Mon, Feb 2, 2026
[Archive]
Volume 16, Issue 49 (2023)
J Med Edu Dev 2023, 16(49): 36-43 |
Back to browse issues page
Ethics code: KE/FK/0234/EC/2021
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ismail N A, Jamil N A. Mental health of pre-clinical medical students in Indonesia during the first year of the COVID-19 pandemic: A reflection. J Med Edu Dev 2023; 16 (49) :36-43
URL: http://edujournal.zums.ac.ir/article-1-1783-en.html
URL: http://edujournal.zums.ac.ir/article-1-1783-en.html
1- Faculty of Medicine, Universitas Islam Indonesia, Yogyakarta, Indonesia , naufalarifismail@gmail.com
2- Department of Public Health, Faculty of Medicine, Universitas Islam Indonesia, Yogyakarta, Indonesia
2- Department of Public Health, Faculty of Medicine, Universitas Islam Indonesia, Yogyakarta, Indonesia
Full-Text [PDF 396 kb]
(1887 Downloads)
| Abstract (HTML) (3457 Views)
Full-Text: (1154 Views)
Abstract
Background & Objective: Perceived awareness and concern for mental health issues among students in Indonesia are still lacking, proceeding before and during the coronavirus disease 2019 (COVID-19) pandemic. In order to gain future benefits, this study evaluates pre-clinical medical students' mental health during the first year of the COVID-19 pandemic in Indonesia.
Materials & Methods: This cross-sectional study was conducted on pre-clinical medical students at the Faculty of Medicine, Universitas Islam Indonesia (FM UII), Yogyakarta, Indonesia, in April 2021. A total sampling method was employed. Participants completed online self-reported questionnaires, including socio-demographic data and the Depression, Anxiety, and Stress Scale-21 (DASS-21) questionnaire to evaluate mental health. Descriptive, bivariate, and multivariate analysis was performed.
Results: A total of 273 pre-clinical medical students were included in this study. They suffered from depression (35.2%) and stress (40.3%) more than a third and about half suffered from anxiety (50.2%). Females were more likely to have depression (AOR: 2.22; 95%CI: 1.19 to 4.15), anxiety (2.56; 1.42 to 4.61), and stress (3.44; 1.81 to 6.54) than males. Anxiety was less common in medical students in their second (0.48; 0.23 to 0.98) and third (0.29; 0.13 to 0.67) years than in the first year. Being a third-year student was a protective factor for stress (0.38; 0.17 to 0.87).
Conclusion: A high prevalence of depression, anxiety, and stress among pre-clinical students was observed. This study can become a reflection for educational institutions and policymakers to prepare good strategies to maintain pre-clinical students’ quality and mental health during and after COVID-19 pandemic.
Materials & Methods: This cross-sectional study was conducted on pre-clinical medical students at the Faculty of Medicine, Universitas Islam Indonesia (FM UII), Yogyakarta, Indonesia, in April 2021. A total sampling method was employed. Participants completed online self-reported questionnaires, including socio-demographic data and the Depression, Anxiety, and Stress Scale-21 (DASS-21) questionnaire to evaluate mental health. Descriptive, bivariate, and multivariate analysis was performed.
Results: A total of 273 pre-clinical medical students were included in this study. They suffered from depression (35.2%) and stress (40.3%) more than a third and about half suffered from anxiety (50.2%). Females were more likely to have depression (AOR: 2.22; 95%CI: 1.19 to 4.15), anxiety (2.56; 1.42 to 4.61), and stress (3.44; 1.81 to 6.54) than males. Anxiety was less common in medical students in their second (0.48; 0.23 to 0.98) and third (0.29; 0.13 to 0.67) years than in the first year. Being a third-year student was a protective factor for stress (0.38; 0.17 to 0.87).
Conclusion: A high prevalence of depression, anxiety, and stress among pre-clinical students was observed. This study can become a reflection for educational institutions and policymakers to prepare good strategies to maintain pre-clinical students’ quality and mental health during and after COVID-19 pandemic.
Introduction
Since the pandemic of the coronavirus disease 2019 (COVID-19) has spread worldwide, people’s daily lives have changed dramatically. This situation makes policymakers impose social restrictions, especially in Indonesia, which is semi-lockdown to reduce the risk of exposure to infection. As a result, daily life becomes very limited, whereas there is less social life and physical and outdoor activities. According to the Indonesian Ministry of Education instruction, learning at schools and universities is transforming online from March 2020 until an unspecified date (1).
This unprecedented quarantine period has had a devastating impact on students’ mental health. For example, Fawaz and Samaha's (2020) study in Lebanon reported that a sudden change to an online learning model led to increased symptoms of depression and anxiety in university students (2). A study by Hamaideh et al. (2022) that evaluated mental health in Jordan reported that students are vulnerable to severe mental illness during the quarantine period if no intervention is indicated (3). Furthermore, Seetan et al. (2021) study among medical students during the pandemic reported that more than half suffered from severe mental disorders and were concerned about being unable to get to their clinical and laboratory sessions (4).
Although the COVID-19 pandemic causes students mental health distress, particularly medical students in the pre-clinical period were considered to have higher mental health distress levels, including depression, anxiety, and stress (5,6). This condition is caused by their learning load and more competitive and psychologically high-pressure environment (5). It means that the COVID-19 pandemic has become an agent that worsens the mental health conditions of students. Whereas pre-clinical medical students are prepared to become competent and qualified health personnel and have good mental health.
Even though the pandemic has been going on for a year, appropriate interventions and strategies from policymakers and educational institutions to maintain the quality and mental health of pre-clinical medical students in Indonesia have not been implemented properly. It seems more likely due to the lack of awareness and concern for mental health issues among students in Indonesia, lasting since before the COVID-19 pandemic. It is expected to have a negative impact on subsequent conditions. Studies on pre-clinical students are expected to be able to measure the impact of COVID-19 on mental health and become a reference and reflection for formulating effective strategies and interventions. This study aims to evaluate mental health consisting of depression, anxiety, and stress among pre-clinical medical students and related factors during the first year of the COVID-19 pandemic in Indonesia, which is expected to enhance awareness and concern for policymakers and educational institutions.
This unprecedented quarantine period has had a devastating impact on students’ mental health. For example, Fawaz and Samaha's (2020) study in Lebanon reported that a sudden change to an online learning model led to increased symptoms of depression and anxiety in university students (2). A study by Hamaideh et al. (2022) that evaluated mental health in Jordan reported that students are vulnerable to severe mental illness during the quarantine period if no intervention is indicated (3). Furthermore, Seetan et al. (2021) study among medical students during the pandemic reported that more than half suffered from severe mental disorders and were concerned about being unable to get to their clinical and laboratory sessions (4).
Although the COVID-19 pandemic causes students mental health distress, particularly medical students in the pre-clinical period were considered to have higher mental health distress levels, including depression, anxiety, and stress (5,6). This condition is caused by their learning load and more competitive and psychologically high-pressure environment (5). It means that the COVID-19 pandemic has become an agent that worsens the mental health conditions of students. Whereas pre-clinical medical students are prepared to become competent and qualified health personnel and have good mental health.
Even though the pandemic has been going on for a year, appropriate interventions and strategies from policymakers and educational institutions to maintain the quality and mental health of pre-clinical medical students in Indonesia have not been implemented properly. It seems more likely due to the lack of awareness and concern for mental health issues among students in Indonesia, lasting since before the COVID-19 pandemic. It is expected to have a negative impact on subsequent conditions. Studies on pre-clinical students are expected to be able to measure the impact of COVID-19 on mental health and become a reference and reflection for formulating effective strategies and interventions. This study aims to evaluate mental health consisting of depression, anxiety, and stress among pre-clinical medical students and related factors during the first year of the COVID-19 pandemic in Indonesia, which is expected to enhance awareness and concern for policymakers and educational institutions.
Material & Methods
Design and setting(s)
This single institution-based cross-sectional study was conducted at the Faculty of Medicine, Universitas Islam Indonesia (FM UII), Yogyakarta, Indonesia, from 4 to 12 April 2021.
Participants and sampling
According to faculty administration data, participants were recruited from a total of FM UII pre-clinical students (first to third year).
Tools/Instruments
The self-reported questionnaire consists of two parts: 1) Socio-demographic data, including gender, age, year of study, weight, and height; 2) The Indonesian version of the Depression, Anxiety and Stress Scale-21 (DASS-21) questionnaire to evaluate mental health status consisting levels of depression, anxiety, and stress that has previously been tested in several countries including Indonesia (7–9). The overall reliability coefficient (McDonald’s omega) of the Indonesian version of DASS-21 questionnaire was 0.910 and for each sub-scale was 0.794, 0.785, and 0.800 for depression, anxiety, and stress (10). The sub-scores of depression, anxiety, and stress were summed up and then classified into five categories: normal, mild, moderate, severe, and extremely severe for descriptive data. In bivariate and multivariate logistic regression analysis, mental health status was classified into two categories: normal or depressed (5 to ≥14), anxious (4 to ≥10), or stressed (8 to ≥17). BMI was calculated using a person’s weight in kilograms divided by height in meters squared (BMI=kg/m2). Then, BMI was classified into three categories according to the Indonesian Ministry of Health: 1) Normal (18.5 to 25.0); 2) Underweight (≤17.0 to 18.4); 3) Overweight (25.1 to ≥27.0) (11).
Data collection methods
Data collection was carried out by distributing a Google Form link containing a self-reported questionnaire that was filled out voluntarily, anonymously, and with consent through social media such as WhatsApp and Line. Participants were required to log in to their email accounts to avoid duplicate data. Male and female pre-clinical medical students who have participated in online learning since it was enacted and had no history of mental illness were eligible to be included in this study.
Data analysis
All data were analyzed using SPSS version 26 (IBM, Chicago, IL, USA). Categorical data were displayed as frequency and percentage. Bivariate analysis using the Chi-Square test was conducted to compare the difference in proportions between groups. Multivariate logistic regression analysis to identify predictors for depression, anxiety, and stress was also carried out by including variables with a P-value <0.25 in the bivariate analysis. A P-value of <0.05 was considered statistically significant.
This single institution-based cross-sectional study was conducted at the Faculty of Medicine, Universitas Islam Indonesia (FM UII), Yogyakarta, Indonesia, from 4 to 12 April 2021.
Participants and sampling
According to faculty administration data, participants were recruited from a total of FM UII pre-clinical students (first to third year).
Tools/Instruments
The self-reported questionnaire consists of two parts: 1) Socio-demographic data, including gender, age, year of study, weight, and height; 2) The Indonesian version of the Depression, Anxiety and Stress Scale-21 (DASS-21) questionnaire to evaluate mental health status consisting levels of depression, anxiety, and stress that has previously been tested in several countries including Indonesia (7–9). The overall reliability coefficient (McDonald’s omega) of the Indonesian version of DASS-21 questionnaire was 0.910 and for each sub-scale was 0.794, 0.785, and 0.800 for depression, anxiety, and stress (10). The sub-scores of depression, anxiety, and stress were summed up and then classified into five categories: normal, mild, moderate, severe, and extremely severe for descriptive data. In bivariate and multivariate logistic regression analysis, mental health status was classified into two categories: normal or depressed (5 to ≥14), anxious (4 to ≥10), or stressed (8 to ≥17). BMI was calculated using a person’s weight in kilograms divided by height in meters squared (BMI=kg/m2). Then, BMI was classified into three categories according to the Indonesian Ministry of Health: 1) Normal (18.5 to 25.0); 2) Underweight (≤17.0 to 18.4); 3) Overweight (25.1 to ≥27.0) (11).
Data collection methods
Data collection was carried out by distributing a Google Form link containing a self-reported questionnaire that was filled out voluntarily, anonymously, and with consent through social media such as WhatsApp and Line. Participants were required to log in to their email accounts to avoid duplicate data. Male and female pre-clinical medical students who have participated in online learning since it was enacted and had no history of mental illness were eligible to be included in this study.
Data analysis
All data were analyzed using SPSS version 26 (IBM, Chicago, IL, USA). Categorical data were displayed as frequency and percentage. Bivariate analysis using the Chi-Square test was conducted to compare the difference in proportions between groups. Multivariate logistic regression analysis to identify predictors for depression, anxiety, and stress was also carried out by including variables with a P-value <0.25 in the bivariate analysis. A P-value of <0.05 was considered statistically significant.
Results
Socio-demographic characteristics
Table 1 presents the socio-demographic characteristics of pre-clinical medical students. Of 483 FM UII pre-clinical medical students, 273 (response rate 56.52%) had filled out the questionnaire and were included in this study (27.1% male and 72.9% female). Most of them were ≥20 years old (63.7%) with a mean of 19.86 ± 1.07, were in their third year of study (39.2%), and had a normal BMI (64%) with a mean of 22.54 ± 4.27.
Table 2 presented pre-clinical medical students’ mental health status in five categories, including depression, anxiety, and stress levels. Their trends tend to decrease with higher severity. When displayed in two categories (mild to extremely severe) in Figure 1, more than a third of students suffer depression (35.2%) and stress (40.3%). Meanwhile, the prevalence of anxiety was slightly higher than normal (50.2%). Females have a higher prevalence of depression, anxiety, and stress than males.
As presented in Table 3, females were more prevalent to have depression significantly (P<0.05) than males. Whereas age, year of study, and BMI did not differ significantly in proportion. Being a female was 2.22 times more likely to suffer depression (95% CI: 1.19 to 4.15).
Bivariate analysis for anxiety-associated factors showed that females, aged≥20, in the third year of study, and have underweight BMI were statistically significant (P<0.05). Then, we adjusted those significant variables for multivariate analysis. The results showed that being female and underweight had higher odds of developing anxiety with AOR 2.56 (95%CI: 1.42 to 4.61) and AOR 2.81 (95% CI: 1.26 to 6.28) respectively. However, medical students in their second (AOR: 0.48; 95% CI: 0.23 to 0.98) and third years of study (AOR: 0.29; 95% CI: 0.13 to 0.67) were less likely to suffer anxiety compares to first-year students.
Evaluation for stress-associated factors with bivariate analysis found that stress was significantly (P<0.05) associated with being female, aged ≥ 20, and in the third year of study. After adjusting for gender, age, and year of study, only females (95% CI: 1.81 to 6.54) were 3.44 times more likely to have stress. Meanwhile, in the third year of the study (AOR: 0.38; 95% CI: 0.17 to 0.86) were less likely to have stress.
Table 1 presents the socio-demographic characteristics of pre-clinical medical students. Of 483 FM UII pre-clinical medical students, 273 (response rate 56.52%) had filled out the questionnaire and were included in this study (27.1% male and 72.9% female). Most of them were ≥20 years old (63.7%) with a mean of 19.86 ± 1.07, were in their third year of study (39.2%), and had a normal BMI (64%) with a mean of 22.54 ± 4.27.
Table 1. Descriptive of socio-demographic characteristics (N=273)
SD: standard deviation; BMI: body mass index.
Mental health status of pre-clinical medical students| Variables | N | % | |
| Gender | |||
| Male | 74 | 27.1 | |
| Female | 199 | 72.9 | |
| Age, mean ± SD | 19.86 ± 1.07 | ||
| < 20 | 99 | 36.3 | |
| ≥ 20 | 174 | 63.7 | |
| Year of Study | |||
| 1st | 70 | 25.6 | |
| 2nd | 96 | 35.2 | |
| 3rd | 107 | 39.2 | |
| BMI, mean ± SD | 22.54 ± 4.27 | ||
| Underweight | 36 | 13.2 | |
| Normal | 175 | 64.1 | |
| Overweight | 62 | 22.7 | |
Table 2 presented pre-clinical medical students’ mental health status in five categories, including depression, anxiety, and stress levels. Their trends tend to decrease with higher severity. When displayed in two categories (mild to extremely severe) in Figure 1, more than a third of students suffer depression (35.2%) and stress (40.3%). Meanwhile, the prevalence of anxiety was slightly higher than normal (50.2%). Females have a higher prevalence of depression, anxiety, and stress than males.
Table 2. Level of depression, anxiety, and stress among pre-clinical medical students
| Levels | Depression | Anxiety | Stress | |||
| N | % | N | % | N | % | |
| Normal | 177 | 64.8 | 136 | 49.8 | 163 | 59.7 |
| Mild | 44 | 16.1 | 39 | 14.3 | 45 | 16.5 |
| Moderate | 32 | 11.7 | 41 | 15.0 | 37 | 13.6 |
| Severe | 7 | 2.6 | 21 | 7.7 | 21 | 7.7 |
| Extremely severe | 13 | 4.8 | 36 | 13.2 | 7 | 2.6 |
**Depression scoring: normal (0-4), mild (5-6), moderate (7-10), severe (11-13), extremely severe (≥14)
*Anxiety scoring: normal (0-3), mild (4-5), moderate (6-7), severe (8-9), extremely severe (≥10)
*Stress scoring: normal (0-7), mild (8-9), moderate (10-12), severe (13-16), extremely severe (≥17)
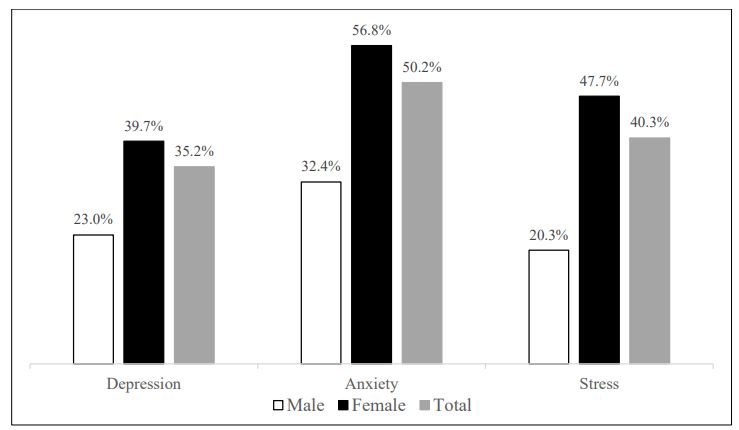
Figure 1. Prevalence of depression, anxiety, and stress among pre-clinical medical students (N=273)
Association between socio-demographic variables with depression, anxiety, and stress*Anxiety scoring: normal (0-3), mild (4-5), moderate (6-7), severe (8-9), extremely severe (≥10)
*Stress scoring: normal (0-7), mild (8-9), moderate (10-12), severe (13-16), extremely severe (≥17)
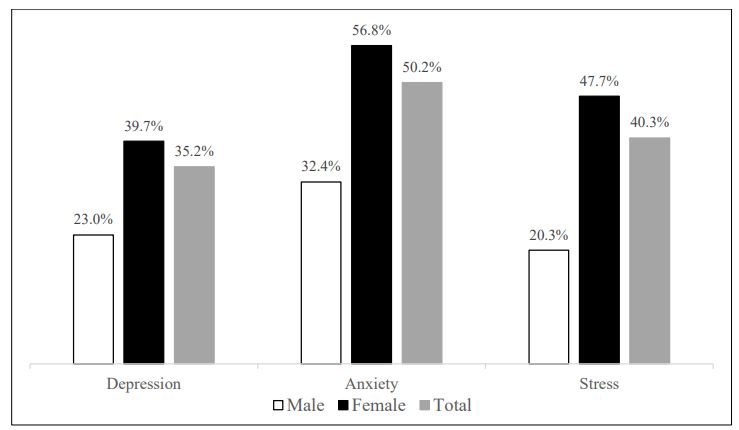
Figure 1. Prevalence of depression, anxiety, and stress among pre-clinical medical students (N=273)
As presented in Table 3, females were more prevalent to have depression significantly (P<0.05) than males. Whereas age, year of study, and BMI did not differ significantly in proportion. Being a female was 2.22 times more likely to suffer depression (95% CI: 1.19 to 4.15).
Bivariate analysis for anxiety-associated factors showed that females, aged≥20, in the third year of study, and have underweight BMI were statistically significant (P<0.05). Then, we adjusted those significant variables for multivariate analysis. The results showed that being female and underweight had higher odds of developing anxiety with AOR 2.56 (95%CI: 1.42 to 4.61) and AOR 2.81 (95% CI: 1.26 to 6.28) respectively. However, medical students in their second (AOR: 0.48; 95% CI: 0.23 to 0.98) and third years of study (AOR: 0.29; 95% CI: 0.13 to 0.67) were less likely to suffer anxiety compares to first-year students.
Evaluation for stress-associated factors with bivariate analysis found that stress was significantly (P<0.05) associated with being female, aged ≥ 20, and in the third year of study. After adjusting for gender, age, and year of study, only females (95% CI: 1.81 to 6.54) were 3.44 times more likely to have stress. Meanwhile, in the third year of the study (AOR: 0.38; 95% CI: 0.17 to 0.86) were less likely to have stress.
Table 3. Association between socio-demographic variables with depression, anxiety, and stress
| Variables | Depression, N (%) | OR (95% CI) | P-value | AOR (95% CI) | P-value | |
| Depressed | Normal | |||||
| Gender | ||||||
| Female | 79 (39.7) | 120 (60.3) | 2.21 (1.20 to 4.07) | 0.010 | 2.22 (1.19 to 4.15) | 0.013 |
| Male | 17 (23.0) | 57 (77.0) | Reference | Reference | ||
| Age | ||||||
| ≥ 20 | 62 (35.6) | 112 (64.4) | 1.06 (0.63 to 1.78) | 0.830 | ||
| < 20 | 34 (34.3) | 65 (65.7) | Reference | |||
| Year of study | ||||||
| 3rd | 34 (31.8) | 73 (68.2) | 0.59 (0.31 to 1.09) | 0.091 | 0.61 (0.32 to 1.16) | 0.132 |
| 2nd | 31 (32.3) | 65 (67.7) | 0.60 (0.32 to 1.13) | 0.115 | 0.57 (0.30 to 1.10) | 0.096 |
| 1st | 31 (44.3) | 39 (55.7) | Reference | Reference | ||
| BMI | ||||||
| Overweight | 26 (41.9) | 36 (58.1) | 1.62 (0.89 to 2.94) | 0.113 | 1.71 (0.93 to 3.16) | 0.086 |
| Underweight | 16 (44.4) | 20 (55.6) | 1.79 (0.86 to 3.73) | 0.115 | 1.81 (0.86 to 3.83) | 0.120 |
| Normal | 54 (30.9) | 121 (69.1) | Reference | Reference | ||
| Variables | Anxiety, N (%) | OR (95% CI) | P-value | AOR (95% CI) | P-value | |
| Anxious | Normal | |||||
| Gender | ||||||
| Female | 113 (56.8) | 86 (43.2) | 2.74 (1.56 to 4.80) | 0.000 | 2.56 (1.42 to 4.61) | 0.002 |
| Male | 24 (32.4) | 50 (67.6) | Reference | Reference | ||
| Age | ||||||
| ≥ 20 | 78 (44.8) | 96 (55.2) | 0.55 (0.33 to 0.91) | 0.019 | 1.02 (0.52 to 2.0) | 0.947 |
| < 20 | 59 (59.6) | 40 (40.4) | Reference | Reference | ||
| Year of study | ||||||
| 3rd | 40 (37.4) | 67 (62.6) | 0.29 (0.16 to 0.55) | 0.000 | 0.29 (0.13 to 0.67) | 0.003 |
| 2nd | 50 (52.1) | 46 (47.9) | 0.53 (0.28 to 1.01) | 0.052 | 0.48 (0.23 to 0.98) | 0.043 |
| 1st | 47 (67.1) | 23 (32.9) | Reference | Reference | ||
| BMI | ||||||
| Overweight | 32 (51.6) | 30 (48.4) | 1.27 (0.71 to 2.26) | 0.424 | 1.40 (0.76 to 2.59) | 0.278 |
| Underweight | 25 (69.4) | 11 (30.6) | 2.70 (1.25 to 5.82) | 0.010 | 2.81 (1.26 to 6.28) | 0.012 |
| Normal | 80 (45.7) | 95 (54.3) | Reference | Reference | ||
| Variables | Stress, N (%) | OR (95% CI) | P-value | AOR (95% CI) | P-value | |
| Stressed | Normal | |||||
| Gender | ||||||
| Female | 95 (47.7) | 104 (52.3) | 3.59 (1.91 to 6.76) | 0.000 | 3.44 (1.81 to 6.54) | 0.000 |
| Male | 15 (20.3) | 59 (79.7) | Reference | Reference | ||
| Age | ||||||
| ≥ 20 | 61 (35.1) | 113 (64.9) | 0.55 (0.33 to 0.91) | 0.019 | 0.95 (0.49 to 1.85) | 0.879 |
| < 20 | 49 (49.5) | 50 (50.5) | Reference | Reference | ||
| Year of study | ||||||
| 3rd | 32 (29.9) | 75 (70.1) | 0.34 (0.18 to 0.64) | 0.001 | 0.38 (0.17 to 0.87) | 0.021 |
| 2nd | 39 (40.6) | 57 (59.4) | 0.54 (0.29 to 1.01) | 0.054 | 0.53 (0.26 to 1.07) | 0.077 |
| 1st | 39 (55.7) | 31 (44.3) | Reference | Reference | ||
| BMI | ||||||
| Overweight | 22 (35.5) | 40 (64.5) | 0.79 (0.43 to 1.44) | 0.434 | ||
| Underweight | 16 (44.4) | 20 (55.6) | 1.14 (0.56 to 2.36) | 0.714 | ||
| Normal | 72 (41.1) | 103 (58.9) | Reference | |||
*Reference; Bold indicates statistically significant (P<0.05); OR: odds ratio; AOR: adjusted odds ratio; BMI: body mass index.
Discussion
Pre-clinical students, especially during the COVID-19 pandemic, are vulnerable to mental health distress. We have investigated the prevalence of symptoms of depression (35.2%), anxiety (50.2%), and stress (40.3%) in pre-clinical students during the first year of the COVID-19 pandemic using the DASS-21 questionnaire. Notably, this questionnaire cannot be used as a mental disorder diagnostic tool but can evaluate the prevalence of mental health in the population. Our results in depression, anxiety, and stress prevalence among pre-clinical medical students were higher than the general world population reported in a previous study conducted during the COVID-19 pandemic and a previous study conducted before the pandemic among university students (12,13). In addition, young people were reported to have worse mental distress than the elderly (14). Our findings indicate that a pre-clinical medical student at a young age is more likely to experience mental health distress and deteriorate during the pandemic. A cohort study in Switzerland by Elmer et al. (2020) proved that students’ mental health during the COVID-19 crisis, including depression, anxiety, stress, and loneliness, tended to deteriorate compared to before the crisis. These findings are associated with concerns about COVID-19, physical and social isolation, and a lack of interaction and emotional support (15).
In fact, many factors influence student mental health, resulting in various findings on the prevalence of depression, anxiety, and stress globally. For example, a study by Islam et al. (2020) on university students in Bangladesh reported that 82.4% and 87.7% of students had mild to severe depressive and anxiety symptoms, respectively (16). Furthermore, several factors such as feeling left behind from others in academics and living with a family are at risk of being more likely to suffer depression. Meanwhile, additional classes, concerns about academic activities, and living with a family will be more at risk of suffering anxiety. Another study by Ramón-Arbués et al. (2020) in Spain reported different results in the prevalence of depression (18.4%), anxiety (23.6%), and stress (34.5%) among university students as measured using the DASS-21 questionnaire. Furthermore, those aged <21 years, having problematic internet use, smoking, insomnia, and low self-esteem were more likely to suffer depression, anxiety, and stress (12). The different findings of these mental health studies may be explained by differences in inclusion criteria, internal factors (gender, perception, age, mental health history, and others), and external factors (residential environment, geographic location, socio-cultural, profession, and others).
Based on our study results, females have a higher prevalence and are more likely to experience depression, anxiety, and stress symptoms than males. Previous studies on university students in Egypt by Soltan et al. (2021) and Lebanon by Fawaz and Samaha (2020) during the COVID-19 pandemic reported similar results to our study (2,17). Possible reasons for impaired mental health in females appear to be influenced by several proposed potential factors, including high estrogen levels associated with depressive events, females tending to have a more expressive and feminine coping style, and gender differences in symptom phenotypes (18).
At our institution, FM UII, being a first-year student tends to be tiring and has many stressors because they are still in the adaptation phase to the new environment at the university, have tight academic schedules, and have to undergo a fairly long orientation period (>6 months). Although these activities are carried out online during the pandemic, this also takes a long time to spend more laptop screen time. In addition, they become less socially interactive directly with their colleagues. It is plausible that our findings suggest that being second and third-year students is a protective factor for anxiety, and only the third year is a protective factor for stress. The most likely reason is that second and third-year students have experienced offline lectures before the pandemic and are more likely to adapt to the physical and social environment than first-year students who have never experienced offline lectures.
Our study reported that the prevalence of abnormal BMI was 35.9%, comprising underweight 13.2% and overweight 22.7%. A possible reason during the quarantine period of the COVID-19 pandemic is that students tend to spend longer time living a sedentary lifestyle and eating more food, which leads to obesity (19, 20). They spend more time on laptops, smartphones, televisions, and others, resulting in an intense isolation effect that contributes to poor mental health (2). On the other hand, a study by Palmer et al. (2021) on university students in Germany reported a gain (27.5%) and loss (21.9%) of weight during the COVID-19 quarantine (21). Those who experienced weight gain were influenced by increased consumption of pasta, meat, sausages, sweets, cakes, and snacks, while weight loss was influenced by fruits and bakery product consumption.
In the current study, having an underweight BMI was also a predictor of being more likely to experience anxiety. Our findings are in line with Dejesus et al. (2016) that there is an increased prevalence of anxiety in people who have underweight and overweight BMI (22). However, a previous cohort study by Sahle et al. (2019) had different results, in which a history of anxiety was not associated with subsequent changes in BMI and vice versa. Possible reasons for these inconsistent findings are the different characteristics of participants and confounding variables that may be involved (23).
During the COVID-19 pandemic in 2020-2021, which was increasingly felt to be affecting mental health, several medical student organizations collaborated with the United Nations Children’s Fund (UNICEF), and universities held mental health webinars during the pandemic (24–26). However, after the COVID-19 pandemic conditions were declared under control in mid-2022 (27), such mental health webinars were as hard to find as before the pandemic period. Mental health awareness is still a big challenge, as reported in a previous study that the stigma in Indonesian society to sufferers of mental health problems is still lacking (28). In addition, seminars or workshops to provide and maintain good mental health among medical students who will enter the clinical stage likely have never been held.
To the best of our knowledge, the current study is the first to evaluate the mental health and associated factors among medical students during the first year of the COVID-19 pandemic in Indonesia. However, this study only evaluates pre-clinical students at one university and other factors potentially associated with mental health were not comprehensively evaluated due to fewer socio-demographic characteristics. This cross-sectional study was also only conducted at one time, so post-COVID-19 mental health needs to be evaluated in future studies. However, our result can be an illustration and reference for the post-COVID-19 period as well as for an unwanted condition that might affect pre-clinical students’ mental health in the future.
In fact, many factors influence student mental health, resulting in various findings on the prevalence of depression, anxiety, and stress globally. For example, a study by Islam et al. (2020) on university students in Bangladesh reported that 82.4% and 87.7% of students had mild to severe depressive and anxiety symptoms, respectively (16). Furthermore, several factors such as feeling left behind from others in academics and living with a family are at risk of being more likely to suffer depression. Meanwhile, additional classes, concerns about academic activities, and living with a family will be more at risk of suffering anxiety. Another study by Ramón-Arbués et al. (2020) in Spain reported different results in the prevalence of depression (18.4%), anxiety (23.6%), and stress (34.5%) among university students as measured using the DASS-21 questionnaire. Furthermore, those aged <21 years, having problematic internet use, smoking, insomnia, and low self-esteem were more likely to suffer depression, anxiety, and stress (12). The different findings of these mental health studies may be explained by differences in inclusion criteria, internal factors (gender, perception, age, mental health history, and others), and external factors (residential environment, geographic location, socio-cultural, profession, and others).
Based on our study results, females have a higher prevalence and are more likely to experience depression, anxiety, and stress symptoms than males. Previous studies on university students in Egypt by Soltan et al. (2021) and Lebanon by Fawaz and Samaha (2020) during the COVID-19 pandemic reported similar results to our study (2,17). Possible reasons for impaired mental health in females appear to be influenced by several proposed potential factors, including high estrogen levels associated with depressive events, females tending to have a more expressive and feminine coping style, and gender differences in symptom phenotypes (18).
At our institution, FM UII, being a first-year student tends to be tiring and has many stressors because they are still in the adaptation phase to the new environment at the university, have tight academic schedules, and have to undergo a fairly long orientation period (>6 months). Although these activities are carried out online during the pandemic, this also takes a long time to spend more laptop screen time. In addition, they become less socially interactive directly with their colleagues. It is plausible that our findings suggest that being second and third-year students is a protective factor for anxiety, and only the third year is a protective factor for stress. The most likely reason is that second and third-year students have experienced offline lectures before the pandemic and are more likely to adapt to the physical and social environment than first-year students who have never experienced offline lectures.
Our study reported that the prevalence of abnormal BMI was 35.9%, comprising underweight 13.2% and overweight 22.7%. A possible reason during the quarantine period of the COVID-19 pandemic is that students tend to spend longer time living a sedentary lifestyle and eating more food, which leads to obesity (19, 20). They spend more time on laptops, smartphones, televisions, and others, resulting in an intense isolation effect that contributes to poor mental health (2). On the other hand, a study by Palmer et al. (2021) on university students in Germany reported a gain (27.5%) and loss (21.9%) of weight during the COVID-19 quarantine (21). Those who experienced weight gain were influenced by increased consumption of pasta, meat, sausages, sweets, cakes, and snacks, while weight loss was influenced by fruits and bakery product consumption.
In the current study, having an underweight BMI was also a predictor of being more likely to experience anxiety. Our findings are in line with Dejesus et al. (2016) that there is an increased prevalence of anxiety in people who have underweight and overweight BMI (22). However, a previous cohort study by Sahle et al. (2019) had different results, in which a history of anxiety was not associated with subsequent changes in BMI and vice versa. Possible reasons for these inconsistent findings are the different characteristics of participants and confounding variables that may be involved (23).
During the COVID-19 pandemic in 2020-2021, which was increasingly felt to be affecting mental health, several medical student organizations collaborated with the United Nations Children’s Fund (UNICEF), and universities held mental health webinars during the pandemic (24–26). However, after the COVID-19 pandemic conditions were declared under control in mid-2022 (27), such mental health webinars were as hard to find as before the pandemic period. Mental health awareness is still a big challenge, as reported in a previous study that the stigma in Indonesian society to sufferers of mental health problems is still lacking (28). In addition, seminars or workshops to provide and maintain good mental health among medical students who will enter the clinical stage likely have never been held.
To the best of our knowledge, the current study is the first to evaluate the mental health and associated factors among medical students during the first year of the COVID-19 pandemic in Indonesia. However, this study only evaluates pre-clinical students at one university and other factors potentially associated with mental health were not comprehensively evaluated due to fewer socio-demographic characteristics. This cross-sectional study was also only conducted at one time, so post-COVID-19 mental health needs to be evaluated in future studies. However, our result can be an illustration and reference for the post-COVID-19 period as well as for an unwanted condition that might affect pre-clinical students’ mental health in the future.
Conclusion
This study reveals a high prevalence of depression, anxiety, and stress among pre-clinical students in Indonesia, with gender, year of study, and BMI as contributing factors. The study demonstrates that more than a third of the students suffered from depression and stress, while about half suffered from anxiety. In addition, females were more likely to experience depression, anxiety, and stress, whereas anxiety was less common in second and third-year students. Interestingly, being a third-year student was found to be a protective factor against stress. As a reflection, our study’s findings highlight the crucial need for intervention from educational institutions and policymakers to prepare effective strategies that prioritize pre-clinical students’ mental health and quality not only during the COVID-19 pandemic but also in any future situations that may impact students’ mental health. By doing so, educational institutions can ensure the development of a healthy and resilient cohort of medical professionals for the future.
Ethical considerations
All study protocols that met the ethical standards outlined in the International and National Guidelines were ethically approved by the Medical and Health Research Ethics Committee, Faculty of Medicine of Universitas Gadjah Mada, Yogyakarta, Indonesia (Number: KE/FK/0234/EC/2021). All participants were given and agreed to the informed consent online.
Acknowledgments
Ethical considerations
All study protocols that met the ethical standards outlined in the International and National Guidelines were ethically approved by the Medical and Health Research Ethics Committee, Faculty of Medicine of Universitas Gadjah Mada, Yogyakarta, Indonesia (Number: KE/FK/0234/EC/2021). All participants were given and agreed to the informed consent online.
Acknowledgments
The authors would like to thank the batch of medical students, namely Inxafar 2018, Rahtellza 2019, and Ashawarna 2020, that have been willing to fill out the questionnaire in this study.
Disclosure
The authors declare no conflict of interest and have not received any funds.
Author contributions
Disclosure
The authors declare no conflict of interest and have not received any funds.
Author contributions
Naufal Arif Ismail contributed to the conception and design of the study, conducted the study, provided study materials, collected, organized, analyzed, and interpreted data, and wrote the initial and final draft of the manuscript. Nur Aisyah Jamil contributed to the supervised, critically reviewed, and approved manuscript publishing, and she agrees to be accountable for the accuracy of the work.
Article Type : Orginal Research |
Subject:
Medical Sciences
Received: 2022/11/23 | Accepted: 2023/03/11 | Published: 2023/03/27
Received: 2022/11/23 | Accepted: 2023/03/11 | Published: 2023/03/27
References
1. Kemdikbud. Mendikbud Terbitkan SE tentang Pelaksanaan Pendidikan dalam Masa Darurat Covid-19 [Internet]. 2020 [cited 2020 Dec 27]. Available from: [Article]
2. Fawaz M, Samaha A. E‐learning: Depression, anxiety, and stress symptomatology among Lebanese university students during COVID‐19 quarantine. Nursing Forum. 2021;56(1):52–57. [DOI]
3. Hamaideh SH, Al‐Modallal H, Tanash M, et al. Depression, anxiety and stress among undergraduate students during COVID‐19 outbreak and “home‐quarantine.” Nursing Open. 2022;9(2):1423–1431. [DOI]
4. Seetan K, Al-Zubi M, Rubbai Y, et al. Impact of COVID-19 on medical students’ mental wellbeing in Jordan. Doering S, editor. PLOS ONE. 2021;16(6):e0253295. [DOI]
5. Pandey U, Corbett G, Mohan S, et al. Anxiety, Depression and Behavioural Changes in Junior Doctors and Medical Students Associated with the Coronavirus Pandemic: A Cross-Sectional Survey. The Journal of Obstetrics and Gynecology of India. 2021;71(1):33–37. [DOI]
6. Zeng W, Chen R, Wang X, et al. Prevalence of mental health problems among medical students in China: A meta-analysis. Medicine (United States). 2019;98(18). [DOI]
7. Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. [DOI]
8. Antony MM, Bieling PJ, Cox BJ, et al. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10(2):176–181. [DOI]
9. Oei TPS, Sawang S, Goh YW, et al. Using the Depression Anxiety Stress Scale 21 (DASS-21) across cultures. Vol. 48, International Journal of Psychology. Taylor & Francis; 2013. p. 1018–29. [DOI]
10. Onie S, Kirana AC, Adisya A, et al. Assessing the Predictive Validity and Reliability of the DASS-21, PHQ-9 and GAD-7 in an Indonesian Sample [Internet]. 2020. [Article] [DOI]
11. P2PTM Kemenkes RI. Tabel Batas Ambang indeks Massa tubuh (IMT) [Internet]. 2019 [cited 2022 Apr 3]. Available from: h [Article]
12. Ramón-Arbués E, Gea-Caballero V, Granada-López JM, et al. The prevalence of depression, anxiety and stress and their associated factors in college students. International Journal of Environmental Research and Public Health. 2020;17(19):1–15. [DOI]
13. Mahmud S, Mohsin M, Dewan MN, et al. The Global Prevalence of Depression, Anxiety, Stress, and Insomnia Among General Population During COVID-19 Pandemic: A Systematic Review and Meta-analysis. Trends in Psychology. 2022;31(1):143–70. [DOI]
14. Elvira SD, Lamuri A, Lukman PR, et al. Psychological distress among Greater Jakarta area residents during the COVID-19 pandemic and community containment. Heliyon. 2021;7(2):e06289. [DOI]
15. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. Capraro V, editor. PLOS ONE. 2020;15(7):e0236337. [DOI]
16. Islam MA, Barna SD, Raihan H, et al. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. Pakpour AH, editor. PLOS ONE. 2020;15(8):e0238162. [DOI]
17. Soltan MR, Soliman SS, Dawoud ME. A study of anxiety, depression and stress symptoms among Fayoum medical students during COVID-19 lockdown, Egypt. Egyptian Journal of Neurology, Psychiatry and Neurosurgery. 2021;57(1). [DOI]
18. Shi P, Yang A, Zhao Q, et al. A Hypothesis of Gender Differences in Self-Reporting Symptom of Depression: Implications to Solve Under-Diagnosis and Under-Treatment of Depression in Males. Frontiers in Psychiatry. 2021;12:6–8. [DOI]
19. He M, Xian Y, Lv X, et al. Changes in Body Weight, Physical Activity, and Lifestyle During the Semi-lockdown Period After the Outbreak of COVID-19 in China: An Online Survey. Disaster Medicine and Public Health Preparedness. 2021;15(2):e23–8. [DOI]
20. Pellegrini M, Ponzo V, Rosato R, et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7):1–11. [DOI]
21. Palmer K, Bschaden A, Stroebele-Benschop N. Changes in lifestyle, diet, and body weight during the first COVID 19 ‘lockdown’ in a student sample. Appetite. 2021;167:105638. [DOI]
22. DeJesus RS, Breitkopf CR, Ebbert JO, et al. Associations Between Anxiety Disorder Diagnoses and Body Mass Index Differ by Age, Sex and Race: A Population Based Study. Clinical Practice & Epidemiology in Mental Health. 2016;12(1):67–74. [DOI]
23. Sahle BW, Breslin M, Sanderson K, et al. Association between depression, anxiety and weight change in young adults. BMC Psychiatry. 2019;19(1):398. [DOI]
24. Universitas Airlangga. Webinar Kesehatan Mental “It’s Okay To Not Be Okay” [Internet]. 2020 [cited 2023 Feb 23]. Available from: [Article]
25. UNICEF Indonesia. It’s okay to not feel okay [Internet]. 2020 [cited 2023 Feb 23]. Available from: [Article]
26. UNICEF Indonesia. Young people take the lead on mental health [Internet]. 2020 [cited 2023 Feb 23]. Available from: [Article]
27. Kementerian Komunikasi dan Informatika Republik Indonesia. Presiden: Kondisi Covid-19 Masih Terkendali, Namun Tetap Waspada [Internet]. 2022 [cited 2023 Feb 23]. Available from: [Article]
28. Hartini N, Fardana NA, Ariana AD, et al. Stigma toward people with mental health problems in Indonesia. Psychology Research and Behavior Management. 2018;11:535–541. [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |