Tue, Feb 17, 2026
[Archive]
Volume 17, Issue 54 (2024)
J Med Edu Dev 2024, 17(54): 21-30 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sohrabi Z, Ramezanpour E, Rashidi N, Nouri Khaneghah Z, Nosrati S, Barry A et al . Improving scrub and circulating skills in operating room students: A quasi-experimental study on the influence of reflective education. J Med Edu Dev 2024; 17 (54) :21-30
URL: http://edujournal.zums.ac.ir/article-1-1951-en.html
URL: http://edujournal.zums.ac.ir/article-1-1951-en.html
Zohre Sohrabi1  , Elham Ramezanpour *2
, Elham Ramezanpour *2  , Neda Rashidi3
, Neda Rashidi3  , Zahra Nouri Khaneghah1
, Zahra Nouri Khaneghah1  , Sohrab Nosrati1
, Sohrab Nosrati1  , Azizeh Barry4
, Azizeh Barry4  , Akram Zhianifard4
, Akram Zhianifard4 
 , Elham Ramezanpour *2
, Elham Ramezanpour *2  , Neda Rashidi3
, Neda Rashidi3  , Zahra Nouri Khaneghah1
, Zahra Nouri Khaneghah1  , Sohrab Nosrati1
, Sohrab Nosrati1  , Azizeh Barry4
, Azizeh Barry4  , Akram Zhianifard4
, Akram Zhianifard4 
1- Center for Educational Research in Medical Sciences (CERMS), Department of Medical Education, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
2- Center for Educational Research in Medical Sciences (CERMS), Department of Medical Education, School of Medicine, Iran University of Medical Sciences, Tehran, Iran ,elham6460@gmail.com
3- Department of Medical Education, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran. & Department operating room, school of paramedical sciences, Dezful University of Medical Sciences, Dezful, Iran.
4- Center for Educational Research in Medical Sciences(CERMS), Department of Medical Education, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
2- Center for Educational Research in Medical Sciences (CERMS), Department of Medical Education, School of Medicine, Iran University of Medical Sciences, Tehran, Iran ,
3- Department of Medical Education, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran. & Department operating room, school of paramedical sciences, Dezful University of Medical Sciences, Dezful, Iran.
4- Center for Educational Research in Medical Sciences(CERMS), Department of Medical Education, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 764 kb]
(704 Downloads)
| Abstract (HTML) (2967 Views)
Results
Table 2. The results of the ANOVA single-variable covariance analysis of positioning skills in operating room students in two control and intervention groups
Conclusion
The findings of the present study reveal that the reflective learning strategy has successfully led to a significant increase in post-test scores. A considerable difference in averages before and after implementation was seen between the group utilizing the reflective learning method and the one using the traditional approach. Notably, this research highlights that students provided with a well-structured and clear guidance for reflection can proceed beyond simply descriptive processes, participating in deeper levels of thought and thereby creating a more profound learning experience.
Full-Text: (781 Views)
Abstract
Background & Objective: Reflective learning is one of the most important learning models because it is based on the student's own experiences and is based on self-directed learning. This study aimed to investigate the effectiveness of reflective learning on scrub and circular skills in operating room students at the Iran University of Medical Sciences.
Material & Methods: The current research is a quasi-experimental pretest-posttest control group design. The research population consisted of 60 students in the 3rd and 5th semesters of their bachelor's degree in the operating room who were randomly assigned to two training groups: one that used the reflective learning approach and the other that used the conventional university method. The skills of the correct principles of scrub and circular were measured in both groups before and one week after the intervention using an objective structured clinical test (three stations). The research instrument was a researcher-made questionnaire that was valid and reliable. The data were analyzed by SPSS version 22.
Results: The two intervention and control groups were homogeneous and similar in terms of demographic characteristics (p > 0.05). The intervention group (reflective learning) demonstrated a significantly higher mean score in scrub and circular skills compared to the control group (traditional learning) (p < 0.05).
Conclusion: The results of the present study showed that the reflective learning teaching method has been able to significantly improve post-test scores. So that, with a structured and coherent guide for reflection, students can move beyond the description process to deeper levels of reflection and, thus, learning.
Material & Methods: The current research is a quasi-experimental pretest-posttest control group design. The research population consisted of 60 students in the 3rd and 5th semesters of their bachelor's degree in the operating room who were randomly assigned to two training groups: one that used the reflective learning approach and the other that used the conventional university method. The skills of the correct principles of scrub and circular were measured in both groups before and one week after the intervention using an objective structured clinical test (three stations). The research instrument was a researcher-made questionnaire that was valid and reliable. The data were analyzed by SPSS version 22.
Results: The two intervention and control groups were homogeneous and similar in terms of demographic characteristics (p > 0.05). The intervention group (reflective learning) demonstrated a significantly higher mean score in scrub and circular skills compared to the control group (traditional learning) (p < 0.05).
Conclusion: The results of the present study showed that the reflective learning teaching method has been able to significantly improve post-test scores. So that, with a structured and coherent guide for reflection, students can move beyond the description process to deeper levels of reflection and, thus, learning.
Introduction
One of the most important aspects of each person's existence in the modern world is education and learning. The quantity and quality of education have a significant impact on how a person's future is shaped (1). One of the variables related to learning is the learning style, which is known as one of the factors affecting the academic progress of students (2). Learning styles are cognitive, emotional, and physiological characteristics that indicate how to understand, act, and respond to the learning environment in a relatively constant manner (3). Learning approaches are very important in the education of the medical sciences because the main mission of teaching these disciplines is to train capable people who can improve the health of society. In many medical science centers in Iran, the lecture is the most common method of information transfer, which may not cover all aspects of education related to students' learning patterns (4).
Medical and paramedical fields, which are among the fields where education is based on theoretical and practical learning, come together. Therefore, having a correct and supportive educational approach can increase the level of students' learning (5). Clinical education is the most important and first source of learning and shaping the professional identity of medical students (6). Clinical education is a process in which the student gradually acquires skills by being at the patient's bedside and prepares to solve the patient's problem by using the acquired experiences and logical arguments. Students are therefore given invaluable opportunity to put principles they have learnt into practice through their interactions with the instructor and the surroundings. It transforms theoretical knowledge into a variety of mental and psychomotor skills required for patient care (7). Therefore, preparing students to take on different roles in the fields of healthcare services is one of the most important activities and goals of paramedical and medical faculties (8).
Studies on clinical training carried out in Iran indicate that this type of training lacks the necessary effectiveness (9, 10). Thus, knowledge of innovative pedagogical approaches is crucial to meeting the curriculum's goals as best as possible, especially in the medical sciences (11). Therefore, teachers need to use new teaching styles in clinical settings in order to use creative teaching-learning strategies (12). One of the methods whose effect has been confirmed in increasing the students' thinking power is reflective learning (13). In recent years, many sources and studies have paid attention to the need for reflective practice in education and supported its necessity in health professions education (14, 15). The classroom and clinical settings are not the same for teaching and learning. They are impacted by a number of variables, which can make it difficult to make corrections and draw lessons from bad experiences if they are not taken into account during the reflection process (16). As a metacognitive process, reflection takes place prior to, during, and following events. It encourages a more thorough comprehension of the subject, improves self-awareness of one's own talents, and makes it easier to handle similar situations in the future. This element can be considered an educational strategy that is based on self-directed learning and establishes a connection between the previous experiences of the learners and the current situation. It causes the integration of their theoretical learning and clinical practice (17).
Reflective learning occurs when the student and instructor simultaneously reflect on an educational experience and think about it (18). Evidence shows that reflection is a self-discovery process and has a significant impact on changing thoughts, performance, attitude, formation, and promoting critical thinking during clinical education (19, 20). Tashiro, citing Tamura, states that conceptually, reflection is a systemic cognitive process rooted in Dewey's educational philosophy. In reflection, a person deeply understands his experience through introspection, so he can improve his behavior or performance (21). The results of the study by Kolman and Nair colleagues showed that reflection corrects wrong training or practices that can potentially cause harm to the patient (22).
One of the most complex work environments in the health care system is the operating room. This complexity is revealed in issues related to the patient and the treatment protocol, as well as the use of high-level technology in the operating room (23). In this environment, students are faced with a wide range of surgical procedures and different clinical skills, which require them to have sufficient knowledge and skills during surgery. Students should be able to effectively combine their theoretical knowledge with the practical skills required in a variety of clinical situations (24). Meanwhile, research indicates that a significant percentage of students still lack the proficiency to carry out a number of essential tasks under supervision (25). For this reason, it is necessary to strengthen the necessary knowledge and skills of nurses in operating room environments (26). Therefore, the teaching methods in the clinic need to be changed (10), and clinical teachers need to use new teaching styles in clinical environments to use creative teaching-learning strategies (12). Mostly In clinical training, opportunities for analysis, interpretation, and reflection are frequently overlooked in favor of observation and practical labor.
Despite the unique qualities of the operating room, the sensitive nature of the procedures performed there, and the need to learn how to play a circular role and understand scrub principles, no previous research has looked at the effects of reflective learning on operating room students. Thus, this study was conducted with the aim of investigating the effectiveness of reflective learning on scrub and circular skills at the Iran University of Medical Sciences.
Medical and paramedical fields, which are among the fields where education is based on theoretical and practical learning, come together. Therefore, having a correct and supportive educational approach can increase the level of students' learning (5). Clinical education is the most important and first source of learning and shaping the professional identity of medical students (6). Clinical education is a process in which the student gradually acquires skills by being at the patient's bedside and prepares to solve the patient's problem by using the acquired experiences and logical arguments. Students are therefore given invaluable opportunity to put principles they have learnt into practice through their interactions with the instructor and the surroundings. It transforms theoretical knowledge into a variety of mental and psychomotor skills required for patient care (7). Therefore, preparing students to take on different roles in the fields of healthcare services is one of the most important activities and goals of paramedical and medical faculties (8).
Studies on clinical training carried out in Iran indicate that this type of training lacks the necessary effectiveness (9, 10). Thus, knowledge of innovative pedagogical approaches is crucial to meeting the curriculum's goals as best as possible, especially in the medical sciences (11). Therefore, teachers need to use new teaching styles in clinical settings in order to use creative teaching-learning strategies (12). One of the methods whose effect has been confirmed in increasing the students' thinking power is reflective learning (13). In recent years, many sources and studies have paid attention to the need for reflective practice in education and supported its necessity in health professions education (14, 15). The classroom and clinical settings are not the same for teaching and learning. They are impacted by a number of variables, which can make it difficult to make corrections and draw lessons from bad experiences if they are not taken into account during the reflection process (16). As a metacognitive process, reflection takes place prior to, during, and following events. It encourages a more thorough comprehension of the subject, improves self-awareness of one's own talents, and makes it easier to handle similar situations in the future. This element can be considered an educational strategy that is based on self-directed learning and establishes a connection between the previous experiences of the learners and the current situation. It causes the integration of their theoretical learning and clinical practice (17).
Reflective learning occurs when the student and instructor simultaneously reflect on an educational experience and think about it (18). Evidence shows that reflection is a self-discovery process and has a significant impact on changing thoughts, performance, attitude, formation, and promoting critical thinking during clinical education (19, 20). Tashiro, citing Tamura, states that conceptually, reflection is a systemic cognitive process rooted in Dewey's educational philosophy. In reflection, a person deeply understands his experience through introspection, so he can improve his behavior or performance (21). The results of the study by Kolman and Nair colleagues showed that reflection corrects wrong training or practices that can potentially cause harm to the patient (22).
One of the most complex work environments in the health care system is the operating room. This complexity is revealed in issues related to the patient and the treatment protocol, as well as the use of high-level technology in the operating room (23). In this environment, students are faced with a wide range of surgical procedures and different clinical skills, which require them to have sufficient knowledge and skills during surgery. Students should be able to effectively combine their theoretical knowledge with the practical skills required in a variety of clinical situations (24). Meanwhile, research indicates that a significant percentage of students still lack the proficiency to carry out a number of essential tasks under supervision (25). For this reason, it is necessary to strengthen the necessary knowledge and skills of nurses in operating room environments (26). Therefore, the teaching methods in the clinic need to be changed (10), and clinical teachers need to use new teaching styles in clinical environments to use creative teaching-learning strategies (12). Mostly In clinical training, opportunities for analysis, interpretation, and reflection are frequently overlooked in favor of observation and practical labor.
Despite the unique qualities of the operating room, the sensitive nature of the procedures performed there, and the need to learn how to play a circular role and understand scrub principles, no previous research has looked at the effects of reflective learning on operating room students. Thus, this study was conducted with the aim of investigating the effectiveness of reflective learning on scrub and circular skills at the Iran University of Medical Sciences.
Materials & Methods
Design and setting(s)
The current study employed a quasi-experimental pretest-posttest control group design (n=40) to examine the impact of reflective learning-based training on the development of scrubbing and circular skills in operating room students at Iran University of Medical Sciences from 2021 to 2022.
Participants and sampling
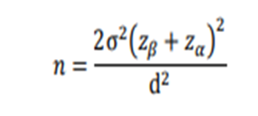
The study population included students in the 3rd and 5th semesters of the operating room course. The sample size was calculated using Formula 1 with a 95% confidence interval and a statistical power of 0.80. In this formula, the average and standard deviation parameters from the study conducted by Heidari and colleagues in 2023 (27) were used. Considering the probability of a 20% dropout rate and the possibility of outlier data, 30 people were considered for each group and randomly assigned to the test (30 people) and control (30 people) groups.
Design and setting(s)
The current study employed a quasi-experimental pretest-posttest control group design (n=40) to examine the impact of reflective learning-based training on the development of scrubbing and circular skills in operating room students at Iran University of Medical Sciences from 2021 to 2022.
Participants and sampling
The study population included students in the 3rd and 5th semesters of the operating room course. The sample size was calculated using Formula 1 with a 95% confidence interval and a statistical power of 0.80. In this formula, the average and standard deviation parameters from the study conducted by Heidari and colleagues in 2023 (27) were used. Considering the probability of a 20% dropout rate and the possibility of outlier data, 30 people were considered for each group and randomly assigned to the test (30 people) and control (30 people) groups.
Formula 1.
The participants were allocated to two groups using the random allocation method through Excel software: one group received reflective learning (30 students) while the other group followed traditional methods (30 students). The criteria for inclusion in the research were the students' willingness to participate in the study, and these students must have passed or were in the process of passing the theory and internship unit of the scrub and circular principles course. The exclusion criteria include the occurrence of unfortunate events during sessions and exams.
Figure 1 CONSORT flowchart of the study
Tools/Instruments
The title of the educational content included the skills of correct principles of scrubbing, positioning skills, and suturing skills in the same ways that were taught in both groups. The tool used in this research was the objective structured test observation checklist related to the principles of scrubbing, positioning skills, and suturing skills. Checklist questions were designed based on the blueprint, reading sources, and books, as well as consultation with operating room experts. The checklist consisted of 88 questions, with each question providing two choices: yes and no. The Position Station, which is divided into three parts (supine, lateral, and prone), consists of 23 questions, each with a corresponding score of 23. The typical Scrub Station comprised of 10 questions, resulting in a total score of 10. The Gun-Wearing Station, consisting of 10 questions, also had a score of 10. The Glove-Wearing Station consisted of 15 questions, resulting in a total score of 15. The Stitching Station was divided into three sections: simple stitch, far and near stitch, and new county stitch. Each section consisted of 10 questions, resulting in a total of 30 questions. The cumulative score for all sections combined was 30.
To validate the checklist, content validity was used, and the questions were given to ten faculty members of the operating room field, and their comments were applied as changes to the checklist. In this study, the internal correlation method (Cronbach's alpha) was used to measure the reliability of the checklist. Cronbach's alpha was calculated for the sub-fields of positioning skill, scrub principle skill, and suturing skill, respectively, 0.76, 0.85, and 0.87, and for the entire checklist, 0.91.
This study was carried out in three phases. The first phase of the research was before the intervention, and in this phase, the pre-test was conducted using an objective structured clinical test of scrub principles and circular skills in the clinical skills center of the faculty for a period of 25 minutes.
The second phase of the study was the implementation of the intervention. The training was done in two groups the day after the pre-test, and first, the training was done in the control group (lecture method). In this group, the educational content related to scrub and circular skills (28-29) was presented for eight hours (four two-hour sessions during two weeks). The educational content presented in the first and second sessions was taught theoretically in the form of lectures and PowerPoint, and the second two sessions were taught practically in the clinical skills center. After the completion of training in the traditional group, the educational content for the intervention group with an approach based on reflective learning was carried out by the researcher in the same way as in the first group (two theoretical sessions in the form of lectures, PowerPoint, and two practical sessions over two weeks). In the intervention group, at the beginning of the first session, the researcher gave explanations about reflective learning. Thus, reflective learning includes experience writing, summarizing, and seeking feedback. The reflection in the present study was reflection on action, according to which the researcher asked the students to write their clinical and classroom experience after each teaching session from the educational content (writing experience) and within 24 hours to share their reflections through sending an email to the professor. To determine the strengths and weaknesses, the professor also provided feedback on the reflections within 24 hours, which resulted in meaningful and deep learning and a way to improve performance. Also, the researcher asked the students to share their clinical experiences to improve the teaching-learning process with the teacher and other students in the class, and the role of the teacher was as a guide.
The third phase of this research was after the intervention. In this way, one week after the intervention, the post-test, like the pre-test, was conducted using the objective structured clinical test (OSCE) of the students of both groups in the Skill Lab of the faculty. This test included five stations, and the topics of the stations were determined based on the educational content mentioned about the principles of scrubs and circulars in the operating room field. In this way, the topics of station number one: principles of hand scrub, station number two: wearing a gown, station number three: wearing gloves, station number four: positioning, and station number five: stitching were defined. The entire structured clinical test was 25 minutes, and five minutes were considered for each test station.
An objectively structured test observation checklist was used in this study to evaluate skills linked to the correct principles of scrubbing, positioning, and stitching. Based on a template created for these specific domains, a set of 20 questions was created. The questions were submitted to eight members of the operating room board for face and content validity assessments to assure legitimacy. The questions were approved after integrating their comments. The Cronbach's alpha method was used to determine the checklist's reliability, yielding a computed value of 0.81.
To increase the internal and external validity of the research, measures were taken by the researchers, including: random allocation of samples, compliance with study protocols, strictness in managing variables, identifying disturbing variables and keeping them away, not sensitizing samples to intervention, lack of effect Rosenthal, and reducing the effect of disturbing and unwanted variables to a minimum.
Data collection method
To conduct this research, the researcher first introduced himself, and after stating the objectives and application of the results, if the students were willing to participate in the research and met the conditions for entering the study, they completed the informed consent form. Participating students were divided into two groups based on reflective learning (30 participants) and traditional speech training (30 participants) based on the academic semester and using the random allocation method based on Excel software. For the intervention group, code one and control group code two were considered.
Data analysis
Considering that SPSS v.22 software is freely available to everyone at our university, we also used this software for data analysis. We used descriptive statistics such as mean and standard deviation to describe the participants based on quantitative demographic variables and their scores on the nominal and ordinal scales before and after the intervention. We also used frequency and percentage to describe them based on qualitative variables. We also used inferential statistics to compare the homogeneity of the two groups based on demographic variables and scrub and circular skills before the intervention and to compare the participants with each other after the intervention. It should be noted that in order to use these statistical tests, the Kolmogorov-Smirnov test was used to measure the compliance of quantitative data with a normal distribution. The assumption of homogeneity of variances (post-test) was checked with Levene's test, and this assumption was also confirmed in the post-test stage (p < 0.05). In order to check another assumption of this test, i.e., the homogeneity of the covariance matrix in two groups, Box's M test was used, which was not statistically significant, and this means establishing the assumption of the equality of the covariance matrix. Since the important presuppositions of covariance analysis were established, the parametric test of covariance analysis can be used. We used the independent t-test to compare the mean of the control group with the intervention group. We also used the covariance test to check the influence of the independent variable on the dependent variable.
The title of the educational content included the skills of correct principles of scrubbing, positioning skills, and suturing skills in the same ways that were taught in both groups. The tool used in this research was the objective structured test observation checklist related to the principles of scrubbing, positioning skills, and suturing skills. Checklist questions were designed based on the blueprint, reading sources, and books, as well as consultation with operating room experts. The checklist consisted of 88 questions, with each question providing two choices: yes and no. The Position Station, which is divided into three parts (supine, lateral, and prone), consists of 23 questions, each with a corresponding score of 23. The typical Scrub Station comprised of 10 questions, resulting in a total score of 10. The Gun-Wearing Station, consisting of 10 questions, also had a score of 10. The Glove-Wearing Station consisted of 15 questions, resulting in a total score of 15. The Stitching Station was divided into three sections: simple stitch, far and near stitch, and new county stitch. Each section consisted of 10 questions, resulting in a total of 30 questions. The cumulative score for all sections combined was 30.
To validate the checklist, content validity was used, and the questions were given to ten faculty members of the operating room field, and their comments were applied as changes to the checklist. In this study, the internal correlation method (Cronbach's alpha) was used to measure the reliability of the checklist. Cronbach's alpha was calculated for the sub-fields of positioning skill, scrub principle skill, and suturing skill, respectively, 0.76, 0.85, and 0.87, and for the entire checklist, 0.91.
This study was carried out in three phases. The first phase of the research was before the intervention, and in this phase, the pre-test was conducted using an objective structured clinical test of scrub principles and circular skills in the clinical skills center of the faculty for a period of 25 minutes.
The second phase of the study was the implementation of the intervention. The training was done in two groups the day after the pre-test, and first, the training was done in the control group (lecture method). In this group, the educational content related to scrub and circular skills (28-29) was presented for eight hours (four two-hour sessions during two weeks). The educational content presented in the first and second sessions was taught theoretically in the form of lectures and PowerPoint, and the second two sessions were taught practically in the clinical skills center. After the completion of training in the traditional group, the educational content for the intervention group with an approach based on reflective learning was carried out by the researcher in the same way as in the first group (two theoretical sessions in the form of lectures, PowerPoint, and two practical sessions over two weeks). In the intervention group, at the beginning of the first session, the researcher gave explanations about reflective learning. Thus, reflective learning includes experience writing, summarizing, and seeking feedback. The reflection in the present study was reflection on action, according to which the researcher asked the students to write their clinical and classroom experience after each teaching session from the educational content (writing experience) and within 24 hours to share their reflections through sending an email to the professor. To determine the strengths and weaknesses, the professor also provided feedback on the reflections within 24 hours, which resulted in meaningful and deep learning and a way to improve performance. Also, the researcher asked the students to share their clinical experiences to improve the teaching-learning process with the teacher and other students in the class, and the role of the teacher was as a guide.
The third phase of this research was after the intervention. In this way, one week after the intervention, the post-test, like the pre-test, was conducted using the objective structured clinical test (OSCE) of the students of both groups in the Skill Lab of the faculty. This test included five stations, and the topics of the stations were determined based on the educational content mentioned about the principles of scrubs and circulars in the operating room field. In this way, the topics of station number one: principles of hand scrub, station number two: wearing a gown, station number three: wearing gloves, station number four: positioning, and station number five: stitching were defined. The entire structured clinical test was 25 minutes, and five minutes were considered for each test station.
An objectively structured test observation checklist was used in this study to evaluate skills linked to the correct principles of scrubbing, positioning, and stitching. Based on a template created for these specific domains, a set of 20 questions was created. The questions were submitted to eight members of the operating room board for face and content validity assessments to assure legitimacy. The questions were approved after integrating their comments. The Cronbach's alpha method was used to determine the checklist's reliability, yielding a computed value of 0.81.
To increase the internal and external validity of the research, measures were taken by the researchers, including: random allocation of samples, compliance with study protocols, strictness in managing variables, identifying disturbing variables and keeping them away, not sensitizing samples to intervention, lack of effect Rosenthal, and reducing the effect of disturbing and unwanted variables to a minimum.
Data collection method
To conduct this research, the researcher first introduced himself, and after stating the objectives and application of the results, if the students were willing to participate in the research and met the conditions for entering the study, they completed the informed consent form. Participating students were divided into two groups based on reflective learning (30 participants) and traditional speech training (30 participants) based on the academic semester and using the random allocation method based on Excel software. For the intervention group, code one and control group code two were considered.
Data analysis
Considering that SPSS v.22 software is freely available to everyone at our university, we also used this software for data analysis. We used descriptive statistics such as mean and standard deviation to describe the participants based on quantitative demographic variables and their scores on the nominal and ordinal scales before and after the intervention. We also used frequency and percentage to describe them based on qualitative variables. We also used inferential statistics to compare the homogeneity of the two groups based on demographic variables and scrub and circular skills before the intervention and to compare the participants with each other after the intervention. It should be noted that in order to use these statistical tests, the Kolmogorov-Smirnov test was used to measure the compliance of quantitative data with a normal distribution. The assumption of homogeneity of variances (post-test) was checked with Levene's test, and this assumption was also confirmed in the post-test stage (p < 0.05). In order to check another assumption of this test, i.e., the homogeneity of the covariance matrix in two groups, Box's M test was used, which was not statistically significant, and this means establishing the assumption of the equality of the covariance matrix. Since the important presuppositions of covariance analysis were established, the parametric test of covariance analysis can be used. We used the independent t-test to compare the mean of the control group with the intervention group. We also used the covariance test to check the influence of the independent variable on the dependent variable.
Results
This study used a quasi-experimental pretest-posttest control group design to investigate the impact of reflective learning-based training on the skills related to scrubbing and circular concepts among 60 students in the 3rd and 5th semesters of the operating room course. The participants had a mean age of (Control Groups: 21 ± 2.65 & Intervention Groups: 21 ± 1.79), with a correlation coefficient (R) of 0.212 and p-value of 0.716. Among them, 32 students (53.33%) were male, and 28 (46.66%) were female, with an associated correlation coefficient (R) of 0.188 and p-value of 0.081. Additionally, 52 students (86.70%) were single, while 8 (13.30%) were married. No statistically significant difference was noticed between the two groups in terms of demographic factors (p = 0.074).
After the end of the training sessions and conducting an objective structured clinical test, the mean score of scrub principles and circular skills before and after the intervention was compared in both groups.
The results of the independent t-test showed that there was no statistically significant difference between the mean scores of the pre-test in the three skill areas of positioning, principles of scrubbing, and suturing in the operating room between the two control and intervention groups (p > 0.05). Therefore, the two groups were identical, homogeneous, or similar in terms of the pre-test (Table 1).
After the end of the training sessions and conducting an objective structured clinical test, the mean score of scrub principles and circular skills before and after the intervention was compared in both groups.
The results of the independent t-test showed that there was no statistically significant difference between the mean scores of the pre-test in the three skill areas of positioning, principles of scrubbing, and suturing in the operating room between the two control and intervention groups (p > 0.05). Therefore, the two groups were identical, homogeneous, or similar in terms of the pre-test (Table 1).
Table 1. Pre-test comparison of two control and intervention groups in positioning skills, principles of scrubbing, and suturing skills
| Research variables Groups |
Pre-test | Sig. | |||
| Number | Mean | SD | |||
| Positioning skills | Control | 30 | 14.03 | 1.99 | t= 1.852, p = 0.083 |
| Intervention | 30 | 14.03 | 2.16 | ||
| Principles of scrubbing | Control | 30 | 5.23 | 1.43 | t= 1.623, p = 0.264 |
| Intervention | 30 | 5.43 | 1.50 | ||
| suturing skills | Control | 30 | 19.96 | 1.06 | t= 2.602, p = 0.311 |
| Intervention | 30 | 19.23 | 1.35 | ||
Note: p-value less than 0.05 was considered significant.
Abbreviations: SD, standard deviation; Sig, significance; t, t-test; p, probability-value.
As shown in Table 2, results of the analysis of covariance suggest a significant difference in the mean scores of the post-test for positioning skills between the two groups. The control groups exhibited a mean score of 14.03 ± 2.42, while the intervention group demonstrated a mean score of 20.03 ± 2.86.
Table 2. The results of the ANOVA single-variable covariance analysis of positioning skills in operating room students in two control and intervention groups
| Test power | Eta2 | level of significance | Average of squares | F | Degrees of freedom | sum of squares | |
| 1.000 | 0.592 | 0.001 | 193.488 | 41.357 | 2 | 386.976 | Homogeneity of the regression slope |
| 0.636 | 0.088 | 0.022 | 19.520 | 5.505 | 1 | 19.520 | Pre-test effect |
| 1.000 | 0.674 | 0.001 | 418.357 | 117.985 | 1 | 418.357 | Intergroup |
| 3.546 | 57 | 202.114 | Error | ||||
| 59 | 653.650 | Total |
Note: p-value less than 0.05 was considered significant.
Abbreviations: F, F test.
Abbreviations: F, F test.
Also, the results of the analysis of covariance in the comparison of the basic skills of scrubbing and suturing skills showed that there is a statistically significant increase between the mean scores of these skills compared to before the intervention (Table 3, Table 4).
Table 3. Results of univariate covariance analysis of the skills of scrub principles in operating room students in two control and intervention groups
| Test power | Eta2 | level of significance | Average of squares | F | Degrees of freedom | Sum of squares | |
| 1.000 | 0.439 | 0.001 | 39.853 | 22.283 | 2 | 79.707 | Homogeneity of the regression slope |
| 0.460 | 0.059 | 0.064 | 4.579 | 3.573 | 1 | 4.579 | Pre-test effect |
| 1.000 | 0.593 | 0.001 | 106.554 | 83.138 | 1 | 106.554 | Intergroup |
| 1.282 | 57 | 73.054 | Error | ||||
| 59 | 181.650 | Total |
Note: p-value less than 0.05 was considered significant.
Abbreviations: F, F test.
Abbreviations: F, F test.
Table 4.The results of the univariate covariance analysis of suturing skills in operating room students in two control and intervention groups
| Test power | Eta2 | Level of significance | Average of squares | F test | Degrees of freedom | Sum of squares | |
| 1.000 | 0.800 | 0.001 | 330.172 | 114.344 | 2 | 660.344 | Homogeneity of the regression slope |
| 0.120 | 0.011 | 0.437 | 1.680 | 0.611 | 1 | 1.680 | Pre-test effect |
| 1.000 | 0.805 | 0.001 | 644.889 | 234.750 | 1 | 644.889 | Intergroup |
| 2.747 | 57 | 156.587 | Error | ||||
| 59 | 824.933 | Total |
Note: p-value less than 0.05 was considered significant.
Abbreviations: F, F test.
Abbreviations: F, F test.
Discussion
The present study aimed to investigate the effect of reflective learning-based training on scrub and circular skills in operating room students at the Iran University of Medical Sciences. The results of the present study showed that there was no statistical difference between the average score of the pre-test of scrub principles and circular skills before the intervention in the two groups. Also, a statistically significant difference was observed between the average scores of both groups one week after the intervention, and this increase in average scores in the reflective learning group had a greater increase than in the traditional teaching group, which proves that the reflective learning method has been able to significantly improve post-test scores. So, the difference between the mean before and after was observed in the reflective learning method group compared to the traditional method. Despite the fact that reflection is considered a basic learning process and the positive results of reflective practice can affect personal and professional development, improving the quality of care (29), it has been neglected in clinical education (30). In line with the results of the present study, Bjerkvi's research in 2019 showed that reflective writing is a tool for students' professional learning and increases their reasoning skills and awareness in clinical situations (31). Therefore, the use of training based on reflective learning has had a greater effect on positioning skills among operating room students than in the control group. And it has increased the skill of positioning in operating room students. Also, the identified findings of Barbagallo and Bagheri's review studies indicate that reflecting practice is considered a key skill to bridge the gap between theory and practical experiences (32, 33). This argument was supported in a study by Persson et al. (2015), which showed that reflection “on practice” is an important post-clinical situation to ensure that students understand and record what happened and how it might have been done differently. The authors also state that the more the process is implemented, the more the reflection changes from simple descriptions of content and scenarios to assessments and actual reflective practice (34).
The reflection employed in this study, characterized as reflection on action, and the findings indicate that the use of education based on reflective learning has created a deeper understanding of the subject, increased self-awareness, and promoted the learning of scrub and circular skills. In his research, Donald Shun proposed the two concepts of reflection in action and reflection on action. Based on Shun's thoughts, the purpose of reflecting on the learning process is to create meaningful and deep learning. In explaining this finding, we can conclude that reflection is a metacognitive process that occurs before, during, or after situations, and its purpose is to increase the learners' understanding of themselves and the situation so that they act more consciously in a similar situation in the future (17). The results of Coleman's study in 2017, which was conducted on nursing students, similar to the present study, showed that reflection corrects wrong training or practices that can potentially cause harm to the patient. Writing reflection is one of the essentials of the learning activity, which can make students aware of and evaluate their situation, identify educational problems and learning opportunities, and determine the strengths and weaknesses of the student and even the educational system (22).
As in this study, providing teacher feedback was used as a necessity to achieve learning; this importance was also raised by Williams in such a way that ensuring the correct guidance of students through the thinking process is supported. To develop such a skill in reflection, not only training and written structure are emphasized, but also the ability to discuss the process and provide feedback is necessary (35). On the other hand, the findings of Bagheri's study, which aimed at investigating the impact of reflective learning based on clinical scenarios on the moral sensitivity of nursing students, did not show a significant difference between before and after the intervention, which is not consistent with the results of the present study. The reason for this difference is that the use of such new approaches, especially considering different cultural pedagogies, can include more complex dimensions to be effective. Also, educators need formal training to facilitate reflective learning activities (36). Also, the results of various studies showed that training in the rethinking method has a significant effect on knowledge, skills, attitudes, and professional performance in different nursing, medical, dental, and operating room groups (37-42).
Considering the type of study (quasi-experimental), we had some limitations, including a small sample size and a lack of generalizability of the results. The current study was just conducted on the students in the operating room. Thus, generalizing the findings to other fields of the medical sciences is somewhat troublesome. Therefore, it is recommended that reflection, as a main component of clinical education throughout the practical courses, be considered among students in the operating room. It is recommended to use samples with a large volume. And this intervention should be done in other groups as well.
The reflection employed in this study, characterized as reflection on action, and the findings indicate that the use of education based on reflective learning has created a deeper understanding of the subject, increased self-awareness, and promoted the learning of scrub and circular skills. In his research, Donald Shun proposed the two concepts of reflection in action and reflection on action. Based on Shun's thoughts, the purpose of reflecting on the learning process is to create meaningful and deep learning. In explaining this finding, we can conclude that reflection is a metacognitive process that occurs before, during, or after situations, and its purpose is to increase the learners' understanding of themselves and the situation so that they act more consciously in a similar situation in the future (17). The results of Coleman's study in 2017, which was conducted on nursing students, similar to the present study, showed that reflection corrects wrong training or practices that can potentially cause harm to the patient. Writing reflection is one of the essentials of the learning activity, which can make students aware of and evaluate their situation, identify educational problems and learning opportunities, and determine the strengths and weaknesses of the student and even the educational system (22).
As in this study, providing teacher feedback was used as a necessity to achieve learning; this importance was also raised by Williams in such a way that ensuring the correct guidance of students through the thinking process is supported. To develop such a skill in reflection, not only training and written structure are emphasized, but also the ability to discuss the process and provide feedback is necessary (35). On the other hand, the findings of Bagheri's study, which aimed at investigating the impact of reflective learning based on clinical scenarios on the moral sensitivity of nursing students, did not show a significant difference between before and after the intervention, which is not consistent with the results of the present study. The reason for this difference is that the use of such new approaches, especially considering different cultural pedagogies, can include more complex dimensions to be effective. Also, educators need formal training to facilitate reflective learning activities (36). Also, the results of various studies showed that training in the rethinking method has a significant effect on knowledge, skills, attitudes, and professional performance in different nursing, medical, dental, and operating room groups (37-42).
Considering the type of study (quasi-experimental), we had some limitations, including a small sample size and a lack of generalizability of the results. The current study was just conducted on the students in the operating room. Thus, generalizing the findings to other fields of the medical sciences is somewhat troublesome. Therefore, it is recommended that reflection, as a main component of clinical education throughout the practical courses, be considered among students in the operating room. It is recommended to use samples with a large volume. And this intervention should be done in other groups as well.
Conclusion
The findings of the present study reveal that the reflective learning strategy has successfully led to a significant increase in post-test scores. A considerable difference in averages before and after implementation was seen between the group utilizing the reflective learning method and the one using the traditional approach. Notably, this research highlights that students provided with a well-structured and clear guidance for reflection can proceed beyond simply descriptive processes, participating in deeper levels of thought and thereby creating a more profound learning experience.
Recognizing the significance of emphasizing active and student-centered learning methods, and acknowledging the necessity for learners to actively participate in the educational process to acquire professional abilities and competences, as well as to foster a positive learning environment, the incorporation of structured reflection opportunities in clinical education is strongly recommended. Emphasizing care, strengthening critical thinking, connecting theory and practice, and promoting self-regulation mechanisms through reflective courses underline the necessity of adding reflection into the clinical education program.
Ethical considerations
The present study was conducted after the approval of a research project at the Iran University of Medical Sciences with the ethical code IR.IUMS.FMD.REC.1400.522.
Artificial intelligence utilization for article writing
No.
Acknowledgments
The researchers would like to thank all students, teachers and of the head of operating room department at Iran University of Medical Sciences for their collaboration and participation in this project.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Disclosure
The present work is the outcome of a research proposal from the Iran University of Medical Sciences.
Author contributions
Z.S. and E.R. were involved in the conception and design of the work, the analysis, and interpretation of the data, the drafting, and the final approval of the manuscript. Z.N., K.H., and S.N collected data and participated in drafting the manuscript. N.R. contributed to the data collection and analysis. All authors read and approved the final manuscript.
Supporting resources
This study was conducted with the financial support of the Medical Science Education Research Center (CERMS) of the Iran University of Medical Sciences.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
The present study was conducted after the approval of a research project at the Iran University of Medical Sciences with the ethical code IR.IUMS.FMD.REC.1400.522.
Artificial intelligence utilization for article writing
No.
Acknowledgments
The researchers would like to thank all students, teachers and of the head of operating room department at Iran University of Medical Sciences for their collaboration and participation in this project.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Disclosure
The present work is the outcome of a research proposal from the Iran University of Medical Sciences.
Author contributions
Z.S. and E.R. were involved in the conception and design of the work, the analysis, and interpretation of the data, the drafting, and the final approval of the manuscript. Z.N., K.H., and S.N collected data and participated in drafting the manuscript. N.R. contributed to the data collection and analysis. All authors read and approved the final manuscript.
Supporting resources
This study was conducted with the financial support of the Medical Science Education Research Center (CERMS) of the Iran University of Medical Sciences.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Article Type : Orginal Research |
Subject:
Medical Education
Received: 2023/05/24 | Accepted: 2024/01/13 | Published: 2024/05/10
Received: 2023/05/24 | Accepted: 2024/01/13 | Published: 2024/05/10
References
1. Mirkazehi rigi Z, Tafzoli M, Karimi Moneghi H, Taghipour A, Shekhi F. The effect of teaching based on reflective education on management skills of preeclampsia in midwifery students. Research in Medical Education, 2020;12 (2):1-9. [Article]
2. Eppich W, Cheng A. Promoting excellence and reflective learning in simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Journal of the Society for Simulation in Healthcare. 2015;10(2):106-15. [DOI]
3. Wolfson AJ. Teaching progressions and learning progressions. International :union: of Biochemistry and Molecular Biology. 2019;47(5):493-497. [DOI]
4. Walsh P, Owen PA, Mustafa N, Beech R. Learning and teaching approaches promoting resilience in student nurses: An integrated review of the literature. Nurse Education in Practice. 2020;45:102748. [DOI]
5. Muir F, Bruce J, McConville K. Teaching, reflecting, and learning: The value of an intercalated medical education programme. Medical Teacher. 2020;42(5):523-528. [DOI]
6. Franco RS, Franco CAGDS, Severo M, Ferreira MA, Karnieli-Miller O. Reflective writing in the teaching of communication skills for medical students-A systematic review. Patient Education and Counseling. 2022;105(7):1842-1851. [DOI]
7. Karnieli-Miller O. Reflective practice in the teaching of communication skills. Patient Education and Counseling. 2020;103(10):2166-2172. [DOI]
8. Parazpardanjani S. Fereiduni Moghadam M. Clinical education from Tehran nursing students’ point of view. Journal of Education & Development of Medical Sciences. 2008;5(2):102-11.
9. Mohamed M, Rashid RA, Alqaryouti MH. Conceptualizing the complexity of reflective practice in education. Frontiers in psychology. 2022;13:1008234. [DOI]
10. Woldt JL, Nenad MW. Reflective writing in dental education to improve critical thinking and learning: A systematic review, European Journal of Dental Education. 2021;85(6):778-785. [DOI]
11. Shaikh F, Schorscher P. Medical students' perspectives on 'teaching, reflecting, and learning'. Medical Teacher. 2020;42(10):1195-1196. [DOI]
12. Sevenhuysen S, Thorpe J, Molloy E, Keating J, Haines T. Peer-assisted learning in education of allied health professional students in the clinical setting: a systematic review. Journal of Allied Health. 2017;46(1):26-35. PMID: 28255594.
13. Haghani F, Jafari Mianaei S, Ehsani M. Reflective learning and teaching: A review. Iranian Journal of Medical Education. 2014;13(11):989-98. [DOI]
14. Graham MM, Johns C. Becoming student kind: A nurse educator's reflexive narrative inquiry. Nurse Education in Practice. 2019;39:111-116. [DOI]
15. Hem MH, Molewijk B, Gjerberg E, Lillemoen L, Pedersen R. The significance of ethics reflection groups in mental health care: a focus group study among health care professionals. BMC Medical Ethics. 2018;19:1-14. [DOI]
16. Raterink G. Reflective journaling for critical thinking development in advanced practice registered nurse students. Journal of Nursing Education. 2016;55(2):101-4. [DOI]
17. Schön DA. The reflective practitioner: How professionals think in action: Routledge; 2017.
18. Graham MM. Navigating professional and personal knowing through reflective storytelling amidst Covid-19. Journal of Holistic Nursing. 2022;40(4):372-382. [DOI]
19. Chen M, Ye L, Weng Y. Blended teaching of medical ethics during COVID-19: practice and reflection. BMC Medical Education. 2022;22(1):361. [DOI]
20. Bulman C, Forde-Johnson C, Griffiths A, et al. The development of peer reflective supervision amongst nurse educator colleagues: an action research project. Nurse Education Today. 2016; 45:148-55. [DOI]
21. Tashiro J, Shimpuku Y, Naruse K, Matsutani M. Concept analysis of reflection in nursing professional development. Japan Journal of Nursing Science. 2013;10(2):170-9. [DOI]
22. Coleman D, Willis DS. Reflective writing: The student nurse's perspective on reflective writing and poetry writing. Nurse Education Today. 2015; 35(7):906-11. [DOI]
23. Schlegel EFM, Cassara M, Olvet DM, Fornari A. The reflective teaching log (RTL): Effective documentation of participatory teaching requirements. Medical Science Educator. 2019;29(2):351-353. [DOI]
24. Lim JY, Ong SYK, Ng CYH, et al. A systematic scoping review of reflective writing in medical education. BMC Medical Education. 2023;23(1):12. [DOI]
25. Alotaibi HM, Alharithy R, Alotaibi HM. Importance of the reflective logbook in improving the residents' perception of reflective learning in the dermatology residency program in Saudi Arabia: Findings from a cross-sectional study. BMC Medical Education. 2022;22(1):862. [DOI]
26. Bleakley A, Allard J, Hobbs A. Towards culture change in the operating theatre: embedding a complex educational intervention to improve teamwork climate. Medical Teacher. 2012;34(9): e635-e40. [DOI]
27. Heidari F, Mottaghi R. The effectiveness of life skills training on cognitive flexibility and quality of life in elderly people with diabetes mellitus type-2: A quasi-experimental study. The Journal of Rafsanjan University of Medical Sciences. 2023;22(4):367-384.
28. Privitera GJ, Delzell LA. Quasi-experimental and single-case experimental designs. Research Methods for Education. 2019:333-70.
29. Ramezani, G., Khoshsokhan, K., Moradi, E., Soltani Arabshahi, K., & Rasouli, D. (2023). Effect of Communication Skills Virtual Module Based on the Calgary-Cambridge Model on the Attitude and Performance of Medical Students. Strides in Development of Medical Education, 20(1), 195-203. [DOI]
30. Keshmiri F, Asgari P, Bahramnezhad F. Opportunity to reflection: The missing link in clinical education. The Journal of Medical Education and Development. 2018;13(3):252-9.
31. Galutira GD. Theory of reflective practice in nursing. International Journal of Nursing Science. 2018;8(3):51-6. [DOI]
32. Bjerkvik LK, Hilli Y. Reflective writing in undergraduate clinical nursing education: A literature review. Nurse Education in Practice. 2019;35:32-41. [DOI]
33. Bagheri M, Haghani F. Take on issues and uses of reflection and reflective practice in nursing education. Journal of Medical Education and Development. 2019;14(2):123-135. [DOI]
34. Barbagallo MS. Completing reflective practice post undergraduate nursing clinical placements: A literature review. Teaching and Learning in Nursing. 2019;14(3):160-5. [DOI]
35. Persson EK, Kvist LJ, Ekelin M. Analysis of midwifery students' written reflections to evaluate progression in learning during clinical practice at birthing units. Nurse Education in Practice. 2015;15(2):134-40. [DOI]
36. Lane AS, Roberts C. Contextualised reflective competence: a new learning model promoting reflective practice for clinical training. BMC Medical Education. 2022;22(1):71. [DOI]
37. Bagheri M, Mohammadi Pelarti A, Karimi S. The effect of reflective learning based on clinical scenarios on the moral sensitivity of nursing students. Education and Ethics in Nursing. 2022;11(1-2):39-46.
38. Kazemipoor M, Keshmiri F. Assessment of reflection-based education on reflective thinking skills of dental students: A quasi experimental study. Journal of Medical Education and Development. 2023;16(49):1-6. [DOI]
39. Azizi M, Ramezani G, Karimi E, Hayat AA, Faghihi SA, Keshavarzi MH. A comparison of the effects of teaching through simulation and the traditional method on nursing students' self-efficacy skills and clinical performance: a quasi-experimental study. BMC Nursing. 2022;21(1):1-8. [DOI]
40. Heng Q, Chu L. Self-efficacy, reflection, and resilience as predictors of work engagement among English teachers. Frontiers in Psychology. 2023;14:1160681. [DOI]
41. Machost H, Stains M. Reflective practices in education: A primer for practitioners. CBE Life Sciences Education. 2023;22(2):es2. [DOI]
42. Oo TZ, Habók A, Józsa K. Qualifying method-centered teaching approaches through the reflective teaching model for reading comprehension. Education Sciences. 2023;13(5):473. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |