of education [11]. Nonetheless, it is crucial to consider that students generally perceive formal instructors as having better knowledge, explanatory skills, and communication abilities. Furthermore, in most studies, the results have been attributed to the intervention without much consideration of potential influences from participants' development or other environmental and educational factors. Given these limitations, it is essential to cautiously attribute outcomes to the intervention. In addition among the limitations of this research are its single-center design, small sample size, lack of a pre-test, and the unexamined long-term effects of the intervention on students. Additionally, this study did not account for potential confounding variables, such as student motivation or external support systems, which could influence self-efficacy and clinical performance.
The findings of this research can be applied in educational settings by incorporating this teaching method, in clinical practice to enhance the quality of care provided by students and nurses, and in management for planning clinical internships and practicum courses using this educational approach.
Conclusion
The near-PAL method has a more significant impact on the self-efficacy of nursing students during clinical internships compared to traditional teaching methods. Furthermore, it can be equally effective as instructor-led teaching in enhancing students' clinical performance. Therefore, it is recommended to use this approach in conjunction with other teaching methods that can further improve clinical performance among students. Given the limited number of studies in this area, future research is suggested to explore the use of near-PAL across various nursing specialties, with a focus on incorporating randomization. Additionally, investigating the long-term effects of near-PAL on clinical performance and self-efficacy in nursing students is essential. Further research combining both quantitative and qualitative methods is needed to enhance data reliability and to understand other aspects of implementing this student-centered educational approach. Adopting the PAL method as a student-centered educational strategy could better prepare students to take on educational roles in clinical settings.
Ethical considerations
This research was conducted with the ethical code IR.JUMS.REC.1401.098. Ethical principles, such as obtaining informed consent, voluntary participation, explaining the research objectives, and ensuring the confidentiality of participants' information, were observed.
Artificial intelligence utilization for article writing
The authors declare that no AI-based tools were used in conducting the research or preparing this manuscript.
Acknowledgment
We are grateful to all the students and instructors who assisted us in conducting this study, as well as the Research Deputy of Jahrom University of Medical Sciences for supporting this research project.
Conflict of interest statement
The authors declare no potential conflicts of interest.
Author contributions
Z.B and M.H conceptualized the study. Z.B and S.R drafted the manuscript, while M.H and M.F provided revisions and critical feedback. All authors approved the final version of the manuscript for publication.
Funding
This study was financially supported by the Research Deputy of Jahrom University of Medical Sciences.
Data availability statement
The datasets used and analyzed in this study are available from the corresponding author upon reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2024/08/4 | Accepted: 2025/04/23 | Published: 2025/07/13
Received: 2024/08/4 | Accepted: 2025/04/23 | Published: 2025/07/13
References
1. Rahimi Z, Badiyepeymaiejahromi Z, Taghizadeganzadeh M. 360-degree evaluation of nursing students' performance. Shiraz E-Medical Journal. 2024;25(11):e148872. [DOI]
2. Chang CY, Gau ML, Tang KY, Hwang GJ. Directions of the 100 most cited nursing student education research: a bibliometric and co-citation network analysis. Nurse Education Today. 2021;96:104645 [DOI]
3. Montaseri MA, Javadpour S, Ramezanli S, Badiyepeymaiejahromi Z. The effect of blended education on nursing students' learning and educational climate in pharmacology internship. Journal of Medical Education Development. 2023;10;15(48):52-61. [DOI]
4. Parchebafieh S, Safavi M, Mashouf S, Salehi S, Esmaeilpour Zanjani S, Bakhshandeh H. Effect of using Peer Assisted Learning approach on clinical self-efficacy of nursing students in Islamic Azad University of Tehran Medical Sciences branch. Journal of Nursing Education. 2018;6(6):8-15.[Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
5. Ghafari S, Atashi V, Taleghani F, Irajpour A, Sabohi F, Yazdannik A. Comparison the effect of two methods of internship and apprenticeship in the field on clinical competence of nursing students. Research in Medical Education. 2022;14(1):64-72. [DOI]
6. Jang A, Song C. Internet of things platform technology used in undergraduate nursing student education: a scoping review protocol. BMJ Open. 2022;12(4):e058556 [DOI]
7. academic nursing education. Iranian Journal of Medical Education. 2014;14(4):323-31. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
8. Afaghi E, Rezaei M, Beheshtifar M, Kalroozi F. The effect of peer education on nursing students’ clinical dressing skills and perceived stress scores at Aja University of Medical Sciences. Military Caring Sciences. 2023;10(3):229-37. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
9. Omidkhoda A, Dehdarirad H, Changizi V. Planning, implementation and evaluation of active learning- teaching methods in inverted classroom,peer learning and virtual education among students in the school of allied medical sciences. Research in Medical Education. 2021;13(3):42-54 [DOI]
10. Secomb J. A systematic review of peer teaching and learning in clinical education. Journal of Clinical Nursing. 2008;17(6):703-16. [DOI]
11. Jauregui J, Bright S, Strote J, Shandro J. A novel approach to medical student peer-assisted learning through case-based simulations. The Western Journal of Emergency Medicine. 2018;19(1):193-197. [DOI]
12. 12. Hajihosseini F, Izadi A, Mahboobi M, Mohammadtabar R. Effect of peer education on practical skills learning of nursing students in clinical skill lab of Mazandaran university of medical sciences. Medical Education Journal. 2013;1(1):13-17. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
13. 13. Kayzouri A, Yaghoutimoghaddam H, Sadeghi H, Hoseinzadeh Hesari M, Haghnazar M. The evaluation effect of peer and non-peer education methods on clinical learning of anesthesia students in Sabzevar university of medical sciences 2016-2017. Journal of Sabzevar University of Medical Sciences. 2019;26(4):487-93. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
14. Safari M, Yazdanpah B, Mahmoudi F, Yaghobean N. Comparing students’ rate of learning through lecturing and peer group teaching and study their viewpoints. Research in Medical Education. 2018;10(3):24-34. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
15. Eslami Akbar R, Hojat M, Badiyepeymaie Jahromi Z. Comparison of teaching through peer learning with the lecture method on the learning level of anesthesiology students at Jahrom university of medical sciences in 2013. Journal of Nursing Education. 2015;4(3):56-65. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
16. Moaddab F, Ghanbari A, Paryad E, Jahani M, Sedighi A. The effect of using the peer assisted learning system from the perspective of nursing students: a quasi-experimental study. Horizon of Medical Education Development. 2020;11(1):26-42. [DOI]
17. Cheraghi F, Hassani P, Yaghmaei F, Alavi Majd H. Development and psychometric performance of clinical efficacy. Payesh. 2009;9(1):51-60. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
18. Palsson Y, Martensson G, Swenne CL, Adel E, Engstrom M. A peer learning intervention for nursing students in clinical practice education: A quasi-experimental study. Nurse Education Today. 2017;51:81-7. [DOI]
19. Austria MJ, Baraki K, Doig AK. Collaborative learning using nursing student dyads in the clinical setting. International Journal of Nursing Education Scholarship. 2013;10(1):73-80. [DOI]
20. Hellström-Hyson E, Mårtensson G, Kristofferzon ML. To take responsibility or to be an onlooker. Nursing students' experiences of two models of supervision. Nurse Education Today. 2012;32(1):105-10. [DOI]
21. Bandura A. Self-efficacy: The exercise of control. Freeman; 1997. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
22. Brannagan KB, Dellinger A, Thomas J, Mitchell D, Lewis-Trabeaux S, Dupre S. Impact of peer teaching on nursing students: perceptions of learning environment, self-efficacy, and knowledge. Nurse Eduction Today. 2013;33(11):1440–1447. [DOI]
23. Kimyai S, Jafari Navimipour E, Mohammadi N. The effect of peer education on practical skills training of dentistry students in restorative preclinic. Iranian Journal of Medical Education. 2011;11(4):418-424. [Online]. Available from: [Accessed: August. 4, 2024]. [PubMed]
24. Heckmann JG, Dütsch M, Rauch C, Lang C, Weih M, Schwab S. Effects of peer-assisted training during the neurology clerkship: a randomized controlled study. Eurpean Journal of Neurolgy. 2008;15(12):1365-70. [DOI]
25. Williams B, Reddy P. Does peer-assisted learning improve academic performance? A scoping review. Nurse Education Today. 2016;42:23-9. [DOI]
26. Goldsmith M, Stewart L, Ferguson L. Peer learning partnership: an innovative strategy to enhance skill acquisition in nursing students. Nurse Education Today. 2006;26(2):123-30 [DOI]
27. Salehi S, Safavi M, Mashoof S, Parchebafieh S, Fesharaki M. Effects of peer education on clinical skills in nursing students, including interns and trainees. Medical Science Journal of Islamic Azad Univesity-Tehran Medical Branch. 2016; 26(1): 36-45. [Online]. Available from: [Accessed: August. 4, 2024]. [DOI]
28. Jackson TA, Evans DJ. Can medical students teach? A near-peer-led teaching program for year 1students. Advance in Physiology Education. 2012;36(3):192-6. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |